Research Article - (2025) Volume 33, Issue 1
Received: 28-Aug-2024, Manuscript No. IPQPC-24-21357; Editor assigned: 30-Aug-2024, Pre QC No. IPQPC-24-21357 (PQ); Reviewed: 13-Sep-2024, QC No. IPQPC-24-21357; Revised: 15-Jan-2025, Manuscript No. IPQPC-24-21357 (R); Published: 22-Jan-2025, DOI: 10.36648/1479-1064.33.1.57
Introduction: Pneumonia remains a leading cause of morbidity and mortality among children under five years old. Despite advancements in medical science, the disease remains a significant public health concern particularly in developing countries. This study aimed to assess the prevalence of pneumonia and its associated factors among under-five children at a tertiary hospital in Mogadishu, Somalia, to contribute to the formulation of effective intervention strategies.
Methods: A hospital-based, descriptive, cross-sectional study was conducted between February and June 2024. A sample size of 384 children was determined using the Cochran formula. Simple random sampling was used to select participants. Data were collected through face-to-face interviews with caregivers and review of medical records using a structured questionnaire adapted from validated sources. Data were analysed using SPSS software, employing descriptive statistics and bivariate analysis with chi-square tests. Variables with P<0.2 were included in a multivariable logistic regression model to adjust for confounders. A P<0.05 was considered statistically significant.
Results: Overall, data of 356 children under 5 years were analysed. The majority comprised children aged 1 month-1 year (n=121, 34.0%). The prevalence of pneumonia was 42.1%. Nearly half of the children had not been vaccinated, and aspiration incidents were reported in 19.9% of cases. Children of less than one month (AOR: 2.3, 95% CI: 1.59-3.58, p<0.1001), and those aged >1-2 years (AOR: 1.9, 95% CI: 1.31-2.74, p=0.001), >3-4 years (AOR: 1.9, 95% CI: 1.24-1.80, p=0.003), and >4-5 years (AOR: 1.9, 95% CI: 1.19-3.00, p=0.007) had a significantly higher risk of paediatric pneumonia. Furthermore, unvaccinated children (AOR: 0.8, 95% CI: 0.60-0.99, p=0.048), and allergic disease in the family (AOR: 0.7, 95% CI: 0.58-0.96, p=0.020) were significantly associated with paediatric pneumonia.
Conclusion: The study highlights the significant burden of pneumonia among children under five in Mogadishu and identifies key risk factors contributing to its prevalence. These findings underscore the urgent need for targeted public health interventions, including improved vaccination coverage, and enhanced caregiver education. Addressing these factors is crucial for reducing pneumonia-related morbidity and mortality in this vulnerable.
Prevalence; Pneumonia; Under five years old children
Pneumonia is a major global public health concern and a leading cause of illness and death among children under five years old [1]. Pneumonia is a leading cause of death among children worldwide, particularly in developing countries where access to clinical services is limited. Therefore, finding effective and low-cost alternatives is a global public health priority [2]. Pneumonia is an inflammatory condition affecting the lungs, encompassing the visceral pleura, connective tissue, airways, alveoli, and vascular structures [2]. Person with pneumonia, the alveoli become filled with pus and fluid, leading to painful breathing and reduced oxygen intake. Pneumonia can be caused by various agents, including viruses (such as rhinoviruses, Coronaviruses, influenza virus, respiratory syncytial virus, adenovirus, and parainfluenza), bacteria (such as Streptococcus pneumoniae, Chlamydophila pneumoniae, and Mycoplasma pneumoniae), and fungi. The bacterial pathogens Streptococcus pneumoniae and Haemophilus Influenzae type B (Hib) are the predominant causes of severe pneumonia among children in developing countries [3,4]. Pneumonia can be classified based on place of acquisition as community acquired or hospital acquired pneumonia. Pneumonia can be also classified based on the anatomy of the lungs involved as lobar pneumonia, bronchial pneumonia, or acute interstitial pneumonia. It can also be classified based on clinical severity as "no pneumonia," "pneumonia," or "severe pneumonia" [5,6]. The clinical manifestations of pneumonia in children include cough, difficulty breathing, rapid breathing, fever, and chest in drawing [2]. Children with a cough and cold but no signs of pneumonia were classified as having "no pneumonia," and their caregivers received advice on appropriate home care, children exhibiting fast breathing were classified as having "pneumonia" and were prescribed an oral antibiotic (oral cotrimoxazole at the time) to be taken at home for five days. Those with chest in drawing, with or without fast breathing, were classified as having "severe pneumonia" and were referred to the nearest health facility for treatment with injectable penicillin. Children showing any general danger signs were classified as having "severe pneumonia or very severe disease [7]. Children under the age of five are highly vulnerable to pneumonia [8], which remains the leading cause of morbidity and mortality in this age group [5]. Children can be protected from pneumonia through preventive measures such as routine pneumococcal vaccination, exclusive breastfeeding, and appropriate complementary feeding. Additionally, treatment strategies that focus on developing community capacity can significantly reduce pneumonia mortality in developing countries [2,9]. Despite the introduction of safe, effective, and affordable interventions that have reduced pneumonia-related deaths from 4 million in 1981 to just over one million in 2013, the disease still accounts