Fili S*, Schilde T, Perdikakis G and Kohlhaas M
Department of Ophthalmology, St.-Johannes-Hospital, Johannesstrasse, Dortmund, Germany
*Corresponding Author:
Fili S
Department of Ophthalmology
St.-Johannes-Hospital, Johannesstrasse
Dortmund, Germany
Tel: 004915206428718
E-mail: sofiafili86@hotmail.com
Received date: December 25, 2015; Accepted date: March 10, 2016; Published date: March 14, 2016
Citation: Fili S, Schilde T, Perdikakis G, Kohlhaas M, (2016) Two Cases of Keratomycosis Caused by Fusarium Solani: Therapeutic Management. J Eye Cataract Surg 2:9. doi: 10.21767/2471-8300.10009
Copyright: © 2016, Fili S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Fusarium keratitis; Keratoplasty à chaud; Multiresistance; Natamycin
Abbreviations
EUCAST: European Committee on Antimicrobial susceptibility Testing; MIC: Minimum Inhibitory Concentration
Introduction
Keratomycosis is the greek word equivalent to fungal keratitis, and it refers to a corneal infection caused by fungi which can end up in severe loss of visual acuity or even enucleation. Fungal keratitis is encountered in tropical climates and in populations related to land cultivation. In the United States keratomycosis is significantly more common to the southern states. Outbreaks of fungal ceratitis have been attributed in the past to specific contact lens solutions. In Germany there are no specific epidemiologic data on keratomycosis. We investigated two different cases of multidrug-resistant fungal keratitis caused by Fusarium solani that did not respond to the intensive conservative local and systemic antifungal therapy-ultimately requiring a keratoplasty à chaud; one of the cases progressed to endophthalmitis, and finally required an enucleation.
Methods and Results
Case 1
A 21-year old male, who used monthly soft contact lenses for 5 years, initially reported to our department’s clinic with pain, photophobia and decreased vision in the right eye for one week starting in October 2014. In his medical history there was no ocular surgery or trauma in the past. The visual acuity of the infected eye in the first case was 1 out of 10. Upon examination, we found a central corneal ulcer of 3.1 mm in diameter with irregular borders, slight infiltration, and a thinned cornea. A hypopyon of 1.0 mm was evident. The left eye showed no abnormalities. Our initial diagnosis was a contact lens associated keratitis. The patient was treated with topical eye drops consisting of Moxifloxacin, Gentamicin and Dexamethasone every hour around the clock. Repeat corneal cultures were performed which initially revealed Staphylococcus epidermidis, although the contact lens culture showed the existence of Enterococcus casseliflavus, Corynebacterium species and Candida lusitaniae. Unfortunately, the epithelial disease recurred and the patient reported once again to the hospital 15 days later. Upon examination, he was diagnosed with extensive epithelial edema, hypopyon and corneal infiltrate. The patient underwent a biopsy of corneal epithelium. The biopsy results were negative for Acanthamoeba and Fungi. Therefore, a corneal collagen crosslinking with Riboflavin and a dose of UVA light of 3 mW/cm2 were applied twice for 30 minutes. This therapy resulted in a slight improvement of the patient´s condition. The patient was further treated with a combination therapy. It consisted of: Polyhexanid 0.02% and Propamidinisoethinat 0.1% eye drops every two hours around the clock; Vancomycin eye drops 5 times a day; Neomycin/ Polymycin eye drops 5 times a day; Fluconazole 200 mg and Doxycyclin 100 mg oral therapy once a day. Despite the prescribed therapeutic schema, the ocular findings worsened. Visual acuity declined to light perception. The clinical findings correlated with the working diagnosis of fungal keratitis. In December 2014, the patient underwent a keratoplasty à chaud of the right eye. Postoperatively, 8 injections of Voriconazole 10 μgram/0.1 ml were administered into the anterior chamber after placement of the graft. A further corneal biopsy showed a fungal keratitis and the culture of the aqueous humour of the puncture of the anterior chamber revealed Fusarium solani resistant to all the antimycotics.
