- (2010) Volume 11, Issue 2
Joshua Richter, Muhammad Wasif Saif
Yale University School of Medicine, New Haven, CT, USA
Pancreatic cancer represents the 4th leading cause of cancer deaths in the United States. Surgical resection remains the only potential curative approach. However, given the notion of a high recurrence rate, adjuvant therapy is needed to offset this risk. The 2010 American Society of Oncology Gastrointestinal Cancers Symposium offered new insights into optimized approaches towards adjuvant therapy of pancreatic cancer. Abstracts focusing on the role of targeted therapy utilizing erlotinib or GI-4000 in combination with gemcitabine (Abstracts #224 and #229) were presented. Subbiah, et al. presented a retrospective analysis comparing systemic chemotherapy versus chemoradiotherapy (Abstract #230) in the adjuvant setting. In addition, a data driven prediction tool to help predict which patients would be able to complete a course of adjuvant therapy in order to select out those who may alternative approaches (Abstract #236) was also presented. The authors summarize these findings presented at the 2010 ASCO Gastrointestinal Cancers Symposium, January 22-24, 2010, Orlando, FL, USA.
Chemotherapy, Adjuvant; Combined Modality Therapy; erlotinib; gemcitabine; Pancreatic Neoplasms
CONKO: Charité Onkologie; EORTC: European Organization for Research and Treatment of Cancer; MUC-1: mucin 1; NCCN: National Comprehensive Cancer Network; VACCR: Veterans Affairs Central Cancer Registry
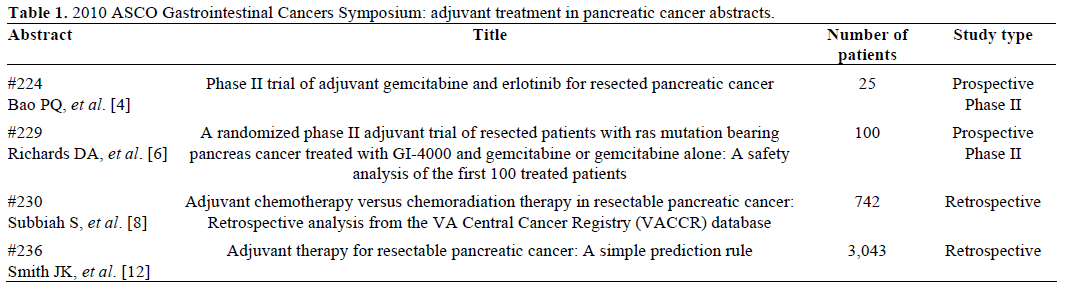
The American Cancer Society estimated that approximately 42,470 new cases of pancreatic cancer were diagnosed in the United States in 2009 with 35,240 deaths [1]. Of these new cases only 15-20% of these are classified as resectable disease; with only one-fifth of those patients surviving 5 years [2]. There continues to be a need for improvement in adjuvant therapy for those patients who are candidates for initial surgical resection. Results from the Charité Onkologie (CONKO-001) trial have shown that adjuvant chemotherapy with gemcitabine confers about a 6- month improvement in median disease-free survival in patients with R0 and R1 resections. However; there was no statistically significant improvement in overall survival between the gemcitabine and the observation groups [3]. This paper summarizes the recent work presented at the 2010 Gastric Cancers Symposium regarding advances in the adjuvant treatment setting of pancreatic cancer (Table 1).
Update in Adjuvant Treatment in Pancreatic Cancer
Abstract #224: Phase II trial of adjuvant gemcitabine and erlotinib for resected pancreatic cancer [4]
Gemcitabine has emerged as a popular chemotherapeutic agent in the treatment of pancreatic cancer. In the metastatic setting the addition of erlotinib to gemcitabine has yielded a small but significant improvement in median overall survival [5]. The authors of this abstract have conducted a phase II prospective trial to evaluate the role of this combination in the adjuvant setting.
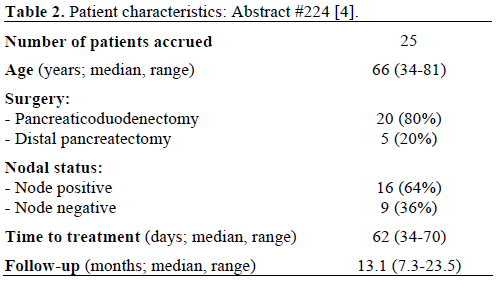
Twenty-five patients with margin-negative resections were treated with gemcitabine 1,500 mg/m2 biweekly for four months with concomitant erlotinib 150 mg daily for a total of 12 months. Therapy was to be initiated within 10 weeks of surgery. The primary endpoint of the study was to evaluate the effect of therapy on time to radiographic recurrence. The patient characteristics are reported in Table 2.
