- (2008) Volume 9, Issue 2
Rakesh Kalapala1, Lingareddy Sunitha2, Reddy D Nageshwar1, Guduru V Rao1, Sandeep Lakhtakia1, Manu Tandan1, Vijay B Nori2
1Department of Gastroenterology, Asian Institute of Gastroenterology;
2Department of Radiology, Lucid Medical Diagnostics. Hyderabad, Andhra Pradesh, India
Received December 26th, 2007 - Accepted, February 18th, 2007
The main pancreatic duct and the common bile duct can be evaluated with a variety of evolving invasive and non-invasive techniques. Virtual CT pancreatoscopy obtained using special computer software is a recent non-invasive innovation which shows the details of the ductal surface (endoluminal view) with greater precision. The use of special computer software in MRI in order to obtain pancreatic ductal surface details or a virtual MR pancreatoscopy has not been described up to now. We report a short series of four patients suffering from chronic pancreatitis who underwent virtual MR pancreatoscopy with an impact on their management and clinical outcome.
Cholangiopancreatography, Endoscopic Retrograde; Cholangiopancreatography, Magnetic Resonance; Lithotripsy; Pancreatic Ducts
Advances in computer technology have led to novel medical imaging techniques. Virtual endoscopic imaging is one such innovation, where the endoscopic details of a specified region in the human body can be generated by three dimensional reconstruction using computed tomography (CT) [1]. The key advantage of this “fly-through” technique of mucosal surface visual inspection is that the patient does not have to go through the rigor of regular invasive endoscopy. This innovation has proved itself in virtual colonoscopy [2], virtual upper GI endoscopy, virtual bronchoscopy [3] and virtual enteroscopy.
The main pancreatic duct and the common bile duct can be evaluated with a variety of evolving invasive and non-invasive techniques. Endoscopic retrograde cholangiopancreatography (ERCP) is an accurate but invasive procedure for imaging of the pancreatic duct and/or common bile duct. However, with its inherent associated potential complications, diagnostic ERCP has been replaced by magnetic resonance cholangiopancreatography (MRCP). Endoscopic ultrasonography (EUS) is an excellent investigative modality but has some disadvantages. It is a semi-invasive method and requires sedation. It also needs considerable expertise and may also over diagnose early chronic pancreatitis. Intraductal ultrasound (IDUS), using thin miniprobes, is currently the investigation of choice for evaluating fine pancreatic duct wall details.
A mother-and-baby pancreatoscope is another invasive procedure utilized for pancreatic or biliary ductal surface evaluation. Virtual CT pancreatoscopy, obtained using special computer software, is a recent non-invasive innovation which shows the details of ductal surface (endoluminal view) with greater precision. This has recently been used to differentiate intraductal papillary mucinous neoplasm (IPMN) from chronic pancreatitis [3].
The use of special computer software in MRI to obtain pancreatic ductal surface details or virtual MR pancreatoscopy has not been described up to now as a PubMed search has disclosed.
We report a short series of four patients suffering from chronic pancreatitis who underwent virtual MR pancreatoscopy with an impact on their management and clinical outcome.
3D MRCP was carried out on a 1.5T HDx GE MR (General Electric, Milwaukee, WI, USA) machine with the following parameters: TR- 3750, TE-74/EF, FOV-32x32, 256x256 matrix, NEX-0.75. A virtual pancreatoscopy was reconstructed and the images were obtained on an Advantage work station ADW 4.3 (General Electric, Milwaukee, WI, USA), using a navigation technique with a surface shaded display after adjusting the threshold values to attain maximum fluid intensity. The reconstruction was done by a radiologist. A higher matrix of 512x512 was also tried but it did not make any significant difference in the resolution of virtual reconstruction.
