Keywords
Treatment outcomes; Tuberculosis patient; DOTS; North West Ethiopia
Introduction
Background
Tuberculosis (TB) is a chronic infectious disease caused by mycobacterium tuberculosis (MTB). It typically affects the lungs (pulmonary TB) but can affect other parts of the body (extra pulmonary TB). The disease is spread via droplet infection when people with pulmonary TB expel the bacilli while coughing, sneezing, talking, etc[1,2].
Almost 1/3 of the world population (about 2 billion) is infected with mycobacterium tuberculosis during the past decade(1). Currently, TB is the leading causes of mortality among infectious diseases worldwide, 95% of TB cases and 98% of TB deaths occur in developing countries [3]. Direct observed treatment (DOTS) is one of the widely accepted global health intervention for tuberculosis. The target of DOTS was to achieve a case detection rate of 84% (all forms of TB) and treatment success rate (TSR) of 87% by 2015 [4].
Ethiopia adopted the DOTS Strategy and has been implementing early. Overall, DOTS coverage among government owned hospitals and health centers has reached to 95%. The “STOP TB” strategy was launched by World Health Organization (WHO) in 2006 to achieve Millennium Development Goals (MDGs) for TB in 2015. Ethiopia also adopted this strategy to achieve the national TB /leprosy targets [5].
The END TB strategy was also launched by WHO with envision of zero deaths, diseases, and suffering due to Tuberculosis along with Sustainable Development Goals (SDGs) at 2035[6]. Though recently studies are showing a decline in the incidence and prevalence of tuberculosis in many countries, case numbers but Multidrug resistance tuberculosis (MDR TB) continue to rise in much of Sub-Saharan countries where HIV is pandemic including Ethiopia [7]. Treatment outcome results serve as a proxy measure of the quality of TB treatment provided by a health care system. Treatment success measured by treatment outcome monitoring is a key output of TB control program [8]. Treatment outcome in all patients should be routinely monitored by the epidemiological surveillance system. This will make it possible to recognize and amend system failures [9]. In addition treatment outcome monitoring is important to evaluate the effectiveness of DOTS Program.Moreover, understanding the specific reasons for unsuccessful outcomes is important in order to improve treatment strategy [10].
Statement of the problem
Despite the availability of effective drugs tuberculosis (TB) is still a global emergency and one of the major public health problems in the 21st century [6]. It is not only a public health problem, but also a socio-economic issue [11]. Globally, TB prevalence in 2015 was 42% lower than in 1990 [5]. Nearly, 1.5 million people died including 0.4 million people who were HIV positive. There were also an estimated 9.6 million new cases of TB including 1.2 million people living with HIV. Of the estimated 9.6 million people who developed TB, more than half (58%) were in the south-east Asia and Western Pacific regions and 28% were in the African Regions but the highest rates of cases and deaths out of the total population (281 cases for every 100 000 people) more than double the global average of 133 occurred in the African region [12]. However, the TB death rate has decreased by 47% since 1990 with nearly all of that improvement taking place since 2000 when the Millennium Development Goals (MDGs) were set. Globally, the treatment success rate for people newly diagnosed with TB was 86% in 2013 and approximately 480,000 people developed multidrug-resistant TB (MDR-TB) and there were an estimated 190,000 deaths from MDR-TB [5].
Global trends show that TB incidence, prevalence and mortality rates are gradually declining. However, the increase in MDR- and EXDR-TB cases is worrisome. Tuberculosis remains a disease of poverty with a high burden of disease in the low middle income countries (LMICs) and in countries with a high HIV prevalence [13]. In developing countries, there is high burden of TB and HIV, delayed diagnosis which is a major contributing factor to the continued transmission and failure to treatment outcome [2]. Ethiopia ranks tenth among the 30 high-TB, HIV and MDR TB burden countries (HBCs) and third in Africa. TB remains one of the leading causes of mortality. It is also the leading cause of morbidity, the third cause of hospital admission and the second cause of death in Ethiopia [14].
According to WHO TB report in 2014, the prevalence and incidence of all forms of TB in Ethiopia is 211 and 207 per 100,000 populations respectively. Excluding HIV related deaths; TB death rate was estimated to be 33 per 100,000 populations in 2014. Among estimated all new TB cases, 13% are HIV co-infected. Moreover, Ethiopia is also one of the high TB/HIV and multi-drug resistant TB (MDR TB) burden countries. According to the recent national TB drug resistance surveillance report, 2.3% of new TB cases and 17.8% of previously treated TB cases were estimated to have MDR which indicates increasing trends in TB drugs resistance burden compared to the first Drug Resistance Survey conducted in 2003-2005 [5].
