- (2014) Volume 15, Issue 2
Namrata Sonia Chandhok, Muhammad Wasif Saif
Tufts University School of Medicine. Boston, MA, USA
Pancreatic cancer is an aggressive and devastating cancer that continues to have high 5-year mortality rates despiteadvancements in the field. Surgery remains the only curative treatment; however, most patients present with late stagedisease deemed unresectable. By refining the resection guidelines to include a borderline resectable group, as well asadvancements in neoadjuvant chemotherapy and radiation that improve resectability, we may improve upon outcomes forpatients with more invasive disease. Here we summarize and discuss findings presented at the 2014 ASCO GastrointestinalCancers Symposium (Abstracts #283, #302, #309, #274, #275, #327) that relate neoadjuvant therapeutic strategies andborderline resectable cancers.
Drug Therapy; General Surgery; Pancreatic Neoplasms; S 1 (combination)
FOLFIRINOX: oxaliplatin, irinotecan, fluorouracil, and leucovorin; hENT1: human equilibrative nucleoside transporter protein; mFOLFIRINOX: modified FOLFIRINOX; NCCN: National Comprehensive Cancer Network; SPARC: secreted protein acid and rich in cysteine
Pancreatic cancer is the 4th leading cause of cancer deaths in both men and women with a 5-year survival rate of 6%. In the United States, it is estimated that the number of new cases of pancreatic cancer in 2013 was 45,220 (2.7% of all new cancer diagnoses) and the estimated deaths from pancreatic cancer were 38,460 that accounts for 6.6% of all cancer deaths [1]. The poor prognosis of the disease is attributable to limited symptoms leading to late diagnosis of the disease and limited therapeutic options with advanced disease. To date, surgery has been the mainstay of treatment for pancreatic cancer, and the only potential cure; however, fewer than 20% of patients present with resectable disease at the time of diagnosis [2].
By redefining locally advanced non metastatic disease into borderline resectable disease and non resectable disease a new patient population that was previously considered to have unresectable disease stands to benefit. The use of chemotherapy and radiation for the treatment of micrometastatic disease, as well as downstaging of disease to resectable status, may have a profound impact on overall disease survival, particularly in borderline resectable disease. Neoadjuvant therapy has previously been shown to improve resectability of tumors previously thought to be unresectable leading to a similar survival rate as patients that were resectable at the time of diagnosis [3].
Per the current National Comprehensive Cancer Network (NCCN) guidelines [4], borderline resectable tumors are defined by the following criteria:
1. No distant metastases;
2. Venous involvement of the superior mesenteric/portal vein with localized narrowing or obstruction of the vessel but preserved vasculature proximal and distal to tumor allowing for safe resection;
3. Encasement of the gastroduodenal artery up to the hepatic artery with either short segment encasement or direct abutment of the hepatic artery, without extension to the celiac axis;
4. Tumor abutment of the superior mesenteric artery not to exceed greater than 180 degrees of the circumference of the vessel wall.
Based on the prior staging system that grouped all locally advanced tumors in the same category, this staging system helps classify a group that may benefit the most from adjuvant therapy in terms of overall resectability, but it is not without flaws. For example, the NCCN guidelines for tumor classification are based on radiologic evidence. There is evidence demonstrating that tumor response to neoadjuvant therapy is not radiographically reflected, even though resectability improves [5]. Efforts are being made to further define borderline criteria with more patient related factor, particularly to help guide duration and choice of neoadjuvant therapy [6].
In addition, an unclear classification system to group patients diagnosed with pancreatic cancer and course of treatment is further complicated by the lack of data on effective adjuvant therapies in resectable/borderline disease. Historically gemcitabine was the primary chemotherapeutic agent used. Recent data have shown that gemcitabine based combination therapies are superior to gemcitabine alone [7]. Several new agents, such as the use of S-1, a novel oral dihydropyrimidine dehydrogenase inhibitory fluoropyrimidine that is a biochemical modulation of 5-fluorouracil (discussed in the Abstracts below) are being tested as a part of combination therapy. Additionally, alternate regimens such as the use of a chemotherapy regimen consisting of oxaliplatin, irinotecan, fluorouracil, and leucovorin (FOLFIRINOX) have come to light. Conroy et al. demonstrated that in patients with metastatic cancer FOLFIRINOX provided a survival advantage, but had a greater toxicity [8]. Updates on this novel regimen in borderline resectable patients were also presented at the 2014 ASCO Gastrointestinal Cancers Symposium and they are presented below.
Multiple aspects of neoadjuvant therapies for borderline pancreatic cancer were explored at the 2014 ASCO Gastrointestinal Cancers Symposium. The role of various chemotherapeutic chemoradiotherapy regimens in improving disease resectability was the most unifiable theme in studies with varied endpoints; however, progression free survival and overall survival of patients with borderline pancreatic cancer were also evaluated. Results from Abstracts #283 [9], #302 [10], #309 [11], #274 [12], #275 [13], #327 [14] are summarized in Table 1.