Antifungal susceptibility testing was performed according to the guidelines of the European Committee on Antimicrobial susceptibility Testing (EUCAST). The microbiological laboratory used the minimum inhibitory concentrations (MIC) in order to determine the type and the amount of antifungal agent that the patient will receive, which in turn lowered the risk for microbial resistance to specific antifungal agents. Minimum inhibitory concentration (MIC) is defined as the lowest concentration of an antimicrobial agent that prevents the visible growth of a microorganism after overnight incubation. In the first case MIC of Amphotericin B appears to be the lowest one of all the tested antifungal agents. Therefore, Amphotericin B seemed to be the most appropriate local and systemic antimycotic therapy to minimize the possibility of recurrence of the fungal keratitis (Table 1).
| Antimycotic agent Minimal inhibitory concentrations (MIC) |
| Amphotericin B |
2 μg/ml |
| Casponfugin |
>8 μg/ml |
| Anidulafungin |
>8 μg/ml |
| Terbinfafin |
>32 μg/ml |
| Fluconazol |
>64 μg/ml |
| Voriconazole |
4 μg/ml |
| Posaconazol |
>8 μg/ml |
| Itraconazol |
>8 μg/ml |
Table 1: Antifungal susceptibility testing through Microdilutiοns-Test (EUCAST) concerning the first patient.
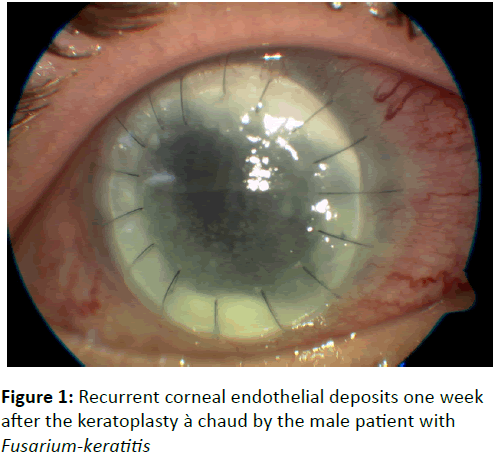
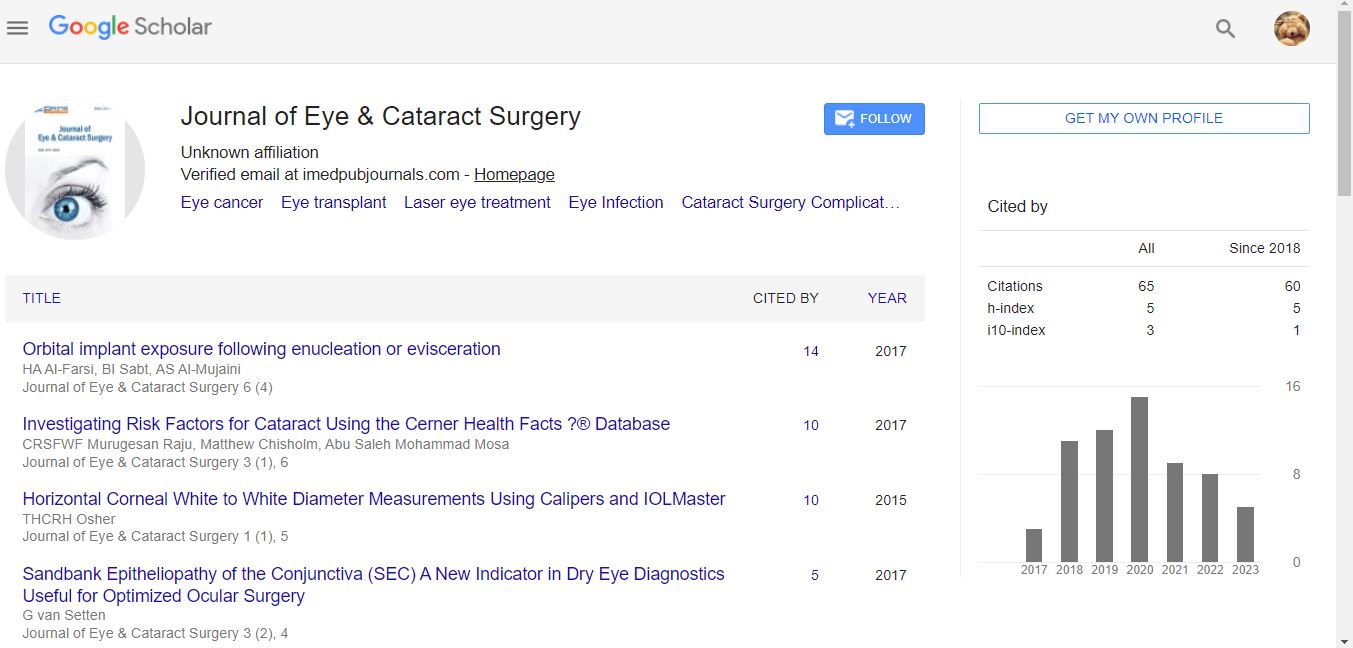
At first, the patient recovered well from the surgery and maintained a clear anterior chamber and corneal graft tissue. The antibiotic regime constisted of topical Voriconazole eye drops every hour, Voriconazole 200 mg i.v. twice a day and oral Doxycyclin 100 mg once a day. However, two weeks later, recurrent corneal endothelial deposits and stromal edema began to develop in the center of the graft (Figure 1), followed by the appearance of cells and hypopyon in the anterior chamber. The patient underwent repeat injections of Amphotericin B into the anterior chamber combined with corneal abrasion one month after the keratoplasty. Cultures from a biopsy of the excised cornea once again revealed the same Fusarium species. An intense local therapy with Amphotericin B eye drops every half hour around the clock and lyposomal Αmphotericin B 240 mg i.v. resulted in no improvement of the eye condition. The patient developed a mild pharmaceutical hepatitis induced by Αmphotericin B.