Treatment outcome and detection rate are the performance indicators of DOTs program set by World Health Organization (WHO) [14,15]. Disease surveillance system and treatment outcome monitoring are considered as the key source of evidence to evaluate the effectiveness of tuberculosis prevention and control program like DOTs [12].
In Ethiopia, DOTs reach coverage of 90 % [9] so the target of halving TB prevalence and mortality rates by 2015 has also been met [5]. DOTs given for at least the first two months of treatment under the direct observation of health care providers has been found to be effective in achieving a highly successful treatment outcome ranging from 86 to 96.5% [16]. Similarly, treatment success rate is considered as a proxy indicator of the quality of health care services and it is usually affected by various reasons despite the existence of increment in treatment success rate in almost all of the studies done in Ethiopia [17]. The average treatment success rate in most of them was below the MDG target [14]. On top of these, 2016 marks the beginning of End TB Strategy and it is SDG target for 2035 [18].
Justification of the study
WHO recommends TB Diseases surveillance system and treatment outcome should be monitored periodically and there is no reports on the DOTS experience in Buriezuria, Jabitehinanand Fenoteselam administrative town health facilities. This study is aimed at assess the treatment Success and associated risk factors for tuberculosis patients registered at Buriezuria, Jabitehinan and Fenoteselam town health facilities DOTS program. Determining the treatment success rate of the health institutions will help program planners and health professionals to show where they are relative to MDG tuberculosis target. if the TSR is under the target, it could lead them to identify potential areas of improvement for implementing End TB strategy. itcould have its own role in preventing multidrug resistance (MDR-TB) and extensive drug resistance (EXDR-TB) tuberculosis. Generally, this study is important to Amhara regional health bureau, Fenoteselam administration health office, Jabitehinan health office, Buriezuria Health office and studied health facilities to know the treatment outcome of tuberculosis patient and associated factors to plan appropriate interventions. It will also be evidence to researchers who are interested on the topic.
Methods
Study location
Fenoteselam and Burietowns are located in the northwest Ethiopia 378 kilometers and 390 kilometers away from Addis Ababa, capital city of Ethiopia respectively. They have its Zuria Woreda which have been serving for rural populations. There are two Hospitals, 20 health centers whichall delivers DOTS service for the people living in and around Fenoteselam and Burie. Patients were diagnosed, registered, treated and referred to other DOTS clinics following the National Tuberculosis and Leprosy Control Program (NTLCP) guideline [19-32].TB contact tracing and identification of high risk group, intensive follow up TB patients, mentoring MDR patients on household level and Nutritional and other economic support Programs are lunched targeting to enhance TB treatment outcomes in the study settings. The study was conducted at districts of Buriezuria, Jabitehinan and Fenoteselam town.
Study design and period
Facility based Cross-sectional survey was conducted among TB patients registered from 2012 to 2016 at DOTS clinic at districts of Buriezuria, Jabitehinanand Fenoteselam town.
Source population
The source populations of the study were all tuberculosis patients registered for TB DOTS program (N=7124patients) ingovernment owned health institution in districts of Buriezuria, Jabitehinan and Fenoteselam town from July, 2012 to June, 2016.
Study population
The study population were selected patients with tuberculosis (n=832) who have had treatment outcomes in government owned health institution in districts of Buriezuria, Jabitehinan and Fenoteselam town health facilities between July, 2012 and June, 2016.
Inclusion criteria and exclusion criteria
All TB patients with complete data like age, sex, residence, treatment outcome were included. Missing of study variables was excluded.
Sample size determination
The sample size was calculated using single population proportion formula, for the dependent variable and to the identified factors which have significant association with dependent variable by considering 95% Confidence level, 5% margin of error. Tuberculosis treatment success rate of by taking estimated average 28%, treatment success rate ranges from 26%-94.8% in Amhara Region [17,27,29,30-32].
Where n: Sample size; p: Estimated average tuberculosis treatment success rate; z: Standard normal value at 95% confidence interval=1.96; w: Margin of error (relative precision) Using Epidemiological information (Epi-info), sample size will be 832 [16] (Table 1).
| Identified Factors |
power |
Ratio(unexposed :exposed) |
Confidence level |
%outcome unexposed group |
OR |
%outcome exposed |
Sample size |
| Co-morbidity |
80% |
2 |
95% |
4.79 |
2.29 |
10.4 |
832 |
| Type of TB |
80% |
2 |
95% |
4.90 |
2.3 |
10.6 |
816 |
| Retreatment |
80% |
2 |
95% |
2.1 |
3.3 |
6.6 |
765 |
Table 1: Sample size determination.