for nearly 20% of all childhood fatalities worldwide [7]. Pneumococcal Conjugate Vaccines (PCV) have significantly reduced the incidence of Invasive Pneumococcal Disease (IPD) in children in the USA. Clinical trials have also demonstrated their effectiveness in African children, including those infected with HIV. Respiratory infections constitute 6% of the global disease burden. Each year, 6.6 million children under five die worldwide, with 95% of these deaths occurring in lowincome countries. For many of these nations, pneumonia represents the greatest challenge and the primary barrier to achieving the goal of reducing the child mortality rate to approximately 25 deaths per 1000 live births. Approximately 13 million children under 5 years of age die each year worldwide, One-third of these deaths are attributed to Acute Respiratory Infections (ARI). According to the World Health Organization (WHO), pneumonia accounts for 16% of deaths among children under five years old, primarily in developing countries. In 2017, pneumonia caused approximately 2,216 children dying from pneumonia every day that year. While another study globally, pneumonia is the leading infectious cause of death among children under the age of 5 years, claiming an estimated 2400 children's lives every day. The World Health Organization (WHO) estimated that annually, Acute Respiratory Infections (ARIs) excluding those caused by measles and pertussis, and neonatal deaths, resulted in 2.1 million deaths in children under the age of five. This accounts for approximately 20% of all childhood deaths. The incidence of pneumonia in children under the age of five is 0.29 episodes per child-year, resulting in approximately 151.8million cases annually in developing countries, with an additional 4 million cases in developed countries. Less than 2% of pneumonia-related deaths occur in the European Region, and less than 3% occur in the Region of the Americas [9]. Fifteen countries account for 74% of the world's annual pneumonia cases. Pneumonia is responsible for 15% of all deaths in children under the age of five globally, with 2% of these deaths occurring in newborns. The incidence of pneumonia among children under five decreased to 120 million cases (with 0.88 million deaths) in 2010 and further to 102 million cases (with 0.7 million deaths) globally by 2015 [8].
Globally, pneumonia is the primary cause of death among children under the age of five, and over 90% of these deaths occur in resource-limited settings. Globally, numerous research studies have been conducted to identify risk factors for pneumonia. Although findings have sometimes been inconsistent, factors such as low birth weight, malnutrition, indoor air pollution, parental smoking, lack of vaccination, overcrowding, absence of a separate kitchen, lack of exclusive breastfeeding, and low maternal education have been consistently identified as associated with the occurrence of pneumonia in children under five years old. UNICEF's statistics on child mortality reveal that each year, nearly 10.5 million children die before reaching their fifth birthday, amounting to approximately 30,000 children per day, half of these deaths among children under five can be directly attributed to five diseases: Pneumonia, diarrhoea, malaria, measles, and AIDS. In Bangladesh, severe pneumonia ranks as the primary cause of hospitalization among children under the age of five, from 2000 to 2014, global childhood pneumonia-related mortality decreased by 54%. Additionally, Bangladesh experienced a significant decline in annual pneumonia-related mortality after 2000, contributing to its progress toward achieving the millennium development goals/SDG.
The African region bears the highest burden of global child mortality, with 50% of worldwide deaths from pneumonia occurring in this age group in Africa. Pneumococcal disease is estimated to cause 826,000 deaths among young children in developing countries, with the majority of these deaths occurring in sub-Saharan Africa. Africa and South-East Asia collectively account for more than three-quarters of global pneumonia deaths in children under the age of 5 years. In sub-Saharan Africa, the estimated proportion of deaths in children under five years attributed to pneumonia ranges from 17% to 26%. Between 2000 and 2019, the global underfive children mortality rate decreased by approximately 50%. However, progress has been uneven, and as of now, 65 countries (32% of 204 countries) are not on track to achieve Sustainable Development Goal (SDG) 3.2 by 2030. Most of these countries are located in sub-Saharan Africa and South Asia, highlighting the challenges in reducing child mortality in these regions despite global improvements.
In East African countries, various researchers have investigated the prevalence of pneumonia in children under five years old. Their studies have reported a wide range of prevalence rates, from as low as 5.5% to as high as 89.8%. In East African countries, risk factors for pneumonia in children under five include low socioeconomic status, maternal education, lack of separate kitchens and ventilation, short breastfeeding duration, incomplete immunization, poor hygiene practices, limited awareness of pneumonia symptoms, overcrowding, indoor air pollution from charcoal use, and household behaviors like carrying children while cooking and environmental factors such as cockroach infestation and new furniture.
The save the children report from 2017 strongly correlates childhood pneumonia with poverty-related factors such as indoor and outdoor pollution, sanitation issues, inadequate access to safe drinking water, and challenges in accessing quality healthcare services.
