- (2011) Volume 12, Issue 4
Nektaria Makrilia1, Kostas N Syrigos1, Muhammad W Saif2
1Oncology Unit, Third Department of Medicine, Sotiria General Hospital, Athens Medical School. Athens, Greece
2Columbia University College of Physicians and Surgeons and Pancreas Center, New York Presbyterian Hospital. New York, NY, USA
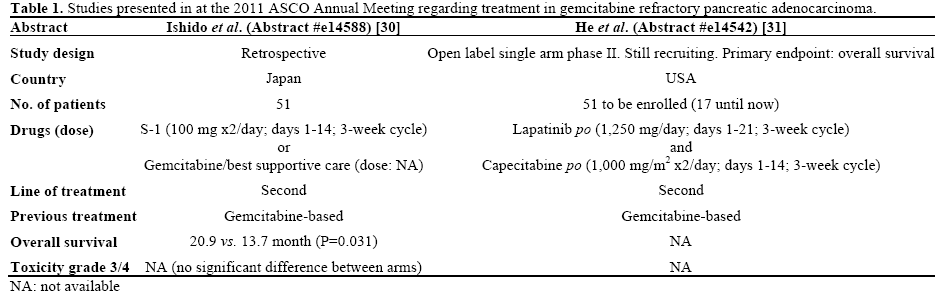
Gemcitabine monotherapy and gemcitabine-based regimens are the current standard of care for locally advanced or metastatic pancreatic adenocarcinoma. However, there is still great controversy over the role of salvage chemotherapy after failure of gemcitabine. This review is an update on the 2011 American Society of Clinical Oncology (ASCO) Annual Meeting regarding the most important developments in the treatment of refractory pancreatic cancer, as they were reported in Abstracts #e14542 and #e14588.
capecitabine; lapatinib; Pancreatic Neoplasms; S-1; Treatment Failure
ASCO: American Society of Clinical Oncology; FOLFIRI: irinotecan with 5-FU and folinic acid; FOLFOX: 5-FU plus folinic acid plus oxaliplatin; HER2: human epidermal growth factor receptor 2; TKI: tyrosine kinase inhibitor
Pancreatic cancer remains a malignancy of poor prognosis as overall survival has shown little improvement despite recent advances in therapeutics. With an estimated total of approximately 276,000 deaths in 2011 on a worldwide basis [1], pancreatic cancer constitutes a therapeutic challenge in current oncology practice. Gemcitabine monotherapy and its combination with erlotinib represent the current goldstandard treatment in advanced pancreatic adenocarcinoma with only modest benefit [2]. After failure of gemcitabine-based regimens, there are limited options available for second-line treatment, mainly because few large clinical trails have been conducted in this field [3]. Therefore, any new developments in this setting are of particular clinical interest.
Second-line chemotherapy offers better survival rates as compared to best supportive care, since Oettle et al. [4] showed benefit with the use of 5-FU/folinic acid/oxaliplatin (FOLFOX) as compared to offering best supportive care alone (median survival of secondline therapy: 21 vs. 10 weeks). In the landmark Charité Onkologie Clinical (CONKO)-003 trial, Pelzer et al. [5] demonstrated that the addition of oxaliplatin to 5- FU and leucovorin significantly improves overall survival and progression-free survival. Therefore, it is suggested that FOLFOX become the standard secondline treatment.
According to recent retrospective studies on taxanes, paclitaxel monotherapy shows mild efficacy with manageable toxicity in the second-line setting [6], as do docetaxel-based regimens [7]. Another agent also targeting microtubule dynamics, the halichondrin B analog eribulin mesylate, seems able to prolong stable disease with good tolerability [8]. Regarding irinotecan, Oh et al. [9] demonstrated that the combination of this agent with oxaliplatin offers a 50% disease control rate with a good toxicity profile. The combination of irinotecan with 5-FU and folinic acid (FOLFIRI) showed modest activity [10] in a randomized phase II study by Yoo et al. and these results were verified by a most recent retrospective study by Neuzillet et al. [11], with a 44.3% response rate. Ko et al. [12] showed that liposome irinotecan (PEP02), a nanoparticle formulation of irinotecan with better pharmacokinetics and tumor distribution, may also be a promising option for gemcitabine-refractory patients, offering a median progression-free survival of 9 weeks.
The efficacy of capecitabine in the second-line treatment of pancreatic adenocarcinoma has been explored in various combinations. Capecitabine monotherapy has been described as a safe option in an effort to prolong survival [13]. Its efficacy has been suggested to be correlated with thymidine phosphorylase and dihydropyrimidine dehydrogenase levels [14]. A 2008 phase II study showed that the combination of capecitabine plus oxaliplatin is active in patients with good performance status that have shown some response to first-line gemcitabine in the past (progression-free survival: 9.9 weeks) [15]. The clinical efficacy of this regimen was similar to that of the capecitabine-gemcitabine doublet in the Boeck et al. trial [16]. Combinations of capecitabine with celecoxib [17] or docetaxel [18] have also exhibited modest activity and tolerable toxicity after gemcitabine failure.
S-1 is an oral fluoropyrimidine that has been mostly investigated in Japanese populations (Figure 1). S-1 monotherapy has been mostly reported as well tolerated but only marginally effective in the secondline setting with moderate disease control rates [19, 20]. However, a most recent phase II study showed a relatively high disease control rate and marked decrease in tumor markers [21]. Combinations of S-1 plus irinotecan [22] or cisplatin [23] seem feasible with manageable toxicity warranting further investigation. Targeted therapies have also been evaluated in the second-line treatment, mostly with poor results. Monotherapy with sunitinib [24], everolimus [25], and bevacizumab [26] have shown inadequate antitumor activity, as have the combinations of bevacizumab with erlotinib [27] or docetaxel [26]. The combination of S- 1 with lapatinib has shown some promising activity in in vitro and in vivo studies [28]. Finally, erlotinib plus capecitabine seems to be a safe and active treatment option according to a phase II trial [29].