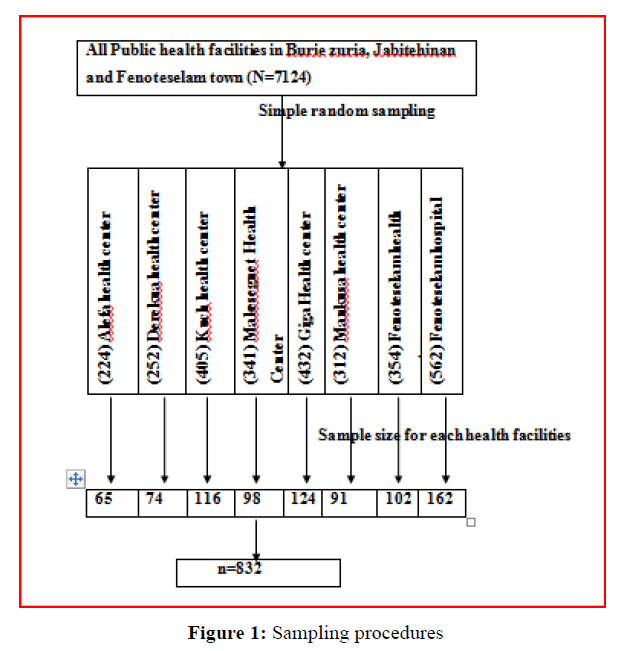
Sampling procedures
First we obtained the list of all public health facilities providing TB diagnosis and treatment Services in districts of Buriezuria, Jabitehinan and Fenoteselam town. There are twenty two health facilities which are serving TB/DOTS service in the study area. Eight health facilities were selected randomly and proportional allocation of the total sample size was carried out to attain the required sample size in each health facilities. The shared sample size for each health facilities divided by the total number of registered TB patients in a given health facility to determine a sampling interval and then study units were selected by systematic random sampling every Kth from registers of health facilities during the study period (Figure 1).
Figure 1: Sampling procedures
Data collection procedures and quality assurance
Data were extracted from registers of health facilities using a structured data sheet especially designed for this study. The contents of the checklist was included socio-demographic data (such as sex, age, and residence),Weight, HIV status, Type of TB, previous history of TB treatment , year of enrolment, and the treatment outcomes of the TB patients were collected from the DOTS registration book. Data extraction was conducted by Nurses and Health Officers who were not working in the Study area.
To ensure data quality the following measures were taken:
a. One day training was given for data collectors before the start of data collection.
b. The overall activities of data extraction were monitored by principal investigator and there were strict supervision during data collection.
c. All completed datasets were examined by the principal investigator for completeness during data collection.
d. From the data extracted from each health facility,5% of the sample was randomly selected and validated against the registration book by the principal investigator.
Variables
Dependent variables
• Tuberculosis treatment outcomes (Codes was given as Successful treatment outcome (1), unsuccessful treatment outcome (0)).
Independent variables
• Socio-demography: Age, Gender, Weight, Residence
• Clinical factors: type of TB (PTB, EPTB), Cases of TB (Bacteriologically confirmed TB, Clinically diagnosed TB), TB patient Type (New cases, Previously treated TB case), HIV Status, Year of enrollment, Center of TB screen, Patient registration groups (New patients, Relapse patients, Treatment after failure, Treatment after loss to follow up, Others, Transfer out).
Operational definition
Pulmonary Tuberculosis: Any bacteriologically confirmed or clinically diagnosed cases of TB involving the lung parenchyma or the trachea-bronchial tree.
Extra pulmonary TB (EPTB): Any bacteriologically confirmed or clinically diagnosed cases of TB involving of organs other than the lungs such as lymph nodes, abdomen, genitourinary tract, skin, joints and bones and meninges.
Previously treated cases: Patients that have received 1 month or more of anti-TB drugs in the past
New patients: patients that have never been treated for TB or have taken anti-TB drugs for less than 1 month.
Relapse patients: patients that have previously been treated for TB were declared cured or treatment completed at the end of their most recent course of treatment and is now diagnosed with a recurrent episode of TB.
Treatment after failure: patients are those who have previously been treated for TB and whose treatment failedat the end of their most recent course of treatment.
Treatment after loss to follow-up: patients have previously been treated for TB and were declared lost to follow-up at the end of their most recent course of treatment and are now diagnosed with TB.
