Abeba Nigatie1*, Worku Belay2 and Girma Nega3
1Department of Nutrition, College of Medicine and Health Science, Bahir Dar University, Ethiopia
2Department of Orthopedic Surgeon, College of Medicine and Health Science, Bahir Dar University, Ethiopia
3Department of Applied Human Nutrition, College of Food Engineering, Bahir Dar University, Ethiopia
*Corresponding Author:
Abeba Nigatie
Professor
Department of Agricultural and Food Engineering
IIT Kharagpur, West Bengal, India
Tel: +251-0582-9 99275
E-mail: abebitpharma@yahoo.com
Received Date: October 26, 2017; Accepted Date: December 22, 2017; Published Date: December 29, 2017
Citation: Nigatie A, Belay W, Nega G (2017) Nutritional Status and Associated Factors among Adult Chronic Osteomyelitis Patients in Felege Hiwot Referral Hospital, Bahir Dar, North West Ethiopia. J Food Nutr Popul Health Vol.1 No.3:29
Keywords
Nutritional status; Malnutrition; Chronic osteomyelitis; Felege Hiwot referral Hospital
Introduction
Chronic osteomyelitis (COM) is a severe, persistent and sometimes incapacitating infection of bone and bone marrow. Globally, though there is limitation of evidences to show exact number of chronic osteomyelitis patients, it is becoming an emerging public health problem because of the increased incidence of high energy trauma. About 80% of chronic osteomyelitis results from contiguous spread from open wounds [1]. Development of infection may result from compromised soft tissue and bone vascularity, systemic compromise of the host and virulent or resistant organisms [2]. The pattern of chronic osteomyelitis distribution is similar to other infectious diseases, showing more noticeable dissemination in low income countries. Among individuals who have been treated for an episode of acute osteomyelitis, the prevalence of chronic osteomyelitis is about 5% to 25% in India, 15% in Gambia, 30% in Ethiopia.
Globally malnutrition is the most important risk factor for illness and death. It has been reported that malnutrition remains undiagnosed in up to 70% of hospital patients and about 70-80% of malnourished patients enter and leave the hospital without receiving any nutritional support and the diagnosis of malnutrition does not appear on their discharge sheet. Malnutrition in orthopedics patients is a condition that is overlooked and understudied, that have negative effects on outcomes.
Method
Study area
Institution based cross-sectional study was conducted to assess nutritional status and to determine associated factors of chronic osteomyelitis patients in Felege Hiwot Referal Hospital which is a referral level teaching hospital of college of medicine and health sciences-Bahir Dar University and has orthopedic department it is the only orthopedics specialty training department in Amhara national regional state. It gives four year orthopaedic residency training for medical doctors. It has over 50 beds and receives referred and some directly visiting patients from all over the country located approximately 578 km north-northwest of Addis Ababa-Ethiopia. Two diploma nurses and one orthopedics surgeon were recruited in data collection and clinical evaluation. A structured and pretested questionnaire was used to collect the data. The questioner was prepared in English and translated to local language “Amharic” and back to English by two language experts to check consistency. Pretest of the questionnaire was made on (5%) of the sample size in private hospital out of the main study area, two days training for data collectors and the supervisor on how to approach the respondents and how to conduct interview based on the objective of the study. In addition the filled questionnaires were also checked daily by the supervisor for completeness and missing data to maintain the data quality. The collected data were coded and entered into Epi info version 7 and analyzed using SPSS version 23. Descriptive statics (frequency, mean, median, standard deviation, range, and percentage) was used for sociodemography. Bivariate and multivariable logistic regression was used in order to identify predictive variables and odds ratio (OR) with 95% confidence interval and value was used as measure of the strength of association. Finally the variables which have significant association were identified on the basis of OR, 95% CI, and value <0.2 to identify eligible variables to fit into the final regression model and value < 0.05 was used to identify predictor variables.
Result
Socio-Demographic characteristics of chronic osteomyelitis patients
A total of 241 chronic osteomyelitis patients were included in the study and 238 responded which make the response rate 98.7%. Nearly two thirds of respondents were males 151(63.4%). The Mean (+s.d.) age of the respondents was 29(+12.0) years. More than half (51.2%) of the chronic osteomyelitis cases were reported among patients 18-27 years followed by those aged 28- 37 years at 22.6% (Table 1).
