Review Article - (2017) Volume 3, Issue 5
Burton Ashworth*
College of Business and Behavioral Science, University of Louisiana, Monroe, USA
*Corresponding Author:
Burton Ashworth
Assistant Professor
College of Business and Behavioral Science
University of Louisiana
Monroe, USA
Tel: 318-342-1439
E-mail: ashworth@ulm.edu bashworth1@lsco.edu
Received Date: August 24, 2017; Accepted Date: September 04, 2017; Published Date: September 12, 2017
Citation: Ashworth B (2017) The Role of Difficult Childhood Behaviors on Intimate Partner Violence. Acta Psychopathol. 3:60. doi: 10.4172/2469-6676.100132
The relationship between family stress (FS) and intimate partner violence (IPV) is well established, but whether the presence of a difficult child moderates the relationship between FS and later IPV was unclear. To fill this important gap in the literature, data from the Longitudinal Studies of Child Abuse and Neglect (LONGSCAN) database were used to determine whether child difficulty (CD) and family stress at child age 6 interact in the prediction of IPV at child age 8. In a parallel analysis to replicate findings, the interaction between child difficulty and family stress at child age 12 was assessed in the prediction of IPV at child age 14. Hypotheses were tested using multiple linear regression at the p<0.05 threshold for statistical significance. Analyses controlled for child gender at child age 6 and for child gender, caregiver depression, substance abuse in the household and household SES at child age 12. The moderator hypothesis was validated in the research when predicting from child difficulty and family stress at child age 6 to IPV at child age 8 and also statistically significant at child age 12 to IPV at child age 14. These findings have important implications in assisting mental health providers with developing novel interventions, which may help reduce IPV. Further examination of the impact difficult behavior of a child may contribute to family stress may enhance our ability to reduce partner engagement in violence and its indirect psychosocial sequelae.
Keywords
Intimate partner violence; IPV; Child difficulty; Family stress; Domestic violence; Gender; Longitudinal; LONGSCAN
Introduction
At the outset, it is important to offer a disclaimer for the scope and focus of this project. The purpose of this project is not to place blame on the child for the activation of violent behavior between partners within a domicile. Children should not feel the weight of any suggestion of guilt for being the cause of violent behavior between those whose privileged responsibility is to create a nurturing and secure habitat for their offspring. Attempting to indicate in any form or fashion that the behavior of a child is the cause of intimate partner violence (IPV) is inappropriate on many levels. However, finding how the presence of a child impacts the family dynamic is justified, in order to develop IPV interventions that may ultimately lead to a better home life for all members of the family system.
Assuredly, there is a need for further research investigating between-partner dysfunctional domestic behavior and its impact on children. Nonetheless, the standing research focuses on a unilateral perspective from caregiver toward child. Undeniably, intimate partner violence impacts the behavior [1], development [2,3] and emotions [4,5] of children. Without suggesting that children are a causal effect for IPV, it is important to change the perspective of flow of effect from caregiver toward child and investigate if there is a flow of effect from the child toward the caregiver. Anyone who has experienced the presence of a child suffering with an illness such as colic can wholeheartedly agree that the behaviors of the infant negatively impact all participants near the child. Research indicates the vocalization of the distress of an infant significantly impact all adults within hearing, both physiologically and psychologically [6-8]. Therefore, it is plausible that the presence of a child experiencing an exceptionality may have a mediating effect on IPV.
Intimate Partner Violence (IPV) is a national epidemic, affecting millions of cohabiting partners [9]. Having a large number of stressors in a home increases the likelihood of incidents of IPV [10]. Family stress elicits violence ranging from verbal assault, to shoving a partner, to the use of a lethal weapon [11]. Family stress may come from marital discord [12], caregiver depression [13,14], substance abuse in the household [15,16], low economic resources [17], minimal social support [18] and occupational difficulties [19,20]. Research suggests lack of social support, low socio-economic indicators, and educational levels impact relationship distress [21], as well as IPV prevalence [22]. While the empirical link between family stress and IPV is well established, less is known regarding the role of a difficult child in the relationship between family stress and IPV. Child difficulty may express as social withdrawal, somatic complaints, anxiety/ depression, social problems, thought problems, attention problems, delinquent behavior, or aggressive behavior [23-25]. The American Psychiatric Association (APA) identifies various diagnoses across the developmental spectrum for children [26], including disabilities in learning, motor skills, communication, pervasive development, feeding and eating, elimination and attachment to caregiver, as well as criteria for identifying attention deficit hyperactivity disorder (ADHD), disruptive behavior disorders, mood disorders, and posttraumatic stress disorder (PTSD), that contribute to identification as a difficult child.