Fourteen of the 25 patients (56.0%) experienced recurrence of disease. Of those 14 patients:
• 9 recurred during treatment;
• 4 recurred after completing the planned course of therapy; and
• 1 recurred after being taken off protocol.
The recurrence free survival was 21.5 months (95% confidence interval: 7.6-24.5 months). Although the median overall survival was not reached; the estimated 1- and 2-year overall survival was 82% and 61%, respectively.
Overall, the combination of the two agents was tolerated moderately well with approximately 1/3 of patients requiring a dose reduction and/or dose holding of one or both drugs during treatment.
Abstract # 229: A randomized phase II adjuvant trial of resected patients with ras mutation bearing pancreas cancer treated with GI-4000 and gemcitabine or gemcitabine alone: A safety analysis of the first 100 treated patients [6]
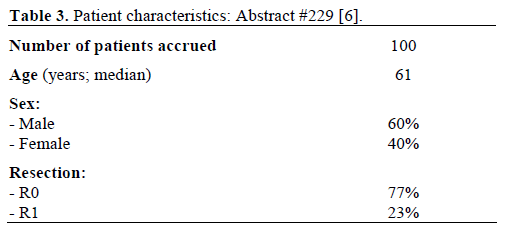
K-ras oncogene mutations have been identified in up to 95% of pancreatic cancers, implying their critical role in their molecular pathogenesis. Various studies have identified a wide prevalence and location of these mutations; however several loci (such as codon 12) may be associated with a particular tendency towards oncogenesis [7]. To further exploit this target the authors of this article have utilized GI-4000 which is a yeast-based (Saccharomyces cerevisiae) vaccine system that is designed to stimulate “killer” T cells in the immune system to find and destroy diseased cells. They have combined this novel agent with gemcitabine as an adjuvant treatment strategy for patients with resected pancreatic cancer. Their study focused on the safety analysis of this regimen. The patient characteristics are reported in Table 3.
Eligibility requirements for the study include patients with an R0 or R1 resection of a pancreatic neoplasm which contained a K-ras oncogene mutation associated with one of the mutants expressed in GI-4000. After successful pancreas cancer surgery, patient tumor specimens were assessed by DNA sequencing to identify whether the tumor contains a K-ras mutation contained in GI-4000. All patients received treatment with 6 cycles of gemcitabine 1,000 mg/m2 weekly x3 out of 4 week cycle. Patients were randomized to GI- 4000 or placebo to be administered weekly x3 prior to chemotherapy, monthly concomitantly with chemotherapy and monthly thereafter until death, recurrence or termination of therapy due to intolerance.
The median exposure to GI-4000 was 11 doses in this cohort. The safety data revealed 35 deaths and 2 discontinuations secondary to adverse events. Major serious adverse events included intra-abdominal abscess and intestinal obstruction. More common adverse events included fatigue, abdominal pain, anemia and neutropenia. Based on this initial safety analysis with acceptable adverse events the cohort has been expanded to 200 patients.
Abstract # 230: Adjuvant chemotherapy versus chemoradiation therapy in resectable pancreatic cancer: Retrospective analysis from the VA Central Cancer Registry (VACCR) database [8]
There is no universally accepted standard approach to treat patients with pancreatic cancer in the adjuvant setting. This controversy derives from several studies, each fraught with its own limitations. Standards of care also vary depending on which side of the Atlantic you are on: chemo-radiotherapy followed by chemotherapy is considered the optimal therapy in North America (Gastrointestinal Tumor Study Group: GITSG; European Organization for Research and Treatment of Cancer: EORTC; Radiation Therapy Oncology Group; RTOG 9704) while chemotherapy alone is the current standard in Europe (European Study Group for Pancreatic Cancer: ESPAC-1, ESPAC-3; CONKO). The EORTC utilized a 5-fluorouracil based chemoradiotherapy strategy and found an improvement in median survival from 19 to 24.5 months; however this was not statistically significant (P=0.208) [9]. The ESPAC-1 trial by Neoptolemos et al. actually found a detriment to survival in the chemoradiotherapy arm [10]. As there still remains some controversy; the National Comprehensive Cancer Network (NCCN) guidelines for the management of pancreatic cancer still allow for the use of adjuvant chemoradiotherapy [11].