Table 1 Socio-Demographic characteristics of chronic osteomyelitis patients at Felege Hiwot Hospital, Bahir Dar, Ethiopia, May 2017, (n=238).
| Variable |
Number |
Percent |
| Age |
18-27 |
122 |
51.2 |
| 28-37 |
54 |
22.6 |
| 38-47 |
31 |
13 |
| ≥ 48 |
31 |
13 |
| Sex |
Male |
151 |
63.4 |
| Female |
87 |
36 |
| Ethnicity |
Amhara |
203 |
85.3 |
| Agew |
35 |
14.7 |
| Religion |
Orthodox |
232 |
97.5 |
| Muslim |
6 |
2.5 |
| Residence |
Rural |
221 |
92.8 |
| Urban |
17 |
7.1 |
| Marital status |
Single |
109 |
45.8 |
| Married |
120 |
50.4 |
| Divorced |
7 |
2.9 |
| widowed |
2 |
0.8 |
| Educational status |
Unable to read and write |
109 |
45.8 |
| Able to read and write |
15 |
6.3 |
| Grade 1-8 |
97 |
40.8 |
| Grade 9-12 |
13 |
5.5 |
| Diploma and above |
4 |
1.7 |
| Occupation |
Farmer |
190 |
79.8 |
| daily laborer |
24 |
10.1 |
| government employee |
10 |
4.2 |
| merchant |
14 |
5.9 |
| Availability of Latrine |
yes |
149 |
62.6 |
| no |
89 |
37.4 |
| Household |
≤ 900 |
15 |
6.3 |
| Monthly |
901-1200 |
89 |
37.4 |
| Income |
1201-1622 |
68 |
28.6 |
| ≥ 1623 |
66 |
27.6 |
Dietary intake related characteristics
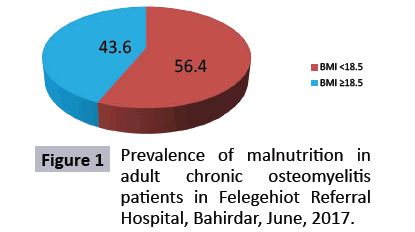
The study identified 54.1 % of respondents had meal frequency of less than three times per day. Large number of the study groups (56%) experienced loss of appetite which lasted for more than two weeks in the course of their illness. When the variety of meal is considered more than half (52.1%) of respondents eat less than three varieties of diet within 24 hours. Most of the respondents (97%) reported that they ate cereals within 24 hours. More than half (64%) of the patients did not get dietary counseling by health professionals in the whole duration of their treatment and follow up period (Figure 1).
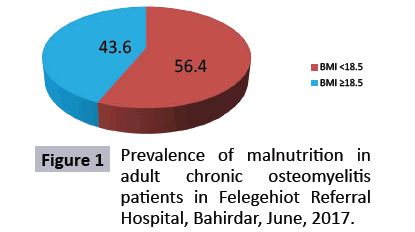
Figure 1: Prevalence of malnutrition in adult chronic osteomyelitis patients in Felegehiot Referral Hospital, Bahirdar, June, 2017.
Discussion
The main objective of the study was to determine prevalence of malnutrition and establish factors associated with malnutrition in chronic osteomyelitis patients. In this study males were more affected (63.4%) by chronic osteomyelitis, which is similar to a study conducted in Nigeria and blacklion Ethiopia. This could be because of the high involvement of young adult productive males in strenuous activities like farming and labour work which likely leads them to traumatic injuries. Rural residents were found to be highly affected by the disease (92%) this could be explained by the low socioeconomic status, lack of awareness because most of them do not have exposure to formal education (Table 2).
Table 2 logistic regression of malnutrition with predictor variables among chronic osteomyelitis patients FHRH Bahir Dar.