A difficult child can increase family stress. Children whose behaviors are impacted by an organic etiology or general medical condition can increase caregiver stress levels [23,27]. Further, delinquent behavior and emotional distress in children are directly related to the presence of stressors among caregivers [28,29], which may contribute to negative behavior between caregivers [30,31]. There is a positive correlation between difficult childhood behavior and caregiver frustration and dissatisfaction [28,32]. Developmental disability in a child can also have a significant impact on caregiver stress [33,34], often resulting in severe complications in the caregivers’ primary relationship [35,36]. In summary, maladaptive characteristics in children are a major factor in caregiver stress [37]. Difficult childhood traits and behaviors that require increased caregiver attention may increase marital discord, and marital discord may eventually result in IPV [31,38]. However, no studies to date have investigated the effect of a difficult child on later IPV between caregivers.
Methods
Using the Longitudinal Studies of Child Abuse and Neglect (LONGSCAN) database, a linear regression methodology determined whether difficulty in a 6 year old child might interact with (“energize”) family stress towards the prediction of later intimate partner violence (IPV) at age 8, above the effects of descriptor covariates. Additionally, this research explored whether family stress and the age 12 child difficulty might interact to predict IPV at child age 14. Factors known to impact the marital relationship or to predict IPV; caregiver depression, substance abuse in the household, and low socioeconomic status [39-41] served as control variables. Using a statistical model of moderator [42-44], the hypothesis was supported if and only if the family stress x child difficulty interaction was statistically significant at the p<0.05 threshold.
Participant data for this study came from the LONGSCAN project database. LONGSCAN is a multi-regional consortium of research sites using common assessment measures, instruments, diagnostic criteria, and data collection methods to study antecedents and consequences of various influences associated with families [45]. LONGSCAN was designed to be ethnically and regionally diverse across east, midwest, northwest, south and southwest regions. The method of data gathering included face-to-face interviews with primary caregiver and child every two years.
Participants and procedure
Selection criteria for the archival data included (a) the child at age 6 lived in home with at least two caregivers, and (b) the data were sufficiently complete for home condition measures at age 6 years (child gender, Everyday Stressors Index, Child Behavior Checklist) and a measure of IPV (Conflict Tactics Scale: Partner to Respondent Physical Aggression) at age 8. Inclusion criteria for children were also included if (a) the child at age 12 lived in a home with at least two caregivers, and (b) the data are sufficiently complete for home condition measures at age 12 years (Self-Report Family Inventory, Child Behavior Checklist, Center for Epidemiological Studies Depression Scale, Risk Behaviors of Family and Friends, and Caregiver Demographics: family income) and a measure of IPV (Conflict Tactics Scale: Physical Aggression) at age 14.
Cases met exclusion criteria if the child at age 6 or age 12 did not live in a home with two caregivers, or (b) the data are not sufficiently complete for associated home condition measures at age 6 or age 12 years (Everyday Stressors Index, Self-Report Family Inventory, Child Behavior Checklist, Center for Epidemiological Studies Depression Scale, Risk Behaviors of Family and Friends, and family income) or a measure of IPV (Conflict Tactics Scale) at age 8 or age 14.
One thousand three hundred fifty four children were examined for inclusion in these studies. The current sample for the study of six year olds consists of three hundred twenty participants (144 males and 176 females) which met inclusionary criteria.
Instruments
Child difficulty was assessed by the Child Behavior Checklist (CBCL). The CBCL was specifically designed to identify problem behaviors in children [46,47]. For the syndrome scales, T scores less than 67 are considered in the normal range, T scores ranging from 67-70 are considered to be borderline clinical, and T scores above 70 are in the clinical range. Among the eight syndromes, Cronbach’s alpha values ranged from 0.62 to 0.92 for boys and from 0.66 to 0.92 for girls. Evidence for content, construct, and criterion-related validity is well documented.
Family stress was measured using the Everyday Stressors Index (ESI) [48] for child age 6.