With regard to the treatment of gemcitabine-refractory pancreatic adenocarcinoma, two important abstracts were presented at the 2011 ASCO Annual Meeting (Table 1).
S-1 in Second-Line Therapy
Ishido et al. (Abstract #e14588) [30] conducted a retrospective study to evaluate the efficacy and safety of S-1 as second-line chemotherapy after failure of gemcitabine. The 51 enrolled patients were divided in two groups: those receiving S-1 monotherapy (26 patients) and those continuing to receive gemcitabine plus best supportive care (25 patients). There was a statistically significant difference between the two groups in overall survival (20.9 vs. 13.7 months; P=0.031) and in survival after relapse (11.7 vs. 6.0 months; P=0.0026), in favor of S-1 treatment. However, the researchers point out that in the S-1 group, survival was significantly prolonged in patients with local recurrences and not in other types of relapse (median overall survival: 26.9 vs. 17.8 months; P=0.046). Since there was no increased toxicity with the use of S-1, it is concluded that it is a safe and efficient therapeutic option for patients with gemcitabine-refractory pancreatic adenocarcinoma.
Capecitabine-Lapatinib
He et al. (Abstract #e14542) [31] describe a new open label single-arm phase II study that examines the use of the capecitabine-lapatinib doublet in the second-line therapy of pancreatic adenocarcinoma. Inclusion criteria are an adequate performance status (PS: 0-2), normal hepatic and renal function and failure after gemcitabine-based treatment. Patients will be administered lapatinib on a daily basis and capecitabine for the first two weeks of three-week cycles. In order to achieve a 90% power of statistical significance, the target is to enroll 51 patients over a period of 2 years. The study’s primary endpoint is median overall survival, while microRNA is also analyzed to examine its association with outcome. Since September 2009, 17 patients have been accrued and preliminary results suggest that the regimen is active and of tolerable toxicity.
To date, there is no established second-line treatment for patients who exhibit disease progression after gemcitabine-based treatment. Since pancreatic cancer progresses rapidly, patients are often of poor performance status after first-line treatment. Thus, maintaining quality of life is of utmost importance and should be seriously taken into account before proceeding to second-line of treatment. In an effort to address this subject, Kim et al. [32] tried to develop a prognostic model to identify patients who would benefit from second-line treatment. After retrospectively analyzing 90 patients, the researchers concluded that good performance status (PS: 0-1), response to first-line treatment and albumin levels of 3.5 mg/dL or greater were factors that could be used to select cases where second-line therapy would be beneficial.
To our knowledge, up to now, the largest studies evaluating S-1 monotherapy in the second-line setting were one retrospective study by Todaka et al. [19] and two phase II trials (Morizane et al. [20], Sudo et al. [21]). The recent results of the Ishido et al. [30] trial, reported at the 2011 ASCO Annual Meeting, show greater efficacy of S-1 as compared to the three previous studies. More specifically, in the Todaka et al. [19], Morizane et al. [20], and Sudo et al. [21] trials, progression-free survival reached 2.1 months, 2.0 months, and 4.1 months, respectively, while overall survival was reported as 5.8 months, 4.5 months, and 6.3 months, respectively. These reports differ significantly from the data presented in the Ishido et al. trial [30]: survival after relapse was 11.7 months with S-1 and overall survival was 20.9 months. These differences are probably attributed to the fact that patients of the Ishido et al. [30] trial had initially been diagnosed at resectable stage and had undergone surgery, as opposed to patients of the older trials who were diagnosed at advanced stages. It is important to note that patients’ performance status and disease control rates are not stated by Ishido et al. [30] and that the benefit in survival with S-1 was seen in patients with local recurrence and not other recurrence types. Based on the above, it is suggested that S-1 may be beneficial after gemcitabine-failure in certain subgroups of patients.
The combination of capecitabine with a tyrosine kinase (TKI) inhibitor has been studied in the past in the second-line setting after gemcitabine failure. Kulke et al. [29] administered capecitabine plus erlotinib to 30 patients and reported median survival of 6.5 months, with no apparent correlation between response and EGFR mutation status. As erlotinib has been shown to be active in the first-line treatment of pancreatic cancer, there has been growing interest in other growth factor TKIs, such as lapatinib, as well. Lapatinib is a dual TKI inhibitor of human epidermal growth factor receptor 2 (HER2) and epidermal growth factor receptor (EGFR) and since multiple HER pathways are often abnormal in pancreatic adenocarcinoma, lapatinib is expected to be more effective than a single EGFR inhibitor [33]. Regarding the He et al. study design [31], it is notable that patients of performance status equal to 2 are included, which will make this study very informative, since a great percentage of patients are of poor clinical status after gemcitabine failure. We should note that the lapatinib-capecitabine combination was most recently evaluated in the first-line treatment of metastatic pancreatic cancer with poor results, with no objective responses [34]. This could suggest inadequate efficacy of this doublet in the second-line setting as well but the initial results of the He et al. trial [31] show otherwise; therefore, the final results are awaited with great interest. Furthermore, it remains to be seen whether the trial reaches the goal of enrolling 51 patients over a period of 2 years, since only 17 patients have been accrued since September 2009.
In conclusion, despite advances in oncology research, the subject of selecting a second-line regimen after gemcitabine-failure remains controversial. Prospective randomized trials are expected to elucidate the role of novel agents and treatment combinations in selected patients with attention to toxicity.
None