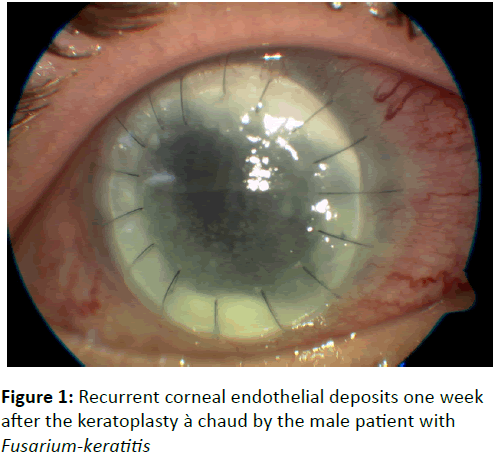
Figure 1: Recurrent corneal endothelial deposits one week after the keratoplasty à chaud by the male patient with Fusarium-keratitis
A week later the condition of the eye worsened; the corneal infiltration increased and hypopyon built up. The stromal and endothelial infection became turbid and progressed into a deep corneal abscess and endophthalmitis. Due to multiple high resistance of Fusarium solani to antimycotics with resultant failure of antibiotic therapy, an enucleation of the infected eye was performed. The patient was discharged from the hospital on Αmphotericin B and Gentamicin eye drops 5 times a day as well as on oral Voriconazole 200 mg twice a day.
Case 2
Α 26-year old female patient, who also used monthly soft contact lenses, reported to the emergency room with mild eye pain, eye redness, photophobia and progressive loss of visual acuity. These symptoms had been progressing for 10 days in the left eye. The incidence occurred in June 2015. No ocular injuries or surgeries were known from medical history. The patient reported that she was a scuba diving teacher and had recently been on a trip to Thailand, where she swam keeping her contact lenses always on. The patient was initially treated in Thailand with eye drops consisting of Tobramycin and Dexamethasone 5 times a day because of eye redness and mild pain. One day prior to admission the regimen was changed to a combination of Ceftazidime and Vancomycin eye drops every half hour. The visual acuity of the left eye was limited to hand motion. The slit lamp examination showed corneal epithelial edema, an ulcer measuring 2.6 x 3.0 mm, hypopyon of 1.4 mm, Descemet’s folds but no sign of corneal perforation. The B-Scan sonography revealed no infiltration of the vitreous humour. A corneal culture was performed immediately and yielded Fusarium solani with a very high resistance to all antimycotics.