| Malnutrition (BMI<18.5) |
Crude OR 95% |
Adjusted OR 95%CI |
| |
Yes |
No |
| Sex |
| Male |
81 (53.6) |
70 (46.3) |
1 |
1 |
| Female |
53 (60.9) |
34 (39.0) |
1.347(.842,2.484) |
1,65(0.869,3.133) |
| Age |
| 18-27 |
78 (63.9) |
44 (36.0) |
1 |
1 |
| 28-37 |
28 (51.8) |
26 (48.2) |
1.646(.511,2.996) |
1,241(.38 ,4.05) |
| 38-47 |
13 (41.9) |
18 (58.1) |
0.407 (.324,2.384) |
0.829(0.23,2.93) |
| ≥48 |
15 (48.3) |
16 (51.7) |
1.298 (1.330,2.132) |
1.165(.230,5.907) |
| Monthly income |
| ≤ 900 |
8 (53.3) |
7(46.7) |
1 |
1 |
| 901-1200 |
56 (62.9) |
33(37.0) |
1.487 (0.387, 3.640) |
0.123 (0,01, 1.48) |
| 1201-1622 |
45 (66.1) |
23 (33.9) |
1.711 (0.441, 4.407) |
0.093 (0.009,0.995)* |
| ≥1623 |
25 (37.8) |
41 (62.2) |
0.533 (0.127, 1.281) |
0.125 (0.01, 1.92) |
| Disease stage |
| Stage1 |
8 (38.0) |
13 (62.0) |
1 |
1 |
| Stage 2 |
38 (50.0) |
38 (50.0) |
0.615 (0.131, 1.164) |
0.676 (0.19, 2.37) |
| Stage 3 |
63 (61.1) |
40 (38.9) |
0.390 (0.245,1.229) |
0.723 (0.29, 1.80) |
| Stage 4 |
25 (65.7 ) |
13 (34.3) |
0.320 (0.391,1.861) |
0.873 (0.36, 2.12) |
| loss of appetite |
| No |
38 (36.5) |
66 (63.5) |
1 |
1 |
| Yes |
100 (74.6) |
34 (25.4) |
5.108 (3.154, 9.691) |
2.224 (1.04, 4.78) |
| Disgusted because of wound |
| No |
11 (25.0) |
33 (75.0) |
1 |
1 |
| Yes |
123 (63.4) |
71 (36.6) |
5.197 (2.643, 11.690) |
0.261 (.06, 1.13) |
| MealFrequency per day |
| Three times |
84 (77.1) |
25 (22.9) |
1 |
1 |
| Twice |
44 (36.0) |
78 (64.0) |
0.188 (0.020, 1.929) |
0.143 (0.01, 2.10) |
| Once |
6 (85.7) |
1(14.3) |
2.0 (0.020, 1.929) |
1.258 ( 0.125, 12.68) |
| Varity of dietwithin 24 hours |
| ≥5 |
39 (34.2) |
75 (65.8) |
1 |
1 |
| <5 |
95 (76.6) |
29 (23.4) |
6.299 (3.743, 11.803) |
4.027 (2.14, 7.58) |
| food intake |
| Good |
20 (24.6) |
61 (75.4 ) |
1 |
1 |
| Poor |
114 (72.6) |
43 (27.4) |
8.086 (4.386,14.898) |
3.080 (1.485, 6.387) |
| Received dietary counseling |
| Yes |
34 (40.0) |
51 (60.0) |
1 |
1 |
| No |
100 (65.4) |
53 (34.6 ) |
2.830(1.65, 4.94) |
3.526 (1.43, 8.73) |
Nearly one fourth of patients involved in the study suffered from the disease for more than three years and further complicated by interventions done by traditional healers. This is similar with the Black lion study which reported 52% of COM patients visited traditional healers. Clear justification for this is poor access to hospitals, lack of trained manpower to provide modern treatment and on top of this the few high level professionals hardly get materials and instruments to undergo advanced operations [2].
When meal frequency and variety of diet is considered nearly half of the study population has frequency of less than three times and less than five verities of diet per day. Since the respondents are from cereal cultivating area so 97% of them eat cereals in a day in addition to this significant number of patients on treatment and follow up in the referral hospital setup didn’t get dietary counseling this is similar with study conducted in Addis. Females were more malnourished than males in in this study, may be possibly females tend) to give more attention to their family than taking care to themselves and to consume better food sources to maintain their nutrition [3]. Patients with duration of illness of more than three years were found to be malnourished than others. This could be explained by the disease itself that chronic illnesses lead to anemia of chronic illnesses, which is in line with the Black lion study [4].
In this study, the prevalence of malnutrition found in chronic osteomyelitis patients was 56.4% this is in line with a study conducted in orthopedic patients where malnutrition was found to be 55% and 55% in five referral hospitals in Amhara region- Ethiopia on traumatic injury patients.
The prevalence was much lower than a study done in Malawi 57%, Uganda 62% [5]. The difference may be due to variations in sample size, year of study and use of different parameters to determine prevalence of malnutrition.
A study in Danish hospital showed prevalence of malnutrition of 40% two Queensland hospitals (31% & 35%) and the Addis Ababa Black lion hospital study revealed 43% [6]. These studies showed lower prevalence than the result of this study. This difference could be due to residence, socioeconomic and cultural differences. This high proportion of malnutrition in the study area could be because of low socio economic status leading to lack of access to food resulting in malnutrition. Besides chronic illnesses and malnutrition augment one another in a vicious cycle manner and this could explain the fact that chronic osteomyelitis patients do not respond well for medical treatment and stay years before they get cured [7].