Pneumonia continues to pose a significant burden in Asian and sub-Saharan countries. In Sub-Saharan Africa (SSA), there were 1,621 cases of pneumonia per 100,000 children as of 2018. In 2018, pneumonia-related deaths among children under five in sub-Saharan Africa included 162,000 deaths in Nigeria, 40,000 deaths in the Democratic Republic of Congo (DRC), 32,000 deaths in Ethiopia, 18,000 deaths in Chad, 16,000 deaths in Angola, 15,000 deaths in Tanzania, and 13,000 deaths in Niger. Pneumonia is the second leading cause of in-patient mortality among children under five in Uganda. Kenya is currently ranked among the 15 countries with the highest estimated number of deaths due to clinical pneumonia, with a mortality rate of 50.3 per 10,000 children under five per year. Pneumonia continues to be a significant health challenge affecting children in Somalia. In developing like Somalia According to the World Health Organization (WHO), pneumonia is the leading cause of death among children under five years old in Somalia, accounting for 15% of all deaths in this age group.
In Somalia, the incidence of pneumonia is also significant, with an estimated 400,000 cases reported annually, Save the Children in 2018, there were 15,165 deaths due to pneumonia in Somalia. In 2018, there were 122 deaths per 1,000 live births among children under five in Somalia due to pneumonia. Additionally, pneumonia accounted for 21% of all child deaths in Somalia that year. In 2017, pneumonia was identified as the leading cause of death among children under five in the country. UNICEF indicated that pneumonia killed 2 children every hour in Somalia in 2018. Pneumonia-related deaths among children under five in Somalia numbered 14,700 in 2015, 14,945 in 2016, 15,041 in 2017, and 15,165 in 2018. The situation in Somalia is dire, exacerbated by food shortages due to drought, which have left millions of children malnourished and highly susceptible to diseases such as pneumonia. More than 80% of the victims are children under two years old, many of whom have weakened immune systems due to malnutrition or inadequate breastfeeding, making them unable to effectively combat infections. Infants, particularly in their first weeks of life, are at the highest risk. Addressing pneumonia during this critical time is crucial to saving lives and improving child health outcomes in Somalia. Therefore, the aim of this study was to assess prevalence of pneumonia and its associated factors among under five years old children at tertiary hospital in Mogadishu Somali.
Problem Statement
Childhood pneumonia has been the most common cause of suffering worldwide among children under five, with developing countries shouldering the highest burden of pneumonia-related mortality and morbidity.
Pneumonia claims the lives of more than two children every hour in Somalia. In 2015, a total of 14,561 Somali children died due to pneumonia, highlighting its significant impact on child mortality in the country.
Current data indicates a significant gap in the understanding of pneumonia prevalence and its associated factors among children under five in Mogadishu, few numbers of comprehensive studies conducted. This knowledge gap impedes the development and implementation of targeted interventions and policies aimed at reducing pneumoniarelated morbidity and mortality. As a result, health disparities persist, adversely affecting child health outcomes in Mogadishu. Addressing this gap is crucial for improving public health strategies and ensuring better health for children in this region.
Study Design and Period
This study used a cross-sectional design to determine the prevalence of pneumonia and its associated factors among children under five years old at a tertiary hospital in Mogadishu, Somalia. The study was conducted over a period of five months, from Feb to June 2024.
Target Population
The study population included all children under five years’ old who were admitted or attended to the Paediatric Department of the Mogadishu Somali Türkiye Training and Research Hospital.
Study Setting
Mogadishu Somali Turkey Recep Tayyip Erdogan Training and Research Hospital, also known as Digfer Hospital, opened to the public in June 2015. The hospital's establishment followed a protocol signed in September 2013 between the health ministries of Somalia and Turkey, aimed at enhancing cooperation in health and medicine. The hospital is located on Digfeer Street in the Hodan district of Mogadishu, Somalia's capital. Positioned on the Eastern Coast of Africa along the Indian Ocean, Mogadishu is the country's largest city and serves as its economic, cultural, and political center. The hospital's strategic location in Mogadishu positions it at the forefront of addressing a wide range of public health challenges. It serves a diverse patient population, with a particular emphasis on providing specialized care, such as pediatric services, to children presenting with various medical conditions.
Sample and Sampling
Sample method: It is a simple random sampling method was employed to select respondents for the study, from whom data will be gathered.
Sample size determination: The sample size was calculated using the Cochran formula for prevalence studies:
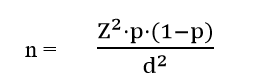
Where:
n=sample size.
Z=Z-value (1.96 for a 95% confidence level).
p=estimated prevalence of pneumonia (assumed to be 50% due to lack of prior data, which maximizes the sample size).
d=margin of error (5%).