The patient was treated initially with Amphotericin B eye ointment, Moxifloxacin eye drops and eye drops with Gentamicin each of them five times a day and Cyclopentolat eye drops 2 times a day. In addition, Voriconazole 200 mg i.v. was administered two times a day. In the next 5 days there was no improvement in the slit lamp findings. Therefore, we decided to perform a corneal cross linking which was repeated 2 days later. Nonetheless, the corneal ulcer remained stable and the visual acuity decreased further to light perception. As a result, the conservative therapy was changed to Natamycin 5 %, Amphotericin B and Polyhexanide 0.02% eye drops 5 times a day, as well as lyposomal Amphotericin B i.v. 150 mg once a day. We performed a third corneal cross linking therapy and two intracameral injections of Amphotericin B 5 μgram were administered (Table 2).
| Antimycotic agent Minimal inhibitory concentrations (MIC) |
| Amphotericin B |
4 μg/ml |
| Casponfugin |
> 8 μg/ml |
| Anidulafungin |
> 8 μg/ml |
| Terbinfafin |
>32 μg/ml |
| Voriconazole |
8 μg/ml |
| Posaconazol |
>8 μg/ml |
| Itraconazol |
>8 μg/ml |
Table 2: Antifungal susceptibility testing through Microdilutiοns-Test (EUCAST) concerning the second patient.
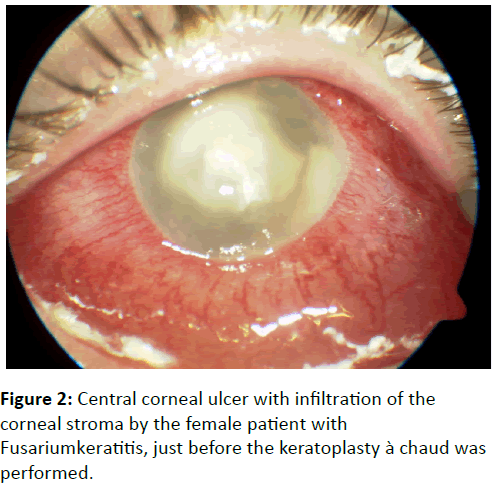
The following 3 days, the central corneal infiltrate worsened (Figure 2), so the patient underwent a combined therapy which consisted of: 1) the application of Povidon-Iodine Solution 0.5% with a swab stick on the infected cornea for 3 minutes, 2) cryocoagulation circular at limbus with 8 spots for 20 sec. with temperature -62 °C, 3) a keratoplasty à chaud. In the following 10 days 5 injections of Amphotericin B intracameral and subconjuctival (one injection per quadrant, four times) were necessary.
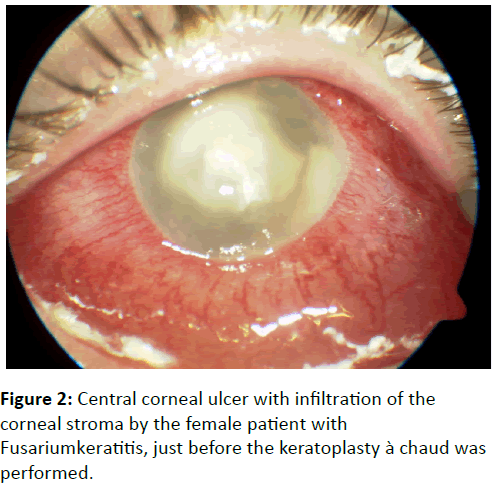
Figure 2: Central corneal ulcer with infiltration of the corneal stroma by the female patient with Fusariumkeratitis, just before the keratoplasty à chaud was performed.
The pathology and microbiological test of the excised cornea revealed a massive granulocytic keratitis with infiltration of the corneal stroma. A positive PAS-reaction was detectable in the corneal stroma. The microbiological culture revealed no bacterial colonies. Two weeks postoperatively the corneal transplant remained clear and the ocular findings showed no recurrence of the disease. The patient was discharged from the hospital with visual acuity of 1 out of 10 on the following therapeutic regime: Natamycin 5% eye drops and Amphotericin B ocular ointment every two hours around the clock, Cyclopentolate three a day, Prednisolone eye drops six times a day and Polyhexanid 0.02 % every hour. The patient was also prescribed Voriconazole 300 mg twice a day and Doxycyclin 100 mg once a day per os.