Others: Patients who have previously been treated for TB but whose outcome after their most recent course of treatment is unknown or undocumented or patients that do not fit into any of the categories listed above.
Transfer out (T): A patient who started treatment in one treatment unit and is transferred to another treatment unit to continue treatment.
Successful Treatment outcome: if bacteriologically confirmed PTB were cured (i.e. negative smear result at the end of treatment and on at least one previous follow-up test) or clinically diagnosed PTB/EPTB were Completed their treatment with resolutions of symptoms.
Unsuccessful treatment outcome includes treatment of PTB/ EPTB patients resulted in treatment failure ,defaulted , death and not evaluated.
• Treatment failure: this term used for pulmonary confirmed TB patients whose follow up smear results remain positive at or beyond fifth month into treatment.
• Lost to follow up (LTFU): This term used for TB patient on treatment for at least four weeks and who has discontinued TB treatment for eight or more consecutive week.
• Died: This term used for TB patient who is reported dead while receiving TB treatment, cause of death may not be related to TB.
• Not evaluated: This term used for patient whose final treatment outcome is not known at time of evaluation
• Moved to MDR-TB: It istermed as TB patient who are found to harbor drug resistant strain at least for Rifampicin, with documentation of lab result, before fifth month of TB treatment.
Data processing and analysis
All data were entered in to Epi Enfo 3.1 and analyzed using SPSS version 20. A descriptive analysis was used to determine differences within the data of Variables. All explanatory variables a p value <0.25 in bi-variate analysis were included in the multivariable logistic regression model to identify independent predictive Variables. Odds Ratio (OR), 95% confidence Interval (CI) were calculated. The results were considered statistically significant at P value <0.05 in the final model.
Results
Socio demographic and clinical characteristics of study participants
A total of 832 patients’ were included in the study whose age ranged from 1 to 80 years, mean and standard deviation of 29.33+14.26 years were included in the study with response rate of 100%. Among study participants, 53.6% were males and 46.4% were females. Children <14 years of ageaccounted 9.7% of the study participants. The majority of participants were in the age group of 15-24 and 25-34yrs old which accounts 31.6% and 25.2% respectively. Majority of patients were urban residents 61.9% (Table 2).
| Characteristics of Variable |
PTB n (%) |
EPTB n (%) |
Total n (%) |
| Sex |
| Male |
260 (30.8) |
190 (22.71) |
450(53.6) |
| Female |
205 (25) |
177 (21.3) |
382(46.4) |
| Residence |
| Urban |
269 (32.3) |
246 (29.5) |
515 (61.9) |
| Rural |
196 (23.5) |
121 (32.1) |
317 (38.1) |
| Age |
| <14 |
27 (3.2) |
54(6.4) |
81(9.7) |
| 15-24 |
140(16.8) |
140(16.8) |
263(31.6) |
| 25-34 |
129(15.5) |
81(9.7) |
210(25.2) |
| 35-49 |
112(13.4) |
56(6.7) |
168(20.2) |
| >50 |
57 (6.8) |
36(4.3) |
93(11.1) |
| HIV Test |
| positive |
94(11.3) |
42(5.0) |
136(16.3) |
| Negative |
357(42.9) |
315(37.9) |
672(80.7) |
| Unknown |
14(1.7) |
10(1.2) |
24(2.9) |
| Total n (%) |
465 (56) |
367 (44) |
832 (100) |
PTB: pulmonary tuberculosis; EPTB: Extraplumonary tuberculosis
Table 2: Characteristics of TB patients (n=832) with type of TB DOTS Clinics of at Buriezuria, Jabitehinan and Fenoteselam town health facilities, 2012 to 2016.
Most tuberculosis patients 95.6% were new cases. During the study period, TB patients’ defaulter, death and failure rate were 2.6%, 3.1% and 1.2% respectively. Of 832 TB patients registered for anti-tuberculosis treatment 97.1% were tested for HIV. The TB-HIV co-infection was 16.8%. The PTB and EPTB type of TB among TB-HIV co-infected patients was 69.2% and 30.8% respectively. The death rate of PTB and EPTB were 61.5% and 38.46% respectively.
Treatment outcome
The overall treatment Success rate was 82.5% across a period of five years. Among all known treatmentoutcome 13.1% were cured, 69.4% completed, 1.2% treatment failure, 2.6% defaulters, 3.1% deaths while1.2% were moved to MDR whereas the rest was transfer out9.5%.