Response options include: 1=not at all bothered; 2=a little bothered; 3=somewhat bothered; 4=bothered a great deal; and 5=don’t know. A higher score indicates a higher level of daily stress. High internal consistency of the index was reported, with a Cronbach’s alpha of 0.83 [49].
The Self Report Family Inventory (SFI) conflict scale was chosen as the measure of family stress because the SFI conflict scale is composed of 12 items dedicated to conflict [50]. Respondents are asked to rate each statement (e.g., “We all have a say in household plans”) on a 5-point scale ranging from 1 (fits our household very well) to 5 (doesn't fit our household at all).
Lower scores represent greater competence on all SFI scales. Beavers and associates [51] reported alpha reliability coefficients for the entire scale ranging from 0.84 to 0.88. Test-retest reliability coefficients (for 30 to 90 days) ranged from 0.84 to 0.87 for Family Health/Competence, 0.50 to 0.59 for Conflict, 0.50 to 0.70 for Cohesion, 0.79 to 0.89 for Expressiveness, and 0.41 to 0.49 for Directive Leadership. 50 Convergent and concurrent validity have been demonstrated through comparisons to other assessments of family functioning, such as FACES II and FACES III, [52] and the Beavers Interactional Scales [51].
Conflict Tactics Scale Partner to Partner Physical Aggression was used as the measure of IPV at child age 8 and the sum of the Conflict Tactics Scale aggression items was used as the measure of IPV at child age 14. The sub scale used for this study was Physical Assault (items 4, 5, 9, 23, 27, 11, 14, 17, 19, 22, 31, and 37). Physical Assault can be separated into two sub scales, minor (items 4, 5, 9, 23, and 27) and severe (items 11, 14, 17, 19, 22, 27, and 31). We used a dichotomous score indicating the presence of physical assault or absence of physical assault. We did not consider the severity of assault. Internal consistency reliability of the subscales ranging from 0.79 to 0.95. Construct validity of the CTS has been demonstrated in a number of studies [53]. Concurrent validity was examined by comparing reports obtained separately from husbands and wives. Husband-wife correlations are reported to range from 0.19 to 0.80, with a mean of approximately 0.40 [54].
The Risk Behaviors of Family and Friends survey (RBFF) [55] was used in the study to assess drug and alcohol use in the household at child age 12. Nine items assess the youth’s perception of the type of household members’ substance use and the frequency with which a household member is either drunk or high. Substances of interest include tobacco, alcohol and a range of illegal drugs.
The Center for Epidemiological Studies Depression Scale (CESD) was used to measure depressive symptoms of the caregiver. The instrument has 20 items comprising six scales that reflect the major dimensions of depression: depressed mood, feelings of guilt and worthlessness, feelings of helplessness and hopelessness, psychomotor retardation, loss of appetite, and sleep disturbance [56]. Response categories indicate the frequency of occurrence of each item, and are scored on a 4- point scale ranging from 0 (rarely or none of the time) to 3 (most or all of the time). High internal consistency has been reported with Cronbach’s alpha coefficients ranging from 0.85 to 0.90 across studies and substantial evidence of construct validity, has been demonstrated [57].
The Caregiver Demographics is a descriptive measure used to determine total household income, a measure of socioeconomic status, which was used as a control variable for child age 12 in the present study. Occupational status is scored using the 9-point Hollingshead Occupational Scale [58]. Education was measured by number of years of schooling as well as by degrees or certification earned. Annual income was measured in $5,000 increments, up to more than $50,000 per year.
This study complied with the ethical guidelines of Fielding Graduate University and the APA, including confidentiality and anonymity. All data were collected from the LONGSCAN archival database after informed consent was acquired [45]. Data were kept confidential. Codes were used so that all analyses could be conducted blinded to participant identification.
Results
Participants
Child participants at age six years included a frequency of 144 males, comprising 45% of the children, and 176 females, making up 55% of the individuals in the test parameters.
The CBCL total problems scale was significantly correlated with ESI (r=0.43, p<0.0001) and with CTS physical aggression (r=0.22, p<0.0001). ESI was significantly correlated with CTS physical aggression (r=0.28, p<0.0001).
The findings demonstrate that CBCL Child Problems, family stress (ESI), and IPV (CTS Partner to Respondent Physical Aggression) were all correlated in the positive direction, such that higher scores on one scale were associated with higher scores on the other scales. Gender was not significantly correlated with CBCL Total Problems, ESI, or CTS Physical Aggression (each p>0.05).