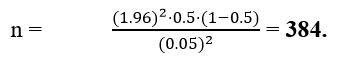
Plugging in the values:
Data Collection Method
Data were collected over a period of five months through face-to-face interviews with the child's caregiver and reviews of medical records. A structured questionnaire, administered by trained research assistants fluent in the Somali language, was used for data collection, with regular supervision to ensure quality. The collected data included socio-demographic characteristics such as the caregiver's age, gender, education level, and income, as well as the child's vaccination status.
Data Analysis
Data were entered and analysed using SPSS software. Descriptive statistics (frequencies, percentages, median, and interquartile range) were used to summarize the data. To identify factors associated with pneumonia, bivariate analysis was performed using chi-square tests for categorical variables. Unadjusted prevalence ratio (95% confidence interval) and Adjusted prevalence ratio (95% confidence interval).
Socio Demographic Characteristics of the Participants.
Overall, data of 356 children under 5 years were analysed. The majority comprised children aged 1 month-1 year (n=121, 34.0%). About 56.5% were male and only 66.3%(n=236) were delivered from the hospital. Nearly half of the children had not been vaccinated (n=171, 48.0%). Over 80% of the children were delivered at term, and aspiration incidents were reported in 19.9% of cases. Table 1 summarizes the sociodemographic characteristics of the children.
| Variable | Sub variable | Frequency | Percentage |
| Age | <1 month | 24 | 6.7 |
| 1 month-1 year | 121 | 34 | |
| >1-2 years | 90 | 25.3 | |
| >2-3 years | 41 | 11.5 | |
| >3-4 years | 49 | 13.8 | |
| >4-5 years | 31 | 8.7 | |
| Gender | Male | 201 | 56.5 |
| Female | 155 | 43.5 | |
| Place of delivery | Hospital | 236 | 66.3 |
| Home | 109 | 30.6 | |
| Others | 11 | 3.1 | |
| Birth weight, median (interquartile range), kilogram | 3 | 3-3 | |
| GA | Term | 295 | 82.9 |
| Pre-term | 61 | 17.1 | |
| Vaccinated | Yes | 185 | 52 |
| No | 171 | 48 | |
| Aspiration | Yes | 71 | 19.9 |
| No | 285 | 80.1 | |
| EBF time, median (interquartile range), days | 120 | 60-180 |
Table 1: Socio demographic characteristics of the participants.
Characteristics of the Parents/Caregivers to the Children
Table 2 summarizes the socio-demographic characteristics of the caregivers. The majority of the caregivers were above 20 years (n=255, 71.6%), and stayed in urban areas (n=255). About 20.5% of the caregivers had attained university education. The distribution of monthly family income showed that 11.5% of the caregivers earn less than $100 USD, 37.1% earn between $100 and $500 USD, and the majority (37.4%) earn between $501 and $1000 USD. Notably, 37.6% households had a smoker, with nearly half of the caregivers reporting allergic diseases in the family (n=175, 49.2%), and cases of tuberculosis reported by 32.3% of the caregivers. Most of the caregivers always use charcoal for cooking (n=148).
| Variable | Frequency | % | |
| Maternal age | <16 | 19 | 5.4 |
| 16-20 | 82 | 23 | |
| >20 | 255 | 71.6 | |
| Education | Illiterate | 94 | 26.4 |
| Literate | 82 | 23 | |
| Primary | 47 | 13.2 | |
| Intermediate | 28 | 7.9 | |
| Secondary | 32 | 8.9 | |
| University | 73 | 20.5 | |
| Where family live | Rural | 64 | 17.9 |
| Urban | 255 | 71.6 | |
| Rotative | 37 | 10.4 | |
| Number of people living in the house, median (interquartile range) | 5 | 4-7 | |
| Number of rooms in the house | 3 | 3-4 | |
| Monthly family income, USD | <100 | 41 | 11.5 |
| 100-500 | 132 | 37.1 | |
| 501-1000 | 133 | 37.4 | |
| >1000 | 50 | 14 | |
| Smoker in the house | No | 222 | 62.4 |
| Yes | 134 | 37.6 | |
| Allergic disease in family | No | 181 | 50.8 |
| Yes | 175 | 49.2 | |
| Tuberculosis disease in the family | No | 241 | 67.7 |
| Yes | 115 | 32.3 | |
| Source of fire | Charcoal | 158 | 44.4 |
| Gas | 164 | 46.1 | |
| Electric | 23 | 6.5 | |
| Wood | 9 | 2.5 | |
| Others | 2 | 0.6 | |
| Usage of charcoal during cooking | Always | 148 | 41.8 |
| Mostly | 56 | 15.8 | |
| Sometimes | 71 | 20.1 | |
| Rarely | 55 | 15.5 | |
| Never | 24 | 6.8 | |
Table 2: Characteristics of the parents to the participants.