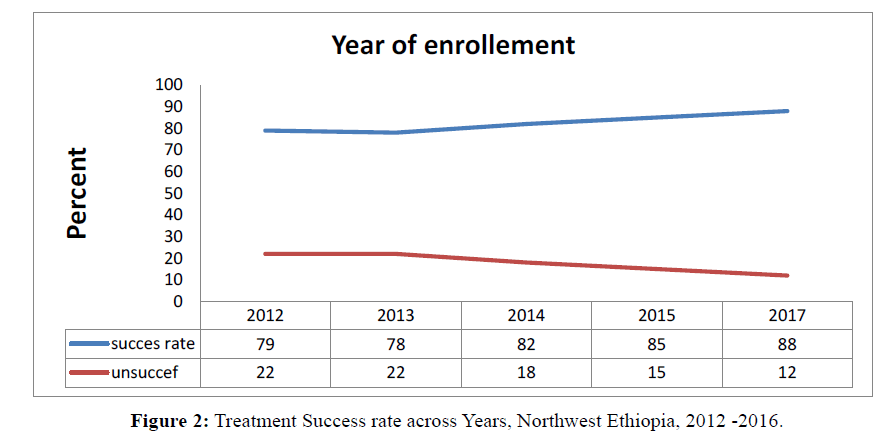
In this study, a high proportion of defaulter 0.57% and moved to MDR 0.78% was recorded for males.In this study, MDR TB was increased over a period of the study years. During the study years, the successful treatment outcome under DOTS program of TB patients vary from years to years thus in 2012(98%), 2013 (78.3%), 2014(82.5%),2015(85.3%) and 2016(88%) (Figure 2 and Table 3).
Figure 2: Treatment Success rate across Years, Northwest Ethiopia, 2012 -2016.
| Characteristics |
Treatment outcome |
Cured
N (%) |
Rx completed
N (%) |
Defaulter
N (%) |
Died
N (%) |
RX Failure
N (%) |
Transfer out
N (%) |
Moved to MDR
N (%) |
Total
N (%) |
| Age |
| 0-4 |
* |
71(8.5) |
4(0.5) |
3(0.4) |
1(0.1) |
2(0.2) |
* |
81(9.7) |
| 15-24 |
28(3.4) |
205(24.6) |
5(0.6) |
7(0.8) |
5(0.6) |
29(3.5) |
1(0.1) |
280(33.6) |
| 25-34 |
51(6.1) |
133(15.9) |
5(0.6) |
4(0.5) |
1(0.1) |
12(1.5) |
4(0.5) |
210(25.2) |
| 35-49 |
20(2.4) |
110(13.3) |
5(0.6) |
8(0.9) |
2(0.2) |
20(2.4) |
3(0.4) |
168(20.2) |
| >50 |
10(1.2) |
58(6.9) |
3(0.4) |
4(0.5) |
1(0.1) |
16(1.9) |
2(0.2) |
93(11.8) |
| Sex |
| Male |
55(6.5) |
306(36.5) |
12(1.5) |
16(1.8) |
5(0.6) |
48(5.8) |
8(0.9) |
450(53.6) |
| Female |
54(6.6) |
271(32.8) |
9(1.1) |
10(1.3) |
5(0.6) |
31(3.7) |
2(0.2) |
382(46.4) |
| Residence |
| Urban |
87(10.4) |
354(42.5) |
4(0.5) |
12(1.5) |
3(0.4) |
54(6.5) |
1(0.1) |
515(61.9) |
| Rural |
22(2.6) |
223(26.8) |
17(2.1) |
14(1.7) |
7(0.8) |
25(3.0) |
9(1.1) |
317(38.1) |
| TB Type |
| PTB |
100(12.0) |
306(36.8) |
5(0.7) |
14(1.7) |
4(0.5) |
30(3.6) |
6(0.7) |
465(55.9) |
| EPTB |
9(1.1) |
271(32.6) |
16(1.9) |
12(1.5) |
6(0.7) |
49(5.9) |
4(0.5) |
367(44.1) |
| |
RX: Treatment; PTB: Pulmonary Tuberculosis; EPTB: Extraplumonary Tuberculosis;*: Not Applicable; MDR: Multi-Drug Resistance
Table 3: Treatment outcome of TB patients (n=832) by sex, age group, residence and tuberculosis type at Buriezuria, Jabitehinan and Fenoteselam town health facilities, Northwest Ethiopia, 2012 to 2016.