Multiple regression: testing moderation for study 1
Multiple regression was conducted to determine whether child difficulty, as inferred from the standardized CBCL total problems scale, might moderate the relationship between family stress, as inferred from the ESI, and IPV, and the CTS partner to respondent physical aggression scale.
For these analyses, CTS partner to respondent physical aggression at child age 8 was the dependent variable, ESI at child age 6 was the independent variable, and CBCL total problems scale at child age 6 was the moderator variable. The interaction between ESI and CBCL total problems scale was included as a predictor variable because the moderator hypothesis is tested by determining whether the interaction of the independent variable and the moderator variable is statistically significant. Gender was included as a variable in these analyses.
Based upon the recommendations of Aguinis and Gottfredson [42], the four moderator procedure steps that were used in this study were:
1. Center scores on the moderator and independent variables prior to computing their product.
2. Compute the product of the centered moderator and independent variables.
3. Perform a regression analysis entering the predictors in two blocks, with the first block containing the centered moderator and centered independent variable and the second block containing the product term.
4. If the entry of the product term in the second block of the model results in a statistically significant change in R2, this is interpreted as moderation.
For the present study, the moderator (child problems) and independent (family stress) variables were centered before computing their product to make the interaction term, consistent with step 1 and step 2 [42]. Consistent with step 3, multiple regression predictors were entered in two blocks, first with the independent and moderator variables in the first block (model), then with the interaction product term added in the second block (model 2). Consistent with step 4, the change in R2 from block (model) 1 to block (model) 2 was assessed for statistical significance, which would be interpreted as evidence of moderation.
For model 1 (what Aquinis & Gottfredson [42] term “block 1”), Table 1 shows that the combination of child gender, child problems (CBCL) and family stress (ESI) accounted for 9% of the variance in IPV (CTS) (R2=0.09). For model 2 (“block 2”), Table 2 shows that adding the child problems x family stress interaction to the combination of child gender, child problems (CBCL) and family stress (ESI) improved the R2 to 0.12. This improvement in R2 from 0.09 to 0.12 was statistically significant, F (1, 315)=10.75, p<0.001, supporting the hypothesis that child problems moderates the relationship between family stress and IPV.
| 95% CI for B | |||||||
|---|---|---|---|---|---|---|---|
| Independent Variables | B | SEb | Beta | t | P | CI LL | CI UL |
| Gender | -0.055 | 0.286 | -0.010 | -0.192 | 0.848 | -0.617 | 0.508 |
| Child Problems (CBCL) | 0.032 | 0.015 | 0.125 | 2.103 | 0.036 | 0.002 | 0.062 |
| Family Stress (ESI) | 0.062 | 0.016 | 0.227 | 3.819 | 0.0001 | 0.030 | 0.094 |
Notes: B=unstandardized beta; SEb=standard error of beta; Beta=standardized beta; t=t-value; p=p-value; CI LL=confidence interval lower level; CI UL=confidence level upper level R2=0.09, F(3, 316)=10.72, p<0.0001. N=320.
Table 1: Regression coefficients for child age 6, without child problems x family stress interaction.
| 95% CI for B | |||||||
|---|---|---|---|---|---|---|---|
| Independent Variables | B | SEb | Beta | t | P | LL | UL |
| Gender | -0.020 | 0.281 | -0.004 | -0.070 | 0.944 | -0.572 | 0.533 |
| Child Problems (CBCL) | 0.037 | 0.015 | 0.144 | 2.462 | 0.014 | 0.007 | 0.067 |
| Family Stress (ESI) | 0.042 | 0.017 | 0.155 | 2.514 | 0.012 | 0.009 | 0.076 |
| Child Problems x Family Stress | 0.005 | 0.001 | 0.204 | 3.656 | 0.0003 | 0.002 | 0.008 |
Note: R2=0.12, F(4, 315)=11.70, p<0.0001. N=320.
Table 2: Regression coefficients for the child age 6, with child problems x family stress interaction.
Note that Table 1 and Table 2 show that both family stress and child problems were significantly associated with IPV, where the Child Problems x Family Stress interaction was included (Table 2) but not (Table 1). This finding shows that family stress and child problems are each associated with IPV in addition to the observation that their interaction is significantly related to IPV.