In an effort to further elucidate this question, the authors of this paper analyzed retrospective data from the Veterans Affairs Central Cancer Registry (VACCR) database regarding patients with resected pancreatic cancer. The treatment modalities are reported in Table 4.
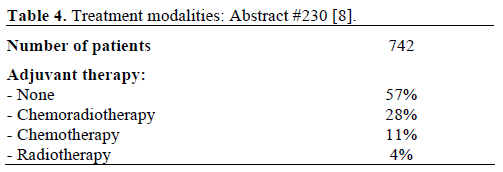
The cohort for this study was collected from patients in the VACCR database from 1995-2007. The majority of patients received either no adjuvant therapy or treatment with chemoradiotherapy. Both the chemotherapy and the chemoradiotherapy arms yielded an improvement in median survival when compared to those who received either no adjuvant therapy or radiation alone. The radiotherapy alone arm yielded the lowest median survival.
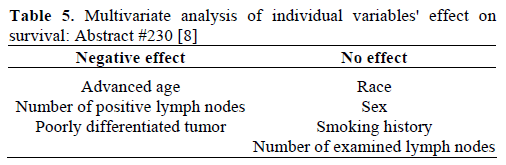
A multivariate analysis was conducted to evaluate the effect of differing factors on the survival statistic. The statistically significant results are displayed in Table 5. The chemotherapy arm was associated with a superior overall survival at 1 year at 63%. However, the chemoradiotherapy arm showed superior overall survival at the 1, 3 and 5 year marks with 72%, 28%, and 19%, respectively. The data suggest a benefit to treating pancreatic cancer with adjuvant therapy; however further prospective studies are needed to tease out exactly what approach is best for each individual patient.
Abstract # 236: Adjuvant therapy for resectable pancreatic cancer: A simple prediction rule [12]
Despite adequate R0/R1 resections for pancreatic cancer there remains a high recurrence rate in patients with macroscopically completely resected tumors. Although the optimal adjuvant therapy is not clearly defined; what is clear is that there is a need for therapy beyond surgical resection. Although regimens such as gemcitabine monotherapy are generally well tolerated, there are a substantial number of patients, for one reason or another, who will be unable to complete a course of adjuvant chemotherapy. If at presentation (upfront/prior to surgery) we knew which patients would be unable to complete adjuvant therapy we would need to do something else to reduce this risk. The authors of this abstract sought to create a prediction model to help define that subset.
Patients were identified through the Surveillance, Epidemiology, and End Result (SEER) and Medicare linked databases and selected out for age less than 65 years with pancreatic cancer resection between 1991 and 2007.
Of the 3,043 patients identified using this tool 80% were used to generate the data and the remaining 20% were used to validate it. The prediction tool takes into account a variety of factors including age, sex, surgery type, as well as comorbidities as calculated by the Charlson comorbidity score. The prediction tool generated a c statistic of 0.62 for the validation set, which translates into a fair predictive value. This tool can help predict those who may not be able to complete a significant course of adjuvant therapy and who should be selected out for alternative approaches for tumor recurrence risk reduction.
The optimal adjuvant approach for patients with resected pancreatic cancer remains elusive. The NCCN guidelines offer a variety of approaches including systemic chemotherapy with agents such as gemcitabine, 5-fluorouracil, capecitabine or gemcitabine followed by 5-fluorouracil based chemoradiotherapy [11]. The NCCN maintains that the best management for any cancer patient is enrollment in a clinical trial.
Intensive research is currently being conducted looking at vaccine strategies in a variety of solid and liquid tumors. Several groups have been evaluating the role of a mucin 1 (MUC-1) based vaccine in the adjuvant setting [13, 14]. MUC-1 is a tumor associated antigen which has been shown to be overexpressed in pancreatic adenocarcinoma. This vaccine approach focuses on the induction of an endogenous T-cell response which may confer a role in both the active therapeutic as well as the preventative setting. It represents an ideal approach in the adjuvant setting where the patient is either disease free or possesses minimal residual disease.
While these approaches offer some degree of benefit, as we enter into an age of “personalized medicine” we need to push the mantra of “the right approach for the right patient!”. A certain approach in a K-ras mutated patient may not be correct in the age-matched K-ras wild type. In the R0 resection setting cure is the goal and we can do better still. It is also important to underline the importance on developing as well as considering neoadjuvant therapy (chemo-radiotherapy or chemotherapy) in this setting. This approach can lead to improved survival, down-staging marginal lesions, sparing patients with rapidly progressive disease unnecessary surgery, and eliminate potential treatment delays that may be associated with adjuvant therapy [15].
The authors have no potential conflicts of interest