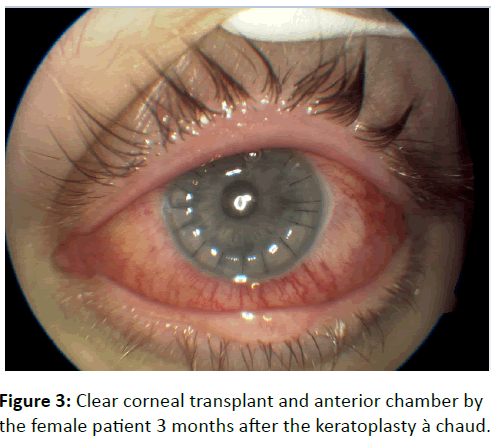
During the 7- month follow up, the patient showed stable ocular findings (Figure 3) and improvement of the visual acuity to 5 out of 10. The local therapy was reduced to Natamycin 5% eye drops and Amphotericin B ocular ointment four times per day, Prednisolone eye drops six times per day and Polyhexanid 0.02 % every hour. The systemic therapy with Voriconazole 200 mg per os twice a day was continued for at least 3 months postoperatively.
Figure 3: Clear corneal transplant and anterior chamber by the female patient 3 months after the keratoplasty à chaud.
Discussion
Fungal keratitis or keratomycosis refers to an infectious process of the cornea caused by any fungal species that can lead to a decrease of vision and potentially to blindness. An enucleation of the eye as part of the treatment may be necessary [1,2]. Keratomycosis was first described by Leber in 1879 [3] and presents an insidious, rapidly progressive disease, which is difficult to diagnose and it can be refractory not only to conservative but also to surgical treatment [1]. The most important factors that favour a good prognosis are: timely diagnosis and adequate therapy-either conservative or operative. Especially Fusarium solani is a phylogenetic, multiresistent microorganism and its identification by morphological traits is often difficult and highly dependent on composition of media and accurate species identification, especially if performed with rapid PCR techniques that may yield important prognostic and therapeutic information that can influence management decisions and improve patient outcomes in the setting of Fusarium keratitis. Therefore, it is of great importance to present the efficacy of the multiple therapeutic methods. The treatment of a keratomycosis can be conservative, or even combined with surgical methods [4]. The polyenes, the azoles, the allylamines, the echinocandins and the fluorinated pyrimidines belong to the antifungal agents. The first category includes Natamycin, Nystatin and Amphotericin B which bind to the ergosterol of the fungal cell wall eventually resulting in its disruption. In this way polyenes are effective against yeast and filamentous fungi [2,5].
Amphotericin B can be used not only as local therapy (eye drops, intracameral or intravitreal), but also as systemic therapy (i.v.). Because of the nephrotoxicity and the hepatotoxicity of the systemic treatment with amphotericin B, its liposomal form with 5-Flucytosin is preferred. The concentration of the Amphotericin B in the eye drop is 0. 5%. Because of the high molecular weight a corneal abrasion should be performed in order for a better ocular penetration to be achieved. The concentration of amphotericin B for the intracameral or intravitreal usage is 7.5 μg/2ml [6]. Although it was shown that Fusarium solani in the first case which we described was resistant to all the antimycotics, we applied at first a local and systemic therapy with Voriconazole although its MIC was lower than that of Amphotericin B in order to avoid its toxicity and massive side effects. Because the slit lamp findings did not improve, we continued with a local therapy with Amphotericin B eye drops 0.5 % every hour after the performance of a corneal abrasion as well as an i.v. therapy with lyposomal Amphotericin B based on the guidelines of the German national reference-center of fungal infections. However, the intensive therapy provided no improvement of the ocular findings and simultaneously provoked a hepatotoxic reaction with severe increase of the levels of hepatic transaminases (>150 UI/l). Natamycin and Nystatin are prescribed only as local therapy because of their toxicity and both are effective against filamentous fungi, particularly for keratitis caused by Fusarium. Although it has been shown that the penetration of topically applied Natamycin is better than that of Amphotericin B through the intact corneal epithelium, the penetration still remains low and it is mainly useful in cases with superficial corneal infection [1,3]. In the second case of fungal keratitis that was presented, the microbiological examination revealed a higher resistance of F. solani to all the antimycotics as in the first case, and the MIC of Amphotericin B und Voriconazole was higher. In spite of that, a combined local therapy of Amphotericin B and Natamycin eye drops every two hours after a corneal abrasion, in addition to the postoperative application of 5 intracameral and subconjuctival injections of Amphotericin B resulted in the successful improvement of the clinical findings of keratomycosis. Under the local therapy with Natamycin and Amphotericin B eye drops and systemic therapy with Voriconazole per os the patient still remains without any signs of recurrence even three months after the keratoplasty à chaud. Azoles play an important role in the treatment of the deep fungal keratitis [3]. Specifically because of its low molecular weight, Fluconazole penetrates the corneal epithelium, and therefore an iatrogenic abrasion isn’t necessary [6]. The fluorinated pyrimidines work synergistic with other antifungal agents as resistance to pyrimidines develops rapidly, these should never be used as monotherapy [2].