This interaction between child problems and family stress is visually displayed in Figure 1:
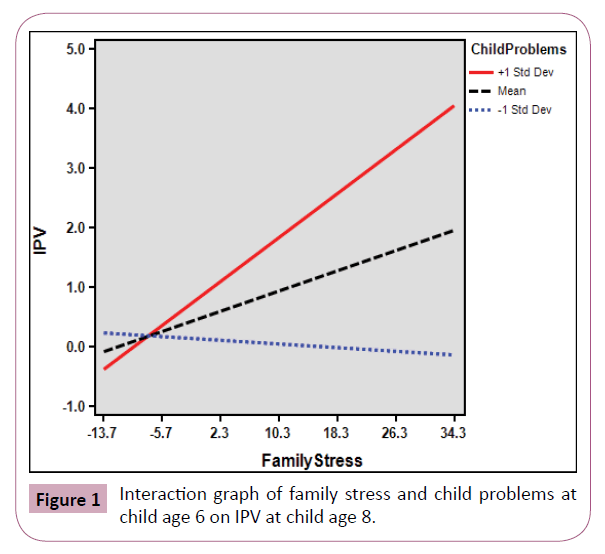
Figure 1: Interaction graph of family stress and child problems at child age 6 on IPV at child age 8.
The dashed line shows the mean relationship between family stress and IPV across levels of child problems. The solid line shows that, for CBCL at 1 standard deviation above the mean, higher CBCL scores were associated with an increase in IPV, while the dotted line shows that, for CBCL scores 1 standard deviation below the mean, family stress was negatively associated with IPV.
Descriptive for child age 12
Child participants at age 12 years included a frequency of 145 males, comprising 52% of the children, and 132 females, making up 48% of the individuals in the test parameters.
The CBCL total problems scale was significantly correlated with ESI (r=0.43, p<0.0001) and with CTS physical aggression (r=0.22, p<0.0001). ESI was significantly correlated with CTS physical aggression (r=0.28, p<0.0001).
The findings demonstrate that CBCL Child Problems, family stress (ESI), and IPV (CTS Partner to Respondent Physical Aggression) were all correlated in the positive direction, such that higher scores on one scale were associated with higher scores on the other scales. Gender was not significantly correlated with CBCL Total Problems, ESI, or CTS Physical Aggression (each p>0.05) (Table 3).
| # | Observed | Potential | |||||
|---|---|---|---|---|---|---|---|
| Variables | Items | N | M | SD | Range | Range | α |
| Child Problems (CBCL) | 120 | 277 | 55.44 | 11.10 | 23-91 | 23-100 | 0.62-0.92 |
| Family Stress (SFI) | 36 | 277 | 1.61 | 0.53 | 1-4.17 | 1-5 | 0.50-0.59 |
| IPV (CTS PA: P→R) | 19 | 277 | 1.52 | 3.54 | 0-19 | 0-∞ | 0.69-0.88 |
| Depression (CEDS) | 22 | 277 | 11.94 | 9.97 | 0-49 | 0-50 | 0.85-0.90 |
Note: alphas (α) reflect values from the LONGSCAN manual (Hunter et al., 2003).
aChild Behavior Checklist (CBCL)
bEveryday Stress Index (ESI)
cConflict Tactics Scale, Partner to Respondent: Physical Assault at Child Age 14
dThe Center for Epidemiological Studies Depression Scale (CESD)
Table 3: Variable distributions of child age 12 data: child problemsa, family stressb & depressiond at child age 12, and IPVc at child age 14.
Correlations
The CBCL total problems scale was significantly correlated with SFI (r=0.44, p<0.0001) and with CTS (r=0.26, p<0.0001). SFI was significantly correlated with CTS (r=0.27, p<0.0001). These findings demonstrate that Total Problems, SFI, and Aggression were all significantly correlated in the positive direction, such that higher scores on one scale were associated with higher scores on the other scales.
Multiple regression: testing moderation for study 2
Multiple regression was conducted to determine whether child difficulty, as assessed by the normalized CBCL total problems scale, might moderate the relationship between family stress, determined from the ESI, and IPV, and inferred from the average CTS score.