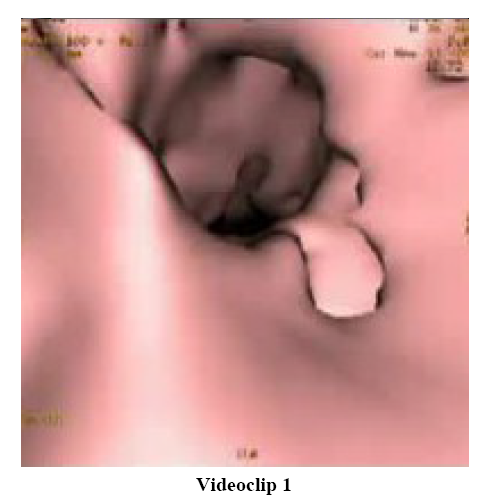
Case 1
A 35-year-old male patient presented with recurrent attacks of pancreatitis of three years duration. Imaging using transabdominal ultrasound and contrast-enhanced computerized tomography (CECT) confirmed changes of chronic pancreatitis with a dilated pancreatic duct. MRCP showed a grossly dilated main pancreatic duct (1.4 cm) with ectasia of the side branches (4-5 mm). Multiple intraductal filling defects of varying sizes (2-8 mm) were noted in the head of the pancreas. Virtual MR pancreatoscopy imaging demonstrated the side branch ectasia and a cluster of intraductal calculi in the region of the head. Extracorporeal shock wave lithotripsy (ESWL) followed by ERCP was performed with main pancreatic duct clearance and stenting (Figure 1; Videoclip 1).
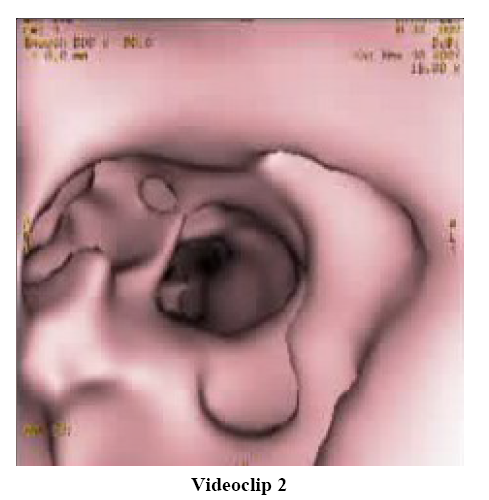
Case 2
A 28-year-old male patient presented with recurrent attacks of pancreatitis together with underlying chronic calcific pancreatitis. He had associated exocrine and endocrine insufficiency. CECT of the abdomen showed a narrowed main pancreatic duct in the head region with upstream ductal dilation. MRCP showed abrupt narrowing of the main pancreatic duct in the head region with a 10x9 mm hypointense filling defect. The rest of the pancreatic duct showed diffuse severe dilatation (20 mm) and side branch ectasia (10 mm). Virtual MR pancreatoscopy demonstrated a large oval calculus in the head. ESWL followed by ERCP was performed with main pancreatic duct clearance (Figure 2; Videoclip 2).
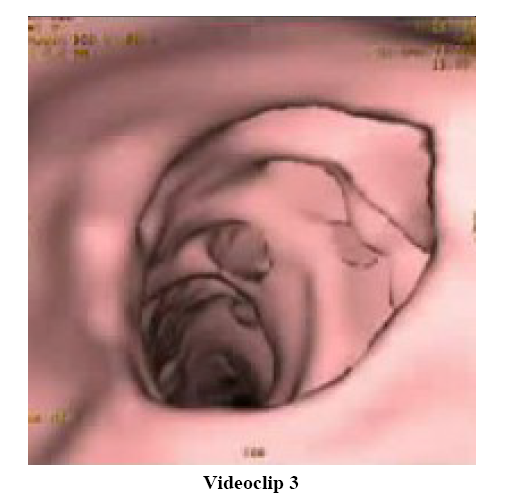
Case 3
A 34-year-old male patient presented with recurrent attacks of acute pancreatitis of one year duration. CECT of the abdomen showed evidence of chronic pancreatitis with intraductal calculi. MRCP showed severe cystic dilatation of the main pancreatic duct in the head and uncinate process with multiple intra-ductal filling defects (sizes: 5-18 mm). The rest of the duct in the body and tail region showed mild to moderate irregular dilatation (6-7 mm) and side branch ectasia (1-2 mm) with no obvious intra-ductal filling defects. Virtual MR pancreatoscopy showed smooth navigation in the dilated pancreatic duct. However, there was no clear demonstration of the calculus located at the genu of the main pancreatic duct. ERCP was done with pancreatic sphincterotomy and a partial clearance of the protein plugs (Figure 3; Videoclip 3).