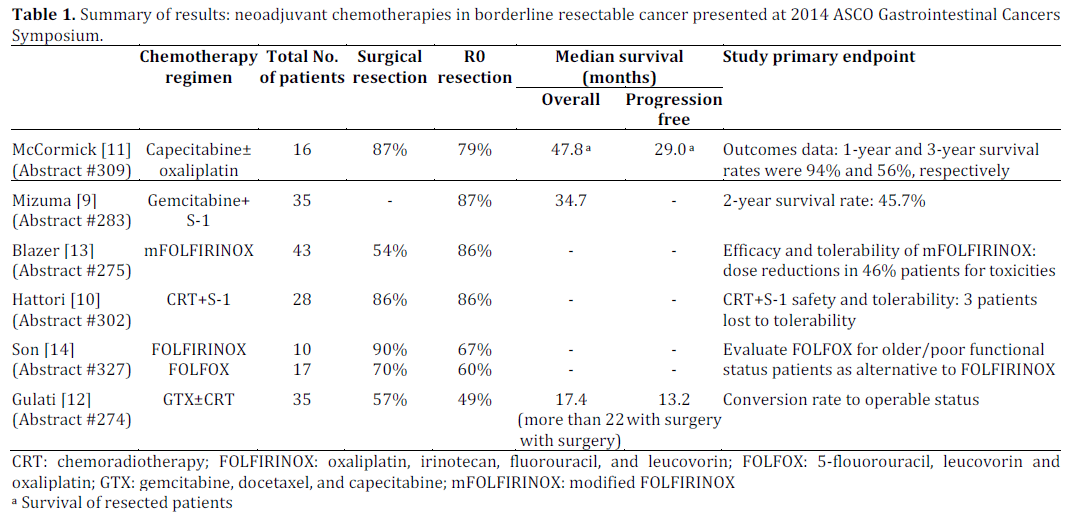
Based on the above data, a few conclusions were drawn. The results of all the studies seem to be in agreement that implementation of neoadjuvent therapy improves resectability of tumors that may improve overall survival. The data is promising; however, given the limited sample size, subjective variability and lack of a singular study group (i.e., a study limited to only borderline resectable patients), no definitive conclusions may be drawn. For example, Abstracts #309 [11] and #283 [9] explored outcomes for resectable and borderline resectable disease collectively, that may contribute to falsely improved outcomes given the inclusion of lower grade disease. Abstract #275 [13] studied modified FOLFIRINOX (mFOLFIRINOX) in patients with borderline resectable, as well as locally advanced unresectable pancreatic cancer [13]. As an initial step toward improved data collection, efforts must be made clarify the definition of the various stages of pancreatic cancer and address the known discrepancies between radiologic data and true resectability. Use of alternate methods to evaluate tumor status would provide an alternate avenue for evaluation. Abstracts #283 [9] addressed the use of CA 19-9 and Abstracts #302 [10] and #327 [14] addressed pathologic evaluation to assess disease status; however, no standard practice was established.
Multiple chemotherapeutic options, such as the ones described in the abstracts above, are currently being tested as alternatives. As a genetically complex disease, it is unlikely that all pancreatic cancer will respond equally to the chemotherapeutic options available. Therefore, genetic information will be necessary to tailor treatment to patient disease. For example, human equilibrative nucleoside transporter protein (hENT1) may help guide the use of gemcitabine based combination therapies as hENT1-low cells have been shown to be resistant to gemcitabine [15] and numerous studies have confirmed hENT1 tumor expression is predictive of gemcitabine response [16, 17, 18]. Similarly data has shown that dysregulation of secreted protein acid and rich in cysteine (SPARC), in peritumoral fibroblasts correlates with a poor prognosis in resectable pancreatic cancer although the mechanism is unclear [19] and loss of SPARC is associated with local spread and metastasis of tumors in mouse models [20]. Targeting specific tumor markers associated with poor prognosis may provide alternate methods to address tumor aggressiveness, study design and chemotherapeutic regimens to improve outcomes.
The abstracts presented were also primarily single arm studies with no clear control arms and generally reflect a single institution experience. Therefore, these abstracts provide good preliminary data on efficacy of particular drug regimens, but we cannot extrapolate the efficacy of a particular regimen against another. Therefore, no guideline for selection of a chemotherapeutic regimen and how it may relate to patient outcome has been established. Similarly, the utility of radiation therapy in addition to chemotherapy is not clear from these data given the lack of controls and subjective selection of participants, as well as follow up course if tumor resection was not considered the primary endpoint.
Despite advances in research, much remains to be understood in the field of pancreatic cancer. The reviews presented at the 2014 ASCO Gastrointestinal Cancers Symposium demonstrate the utility of neoadjuvant/adjuvant chemotherapy as a standard of treatment in both resectable and borderline resectable pancreatic cancers with respect to survival benefit; however, more data are needed to clarify regimens that provide a true survival benefit.
The authors have no potential conflict of interest