For this analysis, CTS score was the dependent variable, SFI was the independent variable, and CBCL total problems scale was the moderator variable. Control variables included gender, family income (SES), and drug abuse. The interaction between the SFI and the CBCL was included as a predictor variable because the moderator hypothesis is tested by determining whether the interaction of the independent variable (family stress) and the moderator variable (total problems scale) is statistically significant.
For model 1, Table 4 shows that the combination of child gender, family income, maternal depression, drug abuse, child problems (CBCL) and family stress (ESI) accounted for 11% of the variance in IPV (CTS) (R2=0.11). For model 2, Table 5 shows that adding the child problems x family stress interaction improved the R2 to 0.13. This improvement in R2 from 0.11 to 0.13 was statistically significant, F(1, 269)=7.34, p<0.007, supporting the hypothesis that child problems moderate the relationship between family stress and IPV. Note that the variance inflation factor was near 1 for this regression analysis, indicating no multicollinearity in this multiple linear regression model.
| 95% CI for B | |||||||
|---|---|---|---|---|---|---|---|
| Independent Variables | B | SEb | Beta | t | P | LL | UL |
| Gender | 0.524 | 0.408 | 0.074 | 1.286 | 0.200 | -0.279 | 1.327 |
| SES (Family Income) | -0.005 | 0.071 | -0.005 | -0.077 | 0.939 | -0.144 | 0.134 |
| Depression (CESD) | 0.010 | 0.024 | 0.027 | 0.408 | 0.684 | -0.037 | 0.056 |
| Drugs abuse (RBFF) | 0.780 | 0.626 | 0.073 | 1.247 | 0.214 | -0.452 | 2.013 |
| Child Problems (CBCL) | 0.050 | 0.021 | 0.156 | 2.325 | 0.021 | 0.008 | 0.092 |
| Family Stress (SFI) | 1.19 | 0.441 | 0.179 | 2.700 | 0.007 | 0.322 | 2.058 |
Note: R2=0.11, F(6, 270)=5.5, p<0.0001. N=277.
Table 4: Regression coefficients for child age 12 without child problems x family stress interaction.
| 95% CI for B | |||||||
|---|---|---|---|---|---|---|---|
| Independent Variables | B | SEb | Beta | t | p | LL | UL |
| Gender | 0.513 | 0.403 | 0.072 | 1.273 | 0.204 | -0.280 | 1.307 |
| SES (Family Income) | -0.015 | 0.070 | -0.013 | -0.218 | 0.828 | -0.153 | 0.122 |
| Depression (CESD) | 0.010 | 0.023 | 0.029 | 0.448 | 0.655 | -0.035 | 0.056 |
| Drugs abuse (RBFF) | 0.730 | 0.619 | 0.069 | 1.179 | 0.240 | -0.489 | 1.948 |
| Child Problems (CBCL) | 0.058 | 0.021 | 0.183 | 2.730 | 0.007 | 0.016 | 0.101 |
| Family Stress (SFI) | 0.594 | 0.488 | 0.089 | 1.216 | 0.225 | -0.367 | 1.554 |
| Child Problems x Family Stress | 0.097 | 0.036 | 0.174 | 2.709 | 0.007 | 0.027 | 0.168 |
Note: R2=0.13, F(7, 269)=5.9, p<0.0001. N=277.
Table 5: Regression coefficients for child age 12 with child problems x family stress interaction.
This significant interaction between child problems and family stress on IPV is visually displayed in Figure 2. The striped black line (dashed line) shows the mean relationship between family stress and IPV across levels of child problems. The red line (solid line) shows that, for CBCL Child Problems at 1 standard deviation above the mean, higher CBCL scores were associated with an increase in IPV, while the blue dotted line shows that, for CBCL Child Problems scores 1 standard deviation below the mean, family stress was negatively associated with IPV.
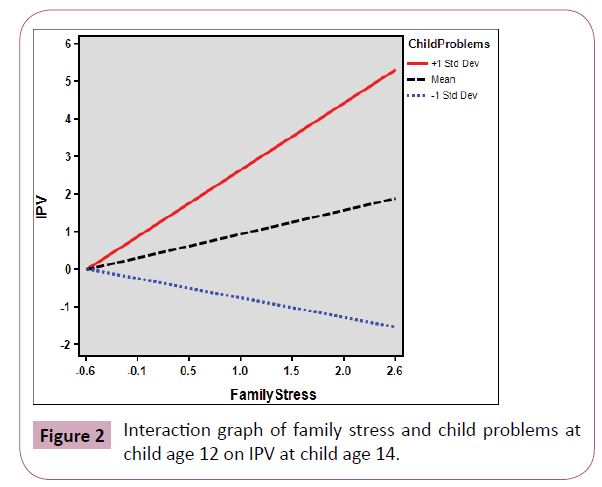
Figure 2: Interaction graph of family stress and child problems at child age 12 on IPV at child age 14.