Clinical Characteristics of the Children
About 42.1% of the children previously had pneumonia. Table 3 summarizes the clinical characteristics of the children with pneumonia. Remarkably, 47.8% of the children had been given antibiotics previously with the most commonly used antibiotic being ceftriaxone. The median duration of hospitalization was 3 days (interquartile range: 0 to 5 days). Over 70% of the children had fever, 60.1% had cough, 56.5%had Shortness of Breath (SOB), and 42.1% had chest retractions. Up to 37.4% had bilateral involvement on the chest X-ray, while 14.3% had a clear X-ray. At bivariate analysis (Table 4), factors associated with pneumonia among children under 5 years were, being a neonate (p <0.0001), age groups of >1-2 years (p<0.0001), >3-4 years (p=0.001), and >4-5 years (p=0.032). Furthermore, the child’s vaccination status (p=0.006), and allergic disease in the family (p=0.023) were other factors associated with pneumonia. At multivariable logistic regression (Table 5), neonates/<1 month (AOR: 2.3, 95% CI: 1.59-3.58, p<0.1001), >1-2 years (AOR: 1.9, 95% CI: 1.31-2.74, p=0.001), >3-4 years (AOR: 1.9, 95% CI: 1.24-1.80, p=0.003), and >4-5 years (AOR: 1.9, 95% CI: 1.19-3.00, p=0.007) significantly had higher risk of pediatric pneumonia. Also, un-vaccinated children (AOR: 0.8, 95% CI: 0.60-0.99, p=0.048), and allergic disease in the family (AOR: 0.7, 95% CI: 0.58-0.96, p=0.020) were less likely to have pediatric pneumonia.
| Variable | Sub variable | Frequency | % |
| Previous pneumonia | Yes | 150 | 42.1 |
| No | 206 | 57.9 | |
| Previous anti-biotic use | Yes | 170 | 47.8 |
| No | 186 | 52.3 | |
| If yes, which anti-biotic did you used | Alfasid | 56 | 32.9 |
| Ceftriaxone | 74 | 43.5 | |
| Macrolides | 33 | 19.4 | |
| Others | 7 | 4.1 | |
| Duration of hospitalization, median (interquartile range), days | 3 | 0-5 | |
| Hospital cost, median (interquartile range) | 100 | 50-150 | |
| Treatment type | IV | 110 | 30.9 |
| IM | 70 | 19.7 | |
| Others | 176 | 49.4 | |
| If there is any culture | Yes | 117 | 32.9 |
| No | 239 | 67.1 | |
| Previous hospitalization | Yes | 147 | 41.3 |
| No | 209 | 58.7 | |
| Fever | No | 103 | 28.9 |
| Yes | 253 | 71.1 | |
| Cough | No | 142 | 39.9 |
| Yes | 214 | 60.1 | |
| SOB | No | 154 | 43.5 |
| Yes | 200 | 56.5 | |
| Retraction | No | 206 | 57.9 |
| Yes | 150 | 42.1 | |
| X-rays findings | Lobar | 61 | 17.1 |
| 1 side | 47 | 13.2 | |
| 2 side | 133 | 37.4 | |
| Clear X-ray | 51 | 14.3 | |
| No X-ray | 64 | 18 | |
| WBC, median (interquartile range|), counts | 15 | 11-18 | |
| Neutrophil, median (interquartile range), counts | 7 | 05-10 | |
| Lymphocyte, median (interquartile range), counts | 4 | 3.7-6 | |
| CRP, median (interquartile range) | 30 | 12-53 | |
| Treatment | Intensive care unit | 74 | 20.8 |
| Clinic | 213 | 59.8 | |
| IM treatment | 53 | 14.9 | |
| Oral drugs | 16 | 4.5 | |
Table 3: Clinical characteristics of the children.
| Variable | Sub variable | Pneumonia | Unadjusted prevalence ratio (95% confidence interval) | P value | |
| No | No | ||||
| (n=206) n (%) | (n=206) n (%) | ||||
| Age | <1 month | 9 (4.4) | 15 (10.0) | 2.4 (1.54-3.63) | <0.0001 |
| 1 month-1 year | 89 (43.2) | 32 (21.3) | Reference | ||
| >1-2 years | 44 (21.4) | 46 (30.7) | 1.9 (1.35-2.77) | <0.0001 | |
| >2-3 years | 24 (11.7) | 46 (30.7) | 1.6 (0.98-2.51) | 0.061 | |
| >3-4 years | 23 (11.2) | 17 (11.3) | 2.01 (1.35-2.99) | 0.001 | |
| >4-5 years | 17 (8.3) | 26 (17.3) | 1.7 (1.04-2.79) | 0.032 | |
| Gender | Male | 119 (57.8) | 82 (54.7) | Reference | |
| Female | 87 (42.2) | 68 (45.3) | 1.08 (0.84-1.37) | 0.56 | |
| Place of delivery | Hospital | 135 (65.5) | 101 (67.3) | 1.6 (0.59-4.17) | 0.366 |
| Home | 63 (30.6) | 46 (30.7) | 1.5 (0.57-4.17) | 0.388 | |
| Others | 8 (3.9) | 3 (2.0) | Reference | ||
| GA | Term | 169 (82.0) | 126 (84.0) | Reference | |
| Pre-term | 37 (18.0) | 24 (16.0) | 0.9 (0.65-1.29) | 0.635 | |
| Vaccinated | Yes | 94 (45.6) | 91 (60.7) | Reference | |