The study also show respondents with better house hold monthly income were less likely to be malnourished than those who have low house hold monthly income (95% CI: 0.009, 0.955) which is 92.7% protective from malnutrition. This finding is expressed similarly in a study done in New Zealand in which higher socioeconomic status had greater impact on diet selection [8]. Likewise in a study from US it was seen that household income affects the intakes of micronutrients where there was a difference of greater than 10% in the number of people meeting the nutrient requirements between the lowest and highest income categories [9]. The findings of this study revealed that the likelihood of being malnourished was found to be higher among patients who had loss of appetite as compared to those had no loss of appetite ( 95% CI: 1.04, 4.78). This is similar to a study done in Nigeria which explained the mimicry of pyogenic chronic osteomyelitis with malignancies. These patients may lose appetite because of the chronic disease or psycho social problems due to prolonged pus discharge from the affected area. In this study it is revealed that majority of the respondents have poor food intake and they are three times more likely to be malnourished than those having good food intake [AOR=3.080; 95% CI (1.485, 6.387)] .This is similarly described in a study conducted in Bangladesh where those having improved food intake were found to be well nourished than those with poor food intake [10]. This is clear from the fact that those having good food intake are likely to consume better diversified food in adequate quantity.
It is apparent from this study that patients who did not receive dietary counseling were 3.5 times more likely to be malnourished when compared to those who received dietary counseling (95% CI: 1.424, 8.73). This is consistent with a study done in a Canadian tertiary care university hospital in which malnutrition was found to be high, only two patients got dietary counseling [11]. Similarly a study in Addis Abeba showed patients who did not receive dietary counseling were 1.8 times more likely to be malnourished compared with those who received dietary counseling (95 % CI: 1.03, 3.12). This might be for the reason that those chronic osteomyelitis patients who have got dietary counseling became more aware of the dietary issues and they might apply the advices to take adequate quantity, quality and variety of foods.
According to findings of this research, there was no statistically significant association in between age, gender, disease staging, education status and occupation of respondents with their nutritional status.
Conclusions
In this study prevalence of malnutrition (BMI<18.5) among adult chronic osteomyelitis patients was 56.4% , which indicates that malnutrition is overlooked in the treatment and follow up of chronic osteomyelitis patients. As visualized clearly young productive adult farmers are more affected by the disease (73%) which could have deleterious impact on the family income and economic development of a country at large. Factors significantly associated with nutritional status include; house hold monthly income, loss of appetite and dietary counseling.
Recommendations
Based on this study finding we have recommended the following:
1. To policy makers Nutritional support as an integral part of the treatment protocol of chronic osteomyelitis should be considered.
2. To Felege Hiwot Referral hospital Attention needs to be given for nutrition aspect besides the medical and surgical treatment.
3. To health professionals Majority of patients in this study didn’t get dietary counseling and this was one of the most important factors which show statistically significant association to nutritional status, so it is recommended that treating health professionals should give dietary counseling for chronic osteomyelitis patients.
4. To researchers further study with a different study design is recommended to address other variables that were not included in this study.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Acknowledgments
The authors would like to thank and sincerely appreciate study participant, data collectors and Bahir Dar university orthopedics residents.
References
- Biruk WL, Wubshet K (2006)Chronic osteomyelitis at Tikur Anbessa hospital, Addis Ababa University, Ethiopia. East and Central African Journal of Surgery 1: 33-41.
- Ali N (2015) Chronic Osteomyelitis.
- Cierny G, Mader J (1989) Adult chronic osteomyelitis: an overview. In D'Ambrosia RD, Marier RL, editors. Orthopedic infections, Thorofare, NJ SLACK.
- Zalavras CG, Patzakis MJ (2003) Open Fractures: Evaluation and Management. Journal of the American Academy of Orthopedic Surgeons 11:212-219.
- USAID, IASC (2011) Harmonized training manual, introduction to nutrition and emergency.
- Zachariah R, Spielmann MP, Harries AD, Salaniponi FM (2002) Moderate to severe malnutrition in patients with tuberculosis is a risk factor associated with early death. Trans R Soc Trop Med Hyg 96:291-294.
- Omran M, Morley J (2000) Assessment of protein energy malnutrition in older persons, part I: History, examination, body composition, and screening tools. Nutrition 16:50-63.
- Willson J, Dougherty C, Ireland M, Davis I (2005) Core stability and its relationship to lower extremity function and injury. J Am AcadOrthop Surg 13: 316-325.
- Ensar A, Jelena P, Erol K (2015) Whole Body Vibration Training Effects on Bone Mineral Density in Postmenopausal Osteoporosis: A Review. Journal of Osteoporosis and Physical Activity 3: 150.
- Bouillet R, Bouillet B, Kadima N, Gillard J (1989) Treatment of chronic osteomyelitis in Africa with plaster implants impregnated with antibiotics. Acta Orthopaedica Belgica 55:1-11.
- Bickler S, Sanno-Duanda B (2000) Epidemiology of paediatric surgical admissions to a government referral hospital in Gambia. Bull World Health Organ 78:1330-1336.