Factors associated with tuberculosis treatment outcome
In multivariable logistic regression model, the odds of HIV negative TB patients were about four times more likely to have successful treatment outcome than the odds of TB patients with unknown HIV sero-status (AOR=4.4(1.83,10.79)). The odds of study subjects whose age group is<14 years(AOR=3.6(1.56,8.57)), 15-24 years (AOR=1.9(1.09,3.54)) and 25-34 years of age (AOR=2.6(1.40,5.15)) were about two, four and three times more likely to have successful treatment outcome compared with those age group >50 years of age respectively. Urbandwellers were two times more likely to have successful treatment outcome compared to their rural counterparts (AOR=2.2(1.50,3.33)). Pulmonary tuberculosis patients were also three times more likely to have successful treatment outcome(AOR=2.9(2.00,4.46)) compared to when compared to EPTB patients (Table 4).
| Variables |
Successful Treatment=686 |
Unsuccessful Treatment=146 |
Total |
COR (95% CI) |
AOR (95% CI) |
| |
(N=832) |
| Sex |
| Male |
361 |
89 |
450 |
0.7(0.49,1.02) |
0.72(0.46,1.06) |
| Female |
325 |
57 |
382 |
1 |
1 |
| Residence |
| Urban |
441 |
74 |
515 |
1.7(1.22,2.51) |
2.2(1.50,3.33) * |
| Rural |
245 |
72 |
317 |
1 |
1 |
| Age in (years) |
| <=14 |
71 |
10 |
81 |
2.6(1.14,5.84) |
3.6(1.56,8.57) * |
| 15-24 |
233 |
47 |
280 |
1.8(1.04,3.17) |
1.9(1.09,3.54) * |
| 25-34 |
184 |
26 |
210 |
2.8(1.40,4.81) |
2.6(1.40,5.15) * |
| 35-49 |
130 |
38 |
168 |
1.2(0.71,2.25) |
1.3(0.74,2.57) |
| >=50 |
68 |
23 |
93 |
1 |
1 |
| TB type |
| PTB |
406 |
59 |
465 |
2.1(1.48,3.07) |
2.9(2.00,4.46) * |
| EPTB |
280 |
87 |
367 |
1 |
1 |
| HIV Status |
| Positive |
106 |
30 |
136 |
2.5(1.01,6.25) |
1.9(0.74,5.13) |
| Negative |
566 |
106 |
672 |
3.8(1.65,8.81) |
4.4(1.83,10.79) * |
| Unknown status |
10 |
14 |
24 |
1 |
1 |
| |
*Significant at |
P value <0.05 |
|
|
|
Table 4: Association between Different Factors and Treatment Outcome among Tuberculosis Patients (N=832), North West Ethiopia, 2012-2016.
Discussion
In this study, we evaluated the treatment outcomes of 832 TB patients who registered at Buriezuria, Jabitehinanand Fenoteselam Administrative town health facilities DOTS clinic over a period of 5 years. Statistically gender had no significant difference on treatment outcome. similarly, the study conducted in Addis Ababa, Ethiopia showed that no significance difference between male and female [2]. Whereas higher rate of males were defaulted than females and this was consistent with a study conducted in southern Ethiopia. The higher social interaction outside home and social isolation lead to TB treatment rejection, alcoholism and other related behaviors among males might contribute to their higher defaulter.A study conducted inNigeria reported that patient behavior and attitude about the diseases are the major factors affecting adherence to TB treatment [4].
Our study showed that 13.1% and 69.4% of TB patients attending DOTS were cured and completed the treatment. These account an overall treatment success rate of 82.5%which was similar with treatment success rates reported as 82.7% Addis Ababa, Ethiopia [2] but it was higher than the rates reported as to 26% at Felegehiwot referral hospital (33), 61.7% paithian India [12] and 73% in Euro Surveillance France [24].
There was yearly variation of treatment success rate from 2012 to 2016. The treatment success rate in the year 2016 was 88% which is in line with WHO international target of 87%(22). This could be taken as an indicator that TB treatment outcome has improvement[18].
The treatment success rate obtained from this study was slightly lower than those reported from Debretabor Hospital (87.1%) [30]. However, we noted that defaulter, death rate, failure rate, moved to MDR, and transfer out of (2.6%),(3.1%),(1.2%),(1.2%) and (9.5%) respectively. These constituted an overall unsuccessful TB treatment outcome rate of (17.6%) which was higher than unsuccessful treatment outcome reported from Enfranz Northwest Ethiopia (8.1%).This finding was almost similar to reports by some studies in the country [30, 33]. default rate was higher than study conducted in Addis Ababa(0.6%) (28).There were 1.2% treatment failures comparable with study conducted at Gondar Teaching Hospital(1.2%), Debreberhan Hospital(1.13%) and DebretaborHospital(0.96%) [29,30].