| No | 112 (54.4) | 59 (39.3) | 0.7 (0.54-0.90) | 0.006 | |
| Aspiration | Yes | 38 (18.5) | 33 (22.0) | 1.1 (0.85-1.51) | 0.395 |
| no | 168 (81.5) | 117 (78.0) | Reference | ||
| Smoker in the house | No | 132 (64.1) | 90 (60.0) | Reference | |
| Yes | 74 (35.9) | 60 (40) | 1.1 (0.86-1.41) | 0.43 | |
| Allergic disease in family | No | 94 (45.6) | 87 (58.0) | Reference | |
| Yes | 112 (54.4) | 63 (42.0) | 0.7 (0.58-0.96) | 0.023 | |
| Tuberculosis disease in the family | No | 144 (69.9) | 97 (64.7) | Reference | |
| Yes | 62 (30.1) | 53 (35.3) | 1.1 (0.89-1.47) | 0.29 | |
| Source of fire | Charcoal | 93 (45.2) | 65 (43.3) | 1.6 (0.54-6.39) | 0.33 |
| Gas | 90 (43.7) | 74 (49.3) | 2.03 (0.59-6.98) | 0.261 | |
| Electric | 16 (7.8) | 7 (4.7) | 1.4 (0.35-5.40) | 0.653 | |
| Wood | 7 (3.4) | 2 (1.3) | Reference | ||
| Others | 0 (0) | 2 (1.3) | 4.5 (1.32-15.30) | 0.016 |
Table 4: Pneumonia risk factors in children.
| Variable | Sub variable | Adjusted prevalence ratio. (95% confidence interval) | P value |
| <1 month | 2.3 (1.59-3.58) | <0.001 | |
| 1 month-1 year | Reference | ||
| Age | >1-2 years | 1.9 (1.31-2.74) | 0.001 |
| >2-3 years | 1.5 (0.94-2.30) | 0.089 | |
| >3-4 years | 1.9 (1.24-1.80) | 0.003 | |
| >4-5 years | 1.9 (1.19-3.00) | 0.007 | |
| Vaccinated | Yes | Reference | |
| No | 0.8 (0.60-0.99) | 0.048 | |
| Allergic disease in family | No | Reference | |
| Yes | 0.7 (0.58-0.96) | 0.02 |
Table 5: Adjusted risk factors for paediatric pneumonia.
Socio Demographic Characteristics of the Participants:
The age distribution shows that the largest group consists of individuals aged 1 month to 1 year (34.0%), followed by those aged 1 to 2 years (25.3%). Infants younger than 1 month make up 6.7% of the population. There is a decreasing trend in older age groups: 2 to 3 years (11.5%), 3 to 4 years (13.8%), and 4 to 5 years (8.7%). in 2023 study done in Mogadishu in Banadir hospital shows majority of the children were 7 months-1 year at 42.6% followed by less than 6 months at 27.8%, implied that majority of the children with pneumonia case were 7 months-1 year when weaning is likely to begin. In 2020 in Northwest Ethiopia prevalence of pneumonia varied by age: 1 year olds: 25.8%, 2 year olds: 26.9%, 3 year olds: 22.9%, children aged 4 years and above: 24.5%. While similar study Uganda in 2019 that the age of the child (months) ≤ 11 40.0%, ≥ 12 60.0%. The distribution of gender in medical studies across different regions reveals notable variations. In Mogadishu's Banadir Hospital in 2023, males constituted 51.2% of respondents, slightly higher than females at 48.8%. This contrasts with findings from Northwest Ethiopia in 2020, where male children affected by pneumonia slightly outnumbered females, with percentages at 54.4% and 45.6%, respectively. In Uganda, a 2019 study showed a more significant disparity, with 60% of children diagnosed as male and 40% as female. Our study found that the median birth weight in the population is 3 kilograms, with an interquartile range of 3 to 3 kilograms, highlighting a high degree of consistency in birth weights. However, a 2023 study conducted at Banadir Hospital in Mogadishu reported different findings regarding birth weights. According to this study, the majority of newborns had birth weights between 1.1 and 2 kilograms, accounting for 57.4% of the births, followed by those weighing between 2.1 and 3 kilograms, making up 32.7% of the population. The median duration of Exclusive Breastfeeding (EBF) observed in our study, 120 days with an interquartile range of 60 to 180 days, underscores the variability in breastfeeding practices within our population. In Mogadishu, a 2023 study at Banadir Hospital revealed that 51.2% of infants received exclusive breastfeeding. A similar study in Uganda in 2019 reported that 80% of infants were breastfed for 12 months or longer, illustrating a potentially higher prevalence of extended breastfeeding practices compared to Mogadishu.