Study 1: Child difficulty, family stress, and IPV prediction from age 6 to age 8
Child difficulty significantly interacted with family stress to predict later IPV. This moderator hypothesis was validated when predicting from child difficulty and family stress at child age 6 to IPV at child age 8. This finding was apparent above any effect of child gender.
Study 2: Child difficulty, family stress, and IPV prediction from age 12 to age 14
Child difficulty significantly interacted with family stress to predict later IPV. This moderator hypothesis was validated when predicting from child difficulty and family stress at child age 12 to IPV at child age 14. This finding was apparent above any effects of child gender or caregiver depression, substance abuse in the household, and SES.
Discussion
Family stress was associated with later IPV in the present study. This association was statistically significant across two child age cohorts and was robust to the measures used to assess family stress and to the inclusion of variables in the analysis. This relationship was statistically significant using simple correlation or using multiple regression and whether from family stress at child age 6 to IPV at child age 8 or from family stress at child age 12 to IPV at child age 14.
This finding of a significant positive relationship between family stress and IPV was consistent with published literature. For example, family stress has previously been shown to be associated with IPV, whether the family stress comes from poverty [59,60], negative emotionality [12], pregnancy [61,62], depression [62], alcohol or substance abuse [62,60] psychopathy [63], criminality [64], job stress [65,66] and low marital satisfaction [63,67,68]. The present findings extend previously published studies of IPV with concurrent family stress to include the observation that family stress can be predictive of later IPV, two years after the family stress was assessed.
Findings of the present study provide further evidence that the relationship between family stress and IPV may not be dependent on the source of the family stress. For example, family stress in the present study was associated with IPV when family stress was assessed using the Everyday Stressors Index (ESI) [48] at child age 6 and when family stress was assessed using the Self-report Family Inventory (SFI) [50] at child age 12. Although not conclusive, the present findings and the findings of others could be interpreted to suggest that family stress may be associated with IPV regardless of the source of the family stress or the standardized family stress measuring instrument. While not all measuring instruments may be suitable to measuring family stress, further research is needed to fully characterize the relationship between various sources of family stress and IPV.
Findings from the current study suggests the possibility that family stress has a general impact on IPV that might not be specific to the origination of the stress. These findings help to lend support to Bowen’s Family System theory. His theory suggests a multiplicity of avenues that could be used by participants in IPV behavior. One such avenue in Bowen’s Family System Theory is Triangles. In Triangle, during a unit crisis in which tension begins to rise between the caregivers, one may choose to diffuse the tension by moving from partner participation, to interaction with the third point of the triangle relationship; the child in the home. A submissive or passive child may allow that interaction to occur, thus allowing the caregiver’s tension to dissipate in a non-violent manner. However, if the child is obstinate, angry, resistant or any number of behaviors that may cause the child to refuse to accept any gesture from one of the members of the triangle, the person filled with tension, may return to the former altercation, reinstating the argument, which may lead to physical assault.
The finding of a significant moderation effect of child difficulty on the relationship between family stress and later IPV shows that child difficulty does more than merely add to family stress in IPV. Instead, family stress and child difficulty may multiply together in the prediction of later IPV risk.
It is important to note that the effect size of the family stress x child difficulty interaction was modest in magnitude, accounting for ~2% of the variance in IPV, and that standardized betas from multiple regression indicated that a one standard deviation increase in the family stress x child difficulty interaction was associated with a roughly one-fifth of a standard deviation increase in IPV at child age 8 and a roughly one-sixth of a standard deviation increase in IPV at child age 14.
The present study using the archival LONGSCAN database of child abuse and neglect was the first research focused on the role of a difficult child on the relationship between family stress and IPV, so future research and replications using more diverse samples is needed to fully characterize the magnitude of the moderating effect of child difficulty on the relationship between family stress and IPV.