This study also found a death rate of 3.1% which was Comparable finding reported from the study conducted in Addis Ababa[27], Metema hospital northwest Ethiopia[17]. This is lower than study conducted in Fenoteselam district hospital 8.5% [31]. This may be due to difference in sample size and time difference.
The odds of patients age group < 14 years(AOR=3.6(1.56,8.57)), 15-24 years(AOR= 3.9, 95% CI (2.13, 7.63)) and 25-34years of age(AOR=1.9(1.09,3.54)) were four, four and two times more likely to have successful treatment outcome compared with the odds of age group >50 years of age respectivelywhich is supported by study conducted at Gondar University Hospital[9], andFelegehiwot Referral Hospital [12].
In this study, the odds of patients from urban dwellers were about two times more likely to have successful treatment outcome compared to the odds of rural counterparts (AOR=2.2(1.50,3.33)) which is in line with study conducted in Felegehiwot referral Hospital 2013 [12].
In this finding,the odds of Patients with Pulmonary tuberculosis patients were about three times more likely to have successful treatment outcome(AOR=2.9(2.00,4.46)) compared to the odds of EPTB patients. It is in line with studies conducted in Felegehiwot referral hospital, 2016 [32-34],west Gojjam zone [31].
HIV infection increases the chance of tuberculosis reactivation and infection [13]. In the present study, the prevalence of HIV among TB patients was 16.8%.This was higher rate reports from different parts of Ethiopia such as Enfranz 11.7% [17], and studies conducted in south region. However, the present study TB-HIV co infection was lower than previous reports from different health centers at Addis Ababa, Metema Hospital, and Felegehiwot Referral Hospital 27.2%, 20.1% and 25% [28,31,32] respectively. TB-HIV co infection in present study(16.8%) was also lower than in the WHO estimate (39%) in Africa [1].
Twenty six (3.1%) study participants died during their course of their treatment. This report was consistent with reports from Enfranz Health Center(3.6%)[17] and different health centers in Addis Ababa 2011(3.7%)[28] and Nigeria(3.9%) [4].
The death rate among TB-HIV co-infection was 57.6%, the failure rate was 28.5%, and defaulted rate was 0.23%, indicating that extraordinary care to HIV-positive TB cases is required in the study region. This study presented that the treatment success rate for HIV negative tuberculosis patients 68.9% was higher than for HIV positive patients 11.6%.
Limitation of the Study
The finding of this study should see insight of the fact that the study incorporated data of patients with complete information of their treatment outcome at selected health facilities. Important socio-demographic Variables, which could affect TB treatment outcome including, co morbidity with other chronic illness, distance from the treatment center, educational status of the patients, nutritional history of patients were not obtained thus they were not included in the analysis. Hence these limitations need to be considered during while interpreting the finding.
Conclusion
In this study, the overall treatment success rate was still below WHO Target of Success rate, 87% and the trend of treatment success rate showed varying across the study periods.Patients who are HIV negative, whose age<14 years, whose age 15-24 years, 25-34years,urban residents and those having Pulmonary tuberculosis TB patients were identified associated factors for successful tuberculosis treatment outcome.
Acknowledgments
we want to say thank you to the district health offices and health institutions those who allow the data for analysis.
Ethical approval
Bahirdar University college medicine and health sciences Institutional review board allow this research to be done.
Conflicts of Interest
The author declare that they have no conflicts of interest
References
- Tingstveit HO, Kleiva GD (2013) TB Management in Bahir Dar, Ethiopia: are we doing things right.
- Hailu D, Abegaz WE, Belay M (2014) Childhood tuberculosis and its treatment outcomes in Addis Ababa: a 5-years retrospective study. BMC pediatrics 14(1):1.
- Kebede A (2014) The first population-based national tuberculosis prevalence survey in Ethiopia, 2010-2011. Int J Tuberc Lung Dis 18(6): 635-9.
- Erah P, Ojieabu W (2009) Success of the control of tuberculosis in Nigeria: A review. Int J Med Sci Public Health 2(1): e214p19-32.
- Organization WH (2015) Global tuberculosis report 2015. 2015: World Health Organization.
- Lorena Cristina S (2012) Review the molecular basis of resistance in Mycobaterium tuberculosis. Open Journal of Medical Microbiology, 2012.
- Keeler E (2006) Reducing the global burden of tuberculosis: the contribution of improved diagnostics. Nature 444: 49-57.
- vanHest R (2013) Tuberculosis treatment outcome monitoring in European Union countries: systematic review. Eur Respir J 41(3): 635-43.