Characteristics of the Parents to the Participants
The distribution of maternal ages in our study shows that 5.4% of mothers are under 16 years old, 23.0% are between 16 and 20 years old, and the majority, 71.6%, are over 20 years old. In contrast, a study conducted in Northwest Ethiopia in 2020 reported a different distribution: 19.8% of mothers were younger than 25 years old, 25.0% were aged 25-27 years, 27.4% were aged 28-31 years, and 27.8% were aged 32 years and older. In our study, 26.4% of respondents are illiterate, and 23.0% are literate without specified educational levels. A 2023 study conducted at Banadir Hospital in Mogadishu reported that 41.4% of caregivers had not attended school, indicating a significant lack of basic education among many caregivers in that region. In our study, education levels vary with 13.2% completing primary education, 7.9% intermediate, 8.9% secondary, and 20.5% university education. In Uganda, 76% of mothers had primary education or less, while 24% had secondary education or higher. In Northwest Ethiopia, educational levels among mothers ranged from 17.0% unable to read/write to 23.3% with diploma or higher education, reflecting diverse educational backgrounds across regions. In our study, 71.6% of respondents live in urban areas, with 17.9% in rural areas and 10.4% in rotational living arrangements. In contrast, a 2019 study in Uganda found 28.0% urban and 72.0% rural residency, highlighting significant differences in urbanization between the two regions. Our study shows a varied income distribution among households: 11.5% earn less than $100 USD, 37.1% between $100 and $500 USD, 37.4% between $501 and $1000 USD, and 14.0% over $1000 USD monthly. In contrast, a 2023 study in Mogadishu found 58.0% of households earning less than $100 USD. In our study, 37.6% of households have smokers, while in a similar study in Uganda in 2019, only 15% of households reported smokers. In our study, charcoal emerged as a significant source of fire, utilized by 44.4% of households. This indicates a substantial reliance on charcoal for cooking, despite the availability of other options such as gas (46.1%) and electric (6.5%). Wood and other sources accounted for smaller percentages at 2.5% and 0.6% respectively. a similar study conducted in Uganda in 2019 demonstrated a markedly different pattern, with wood being the primary cooking fuel for 70% of households, and charcoal accounting for 30%. While in South West of Ethiopia charcoal was reported as the most common source of cooking fuel, utilized by 59.5% (182 households) of the surveyed population. Additionally, wood was utilized by 55.6% (170 households) of respondents for cooking purposes.
Clinical Characteristics of the Participants
In our study, 42.1% of respondents reported a history of previous pneumonia, while 57.9% had no prior occurrence. Comparatively, a 2023 study conducted at Banadir Hospital in Mogadishu reported a prevalence rate of 33% for pneumonia. Additionally, a study in Northwest Ethiopia in 2020 found a prevalence of 12% among children under five, with a 95% confidence interval. whereas a similar study in Uganda in 2019 reported a prevalence of 20% among children in the same age group. Based on the observed symptoms and X-ray findings, it is evident that the clinical presentation of the disease in this study cohort is characterized by a high prevalence of fever (71.1%), shortness of breath (56.5%), and retractions (42.1%). These findings underscore the significant burden of respiratory symptoms associated with the condition under investigation. Interestingly, our results contrast with those of a previous study conducted in the South West of Ethiopia, which reported a lower prevalence of cough (37.6%) during their survey period, this discrepancy could reflect regional variations in disease manifestation or differences in study populations and methodologies, Shortness of Breath (SOB) in 56.5%, and retractions in 42.1%. The X-ray findings reveal diverse patterns of pulmonary involvement, with bilateral involvement being the most common (37.4%). Lobar involvement was noted in a smaller proportion of cases (17.1%), while a substantial portion had either clear X-rays (14.3%) or no X-ray findings (18.0%). These radiographic findings highlight the heterogeneous nature of lung manifestations associated with the disease, ranging from localized to more diffuse patterns. While in thopia study shows the presence of cough, having difficulty of breathing, fast breathing, fever, and having chest in drawing were the identified clinical predictor for pneumonia among 2-59 month children in the current study.