Polyhexanid is one of the standard drugs against Acanthamoeba; its effectiveness against Fusarium has been shown not only through in vitro but also through in vivo studies. Patients with fusarium keratitis, who had no response to the therapy with other antifungal agents, demonstrated an improvement of the corneal findings under the local therapy with 0.02% Polyhexanid. Because of the high molecular weight of 5000 Da an iatrogenic abrasion should be performed routinely so that the antibiotic can penetrate the tissue [2,3]. The combined therapy of two different antifungal agents and Polyhexanid resulted successfully in an important improvement of the corneal findings and therefore, the bulbus and the visual function of the second patient presented here were maintained. Optimal treatment for Fusarium spp. has not yet been established. At best, response rates to antifungals such as lipid amphotericin B, voriconazole or posaconazole have ranged between 45% and 48%. It is of great importance to emphasize that despite the multiresistance of Fusarium solani in both cases of keratitis that were presented, not only the local but also the systemic therapies were both adjusted according to the MIC based upon recommendation guidelines of the German national reference-centre of fungal infections. The goal of this effort wasn’t the complete healing of the fungal keratitis, but the avoidance of the expansion of the infection to the adjacent structures of the eye such as limbus, sclera, anterior chamber as well as the corneal graft. This goal was not achieved in the first case as the fungi penetrated the cornea and infiltrated the anterior chamber and the vitreous resulting in panophthalmitis that finally required enucleation. After this unfortunate experience we decided to follow a more aggressive, not only conservative but also surgical regime in an early stage of the corneal infection in the second patient. This approach was very successful as the eye of the patient was preserved. Another option for medical treatment of keratomycosis is the application of antiseptic agents on the cornea. Povidone-iodine is an antiseptic agent effective against gram positive and gram negative bacteria, spores, amoebic cysts, fungi, protozoa, yeasts and can be used therapeutically on corneal ulcers. Kalu has shown in his study that the synergistic use of povidone-iodine (0.5%) and 5% natamycin is effective in prevention of filamentous keratitis and its efficacy is independent of fungal species [7]. The in vitro study of Yan Xu reveals that silver nitrate may be effective against corneal Fusarium and Aspergillus isolates [8]. Singh has also introduced the application of silver nitrate with a swab stick on the corneal ulcers in his therapeutic schema against fungal keratitis. Silver nitrate binds to the DNA of microorganisms and prevents the unzipping of the DNA helix, inhibiting replication. It is also assumed that silver nitrate starts ionizing, thus releasing nascent oxygen that has the capacity to destroy the fungal wall. Singh treats more than 200 fungal corneal ulcer cases every year by starting the therapy with the application of silver nitrate 0.75% and Lugol iodine on the corneal ulcer followed by local and systemic antifungal therapy [2]. According to Singh’s regime the application of povidone-iodine solution is followed by the cryocoagulation of the limbus and a keratoplasty à chaud. These interventions combined with an intensive antifungal local and systemic therapy resulted in the maintenance of the bulbus as well as the visual function of the female patient. Unfortunately, the intensive local and systemic therapy is not sufficient for approximately 15-27 % of the cases with keratomycosis. In these resistant cases surgical intervention is required. Studies have shown that UVACrosslinking with Riboflavin has a limited efficacy in cases of fungal keratitis in comparison to keratitis caused by bacteria. However, a treatment with photodynamic keratectomy (PTK) with Belgalrosa has been proved in in vitro studies to be effective in Keratitis caused by Fusarium solani or Aspergillus [9].