- Tessema B (2009) Treatment outcome of tuberculosis patients at Gondar University Teaching Hospital, Northwest Ethiopia: A five-year retrospective study. BMC public Health 9(1): 1.
- Vasankari T (2007) Risk factors for poor tuberculosis treatment outcome in Finland: a cohort study. BMC public health 7(1): 1.
- Liu JH Yao, Liu E (2005) Analysis of factors affecting the epidemiology of tuberculosis in China.Int J Tuberc Lung Dis 9(4): 450-4.
- Organization,W.H.O Global status report on alcohol and health. 2014:World Health Organization.
- Duthey B (2013) Priority medicines for europe and the world:“a public health approach to innovation”.
- World Health Organization (2010) The global plan to stop TB 2011-2015: transforming the fight towards elimination of tuberculosis.
- Getahun B (2013) Treatment outcome of tuberculosis patients under directly observed treatment in Addis Ababa, Ethiopia. Braz J Infect Dis17(5):521-8.
- Chaulk CP, Kazandjian VA (1998)Directly observed therapy for treatment completion of pulmonary tuberculosis: Consensus Statement of the Public Health Tuberculosis Guidelines Panel. Jama 279(12): 943-8.
- Endris M (2014) Treatment outcome of tuberculosis patients at Enfraz Health Center, Northwest Ethiopia: a five-year retrospective study. Tuberc Res Treat.
- Uplekar M (2015) WHO's new End TB Strategy. The Lancet385(9979):1799-1801.
- Ethiopia Ministry of Health (2016) Emoh, national comprehensive tuberculosis, leprosy and tb/hiv training manual for health care workers.
- World Health Organization (2008) G.T.Programme, Global Tuberculosis Control: WHO Report.
- Bao QS, Du YH, Lu CY (2007) Treatment outcome of new pulmonary tuberculosis in Guangzhou, China 1993–2002: a register-based cohort study. BMC Public Health 7(1): 1.
- World Health Organization (2013) Global tuberculosis report 2013.
- Karanjekar V (2014) Treatment Outcome and Follow up of Tuberculosis Patients Put on Directly Observed Treatment Short:Courseunder Rural Health Training Center, Paithan, Aurangabad in India. Ann Med Health Sci Res 4(2): 222-6.
- Van der Werf , Sprenger M (2013) Joint efforts needed to stop transmission of tuberculosis in Europe. Euro surveillance: bulletin EuropeÃÅÃÂensur les maladies transmissibles European communicable disease Bulletin18:1-12.
- Klocke R, Sylvester A (1994) The American Journal of Respiratory and Critical Care Medicine. Am J Respir Crit Care Med 149(1):1-2.
- Mashimbye L (2010) Tuberculosis (TB) treatment outcomes in adult TB patients attending a rural HIV cllinic in South Africa (Bushbuckridge), 2010.
- Tilahun G, Gebre-Selassie S (2016) Treatment outcomes of childhood tuberculosis in Addis Ababa: a five-year retrospective analysis. BMC Public Health16(1): 612.
- Deribew A (2011) Investigation outcomes of tuberculosis suspects in the health centers of Addis Ababa, Ethiopia. PLoS One 6(4): e18614.
- Tefera F, DejeneT, Tewelde T (2016) Treatment Outcomes of Tuberculosis Patients at Debre Berhan Hospital, Amhara Region, Northern Ethiopia. Ethiop J Health Sci 26(1):65-72.
- Melese A, Zeleke B, Ewnete B (2016) Treatment Outcome and Associated Factors among Tuberculosis Patients in Debre Tabor, Northwestern Ethiopia: A Retrospective Study. Tuberculosis Research and Treatment.
- Gebreegziabher SB, Yimer SA, Bjune GA (2016) Tuberculosis case notification and treatment outcomes in West Gojjam Zone, Northwest Ethiopia: a five-year retrospective study. J Tuberc Res 4(1): 23.
- Zenebe Y (2016) Profile of tuberculosis and its response to anti-TB drugs among tuberculosis patients treated under the TB control programme at Felege-Hiwot Referral Hospital, Ethiopia. BMC Public Health 16(1): 688.
- Biadglegne F (2013)A retrospective study on the outcomes of tuberculosis treatment in Felege Hiwot Referral Hospital, Northwest Ethiopia. Int J Med Sci Public Health 5(2): 85-91.
- Kochi A (2001)The global tuberculosis situation and the new control strategy of the World Health Organization. Bull World Health Organ 79(1): 71-75.