Pneumonia Risk Factors in Children
Age: Compared to infants 1 month to 1 year, the unadjusted prevalence ratio for pneumonia was significantly higher under 1 month (neonate) and in children aged >1-2 years. The prevalence ratio was also higher in children aged >3-4 years and >4-5 years, but not statistically significant for children aged >2-3 years. While these findings align partially with a study conducted at Banadir Hospital in Mogadishu, which found that children aged 4-5 years had 1.125 times lower odds of pneumonia prevalence compared to those under 6 months of age (P=0.008). This discrepancy in the results for the 4-5 years’ age group between our study and the Banadir Hospital study could be due to differences in study design, population characteristics, or local healthcare practices. Additionally, a 2019 study from Uganda also reported a statistically significant association between the age of the child and the likelihood of developing pneumonia. This study highlighted that younger children are particularly vulnerable, supporting our findings of higher prevalence ratios in infants under 1 month and children aged over 1-2 years. In comparing these studies, a consistent pattern emerges, underscoring the heightened vulnerability of younger children to pneumonia. While our study and the Ugandan study both indicate a strong age-related risk for pneumonia, the Mogadishu study's specific finding of lower odds in the 4-5 years’ age group necessitates further investigation. It suggests potential regional or healthcare-related factors that could influence pneumonia prevalence and warrants a closer look at local healthcare interventions and socioeconomic conditions. Our study did not find a significant difference in the unadjusted prevalence ratio of pneumonia between males and females. This suggests that gender may not independently influence the risk of pneumonia among infants in our study population. Our study found no significant difference in the prevalence of pneumonia among infants delivered in hospitals or at home compared to other delivery settings. This suggests that the location of delivery may not independently influence pneumonia risk. In our study, we observed that preterm infants did not exhibit a significantly different unadjusted prevalence ratio of pneumonia compared to term infants. This finding aligns with the results from a study conducted at Banadir Hospital in Mogadishu, which reported a statistically significant association between preterm birth and the occurrence of pneumonia. Our study found that unvaccinated infants had a significantly lower unadjusted prevalence ratio of pneumonia compared to vaccinated infants. Similarly, a study at Banadir Hospital in Mogadishu identified a significant association between pneumonia vaccination and health outcomes. In our study, we did not observe significant differences in the unadjusted prevalence ratios of pneumonia associated with aspiration status, presence of a smoker in the household, family history of allergic disease, or family history of tuberculosis disease. These findings suggest that in our study population, these factors may not independently influence the risk of pneumonia among infants.
Conversely, a study conducted in Uganda in 2019 reported a significant association between the presence of a smoker in the household and pneumonia occurrence. The low p-value from their analysis indicates that exposure to household smoke constitutes a substantial risk factor for pneumonia in children. In contrast to our study, research conducted at Banadir Hospital in Mogadishu identified several factors significantly associated with pneumonia infection among children under 5 years old. Specifically, the level of education of the caretaker, level of income of the caretaker, birth weight, and exclusive breastfeeding were all found to be statistically significant predictors of pneumonia the presence of any smokers in the family was associated with a significantly increased odds ratio for pneumonia. These findings highlight the multifaceted nature of pneumonia risk factors, encompassing socio-economic, maternal health, and environmental influences. Our study did not find significant differences in the unadjusted prevalence ratios for pneumonia when comparing wood as the source of fire to charcoal, gas, or electric sources of fire. These results suggest that the type of fuel used for cooking or heating may not independently influence pneumonia risk in our study population.
To enhance pneumonia prevention, it is crucial to strengthen and expand vaccination programs to ensure higher coverage and protection, particularly focusing on children under one month and children aged 1-5 years who are most at risk. Healthcare interventions should prioritize these age groups, and efforts must be made to educate caregivers and communities on the importance of vaccination, proper nutrition, and early medical intervention for respiratory infections. Additionally, further research is necessary to explore additional risk factors and develop more comprehensive intervention strategies, addressing existing data gaps to improve overall prevention methods.
Limitation of Study
The study was conducted at a single center, which may limit the generalizability of the findings. The results may not be fully representative of the broader population, as the study sample was drawn from a specific hospital and geographical location. Further studies involving multiple centers would be needed to validate and generalize the findings across a wider population.
The study highlights the significant burden of pneumonia among children under five in Mogadishu and identifies key risk factors contributing to its prevalence. These findings underscore the urgent need for targeted public health interventions, including improved vaccination coverage, and enhanced caregiver education. Addressing these factors is crucial for reducing pneumonia-related morbidity and mortality in this vulnerable population.
The data used to support the results of the research are available from the corresponding author upon request.
Ethical approval for this study (Ethical Committee N° MSTH 10898) was provided by the Mogadishu Somali Türkiye Training and Research Hospital Ethical Committee, Mogadishu, Somalia, on 04 July 2022.
We would like to express our sincere gratitude to Dr. Yonis Abdullahi Ahmed Anshur for his invaluable guidance and insightful feedback throughout the research process. Special thanks to the Mogadishu Somali Türkiye Training and Research Hospital for providing the necessary resources and support. We also appreciate the contributions of our colleagues and the technical staff; whose expertise and assistance were crucial in completing this study. Finally, we extend our heartfelt thanks to our families for their unwavering support and encouragement.
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data, took part in drafting the article or revising it critically for important intellectual content, agreed to submit to the current journal, gave final approval to the version to be published, and agree to be accountable for all aspects of the work.
The authors received no financial support for the research, authorship and/or publication of this article.
The authors declare that there is no conflict of interest.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Roble MA, Anshur YAA, Qalif Y, Adan AM, Ahmed FH, et al. (2025) Prevalence of Pneumonia and Its Associated Factors among under Five Years Old Children at Tertiary Hospital in Mogadishu Somalia. Qual Prim Care. 33:57.
Copyright: © 2025 Roble MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.