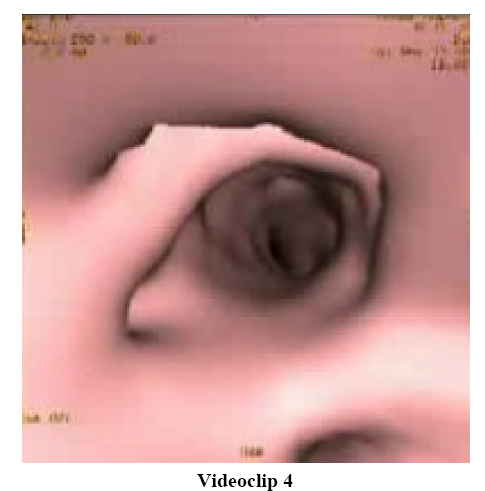
Case 4
A 32-year-old male patient with recurrent attacks of acute pancreatitis of 18 month duration had a space occupying lesion in the head region of the main pancreatic duct. CECT of the abdomen showed changes due to chronic pancreatitis. MRCP showed moderate dilatation of the main pancreatic duct (maximum diameter: 9 mm) with mild to moderate side branch ectasia (2-4 mm). There was an oval filling defect measuring 9x8 mm in the pancreatic duct in the region of the head. Virtual MR pancreatoscopy clearly showed side branch ectasia as well as the calculus. ERCP with sphincterotomy was followed by clearance of the head calculus (Figure 4; Videoclip 4).
Evaluation of the pancreatic duct and the common bile duct with ERCP is a wellestablished, but invasive, procedure. ERCP is dependent on operator skill and experience, along with associated procedure related complications, and its access time generally varies between 15 to 20 minutes. Virtual MR pancreatoscopy takes about 8-10 minutes for the acquisition of the sequences and another 5 minutes for reconstruction. EUS is a good investigative modality for chronic pancreatitis. However, EUS has certain disadvantages; it is a semi-invasive method and requires sedation. It also needs considerable expertise and may also over diagnose early chronic pancreatitis. Virtual CT pancreatoscopy is a recent non-invasive armamentarium in the evaluation of the pancreatic duct, especially in diagnosing mucin-producing pancreatic tumors [4] and IPMNs [5].
Virtual MR pancreatoscopy appears to be a feasible technique for endoluminal imaging of the pancreatic duct. This novel method provides an excellent internal surface display of the pancreatic duct which simulates “flythrough” endoscopy. This is an established technique for differentiating between IPMNs and chronic pancreatitis. The main pancreatic duct and its side branches are visualized with clarity displaying finer details. Although the dilatation of the main pancreatic duct and its side branches varied from mild to severe chronic pancreatitis, it did not hinder the resolution and finer surface detail on virtual imaging. The size and volume of the intraductal calculi can be calculated with reasonable precision which would help in follow-up cases of chronic pancreatitis after pancreatic endotherapy or ESWL.
The only problem encountered was in the visualization of calculi lodged at the normal angulation or genu along the course of the main pancreatic duct. It was difficult to navigate at the bends and turns of the main pancreatic duct as well as in the severe side branch ectasia in uncinate the process forming a cystic lesion. The artifacts which hinder visualization can be eliminated from an intraluminal view by modifying the threshold settings. However, this compromises accurate demonstration of the anatomy. The virtual images depicted the intra-luminal nature and shape of an impacted stone and abrupt obstruction or stenosis of the duct.
We present an analysis of an innovative technique carried out on a small sample size. We found that this technique is non-invasive, delineates the main pancreatic duct anatomy, mainly intra-luminal in greater detail, thus we can differentiate between calculi and protein plugs. There are no reports about this modality in the literature and we feel this will be add more information both as a diagnostic modality in chronic pancreatitis as well as deciding which patients would benefit from therapeutic ERCP (for small main pancreatic duct calculi extraction and ESWL followed by main pancreatic duct clearance in large calculi). This new imaging technique may provide a major role in delineating the intraluminal main pancreatic duct anatomy and hence a better therapeutic approach for endotherapy. However, further studies with a larger number of cases are needed in order to establish the efficacy of this technique in regular clinical practice as a diagnostic modality in the armamentarium of chronic pancreatitis.
Virtual MR pancreatoscopy is a new development of MRCP which allows endoluminal viewing of the dilated pancreatic duct and its side branches. Although this was evaluated in a small group of patients, the method appears promising, especially in evaluating patients with dilated pancreatic ducts. The cases presented here highlight MR pancreatoscopy as a reliable non-invasive option for the diagnosis of chronic pancreatitis. The results seen in current studies are encouraging, especially in the evaluation of a dilated pancreatic duct. However, future large volume comparative studies with EUS or other modalities will be required to validate these findings.
The authors have no potential conflicts of interest