In cases not responding to aggressive antifungal therapy a keratoplasty à chaud should be performed before the corneal disease progresses to the anterior chamber or reaches the limbus or the sclera. Otherwise, the prognosis for maintenance of the visual function or even the bulbus is dismal [2]. In general keratoplasty à chaud is reffered to penetrating corneal surgery on inflamed eye, that is either non responsive to clinical treatment or at risk for perforation. In literature there are not many case series with keratoplasty à chaud and outcome analysis. Verhelle and Maudgal in 1996 report on 19 keratoplasties where the infectious agent was persistent only in a case of acanthamoeba keratitis, the visual acuity outcome was variable but fair enough [10]. Stübiger et al report on 128 keratoplasties. 95% of the eyes coud be preserved and in 54% the visual acuity was improved. In literature there are no studies dedicated to early vs late keratoplasty and outcome analysis [11].
In cases of infiltration of the posterior chamber, beyond keratoplasty an extraction of the lens, opening of the posterior capsule and perhaps also a core vitrectomy with intracameral injection of antifungal agents are to be considered [3]. If the sclera or limbus is infiltrated then a tectonic keratoplasty is needed, although even then, the chances to preserve the bulbus are very limited [3]. The male patient presented here underwent a keratoplasty à chaud relatively late. In this case, not only the anterior and the posterior chamber but also the aqueous humours were infiltrated. As a result, the transplant was infiltrated in about one week postoperatively. Because of our unfortunate experience with this patient, a keratoplasty à chaud was performed on the female patient before the posterior chamber was infiltrated. As a result, the prognosis was much better and the patient maintained a visual acuity of 3 out of 10.
In conclusion, although keratomycosis is a severe corneal disease which can affect the visual acuity and eventually can lead even to enucleation, the new therapeutic modalities can deliver a faster diagnosis so a targeted therapy can be implemented sooner. According to our clinical experience we would highly recommend: 1) an early keratoplasty à chaud be performed as soon as the diagnosis of a fungal keratitis is confirmed. The procedure will prevent the fungi from expanding to the corneal limbus and the anterior chamber, 2) the combination of the keratoplasty à chaud with the application of Povidone-Iodine solution with a swab stick on the infected cornea, the cryocoagulation of the limbus and the subconjunctival injections of Amphotericin B could be beneficial in cases of keratomycosis caused by multiresistant fungi, 3) lastly, in terms of prevention for the contact-lensassociated keratitis, we should not underestimate the importance of correct lens cleaning and preservation in the right fluids. In this regard, in depth public education should be encouraged.
References
- Mravicic I, Dekaris I, Gabric N, Romac I, Glavota V (2012) An overview of fungal keratitis and case report on Trichophyton keratitis. Intech.
- Singh D (2015) Fungal Keratitis.
- Behrens-Baumann W, Finis D, MacKenzie C (2015) Keratomycosis – Therapy Standards and New Developments. KlinMonantsblAugenheilkd 232: 754-764.
- Eddy MT, Steinberg J, Richard G, Hassenstein A (2012) Severe contact lens-associated fungal keratitis. Ophthalmologe 109: 1106-1111.
- Thomas PA (2003) Fungal infections of the cornea. Eye 17: 852-862.
- Al-Badriyeh D, Neoh CF, Stewart K, Kong DC (2010) Clinical utility of voriconazole eye drops in ophthalmic fungal keratitis. ClinOphthalmol 4: 391-405.
- Kalu C (2005) Positive impact of povidone-iodine and natamycin in prevention of filamentous fungal keratitis in rabbit model. American Academy of Optometry.
- Xu Y, Pang G, Gao C, Zhao D, Zhou L, et al. (2009) In Vitro Comparison of the Efficacies of Natamycin and Silver Nitrate against Ocular Fungi. Antimicrob Agents Chemother 53: 1636-1638.
- Alnawaiseh M, Böhm MR, Idelevich EA, Becker K, Grewe S, et al. (2014) Successful treatment of Fusarium-associated keratitis with multiresistant pathogen and multimorbid patient. Ophthalmologe 111: 259-261.
- Verhelle V, Maudgal PC (1996) Keratoplasty à chaud in severe keratitis. Bull SocBelgeOphtalmol 261: 29-36.
- Stübiger N, Pleyer U, Erb C, Thiel HJ (1995) Keratoplasty à chaud. Ophthalmologe 92: 427-432.