- (2009) Volume 10, Issue 3
Omer Vedat Unalp1, Unal Aydin1, Pinar Yazici1, Deniz Nart2, Cigdem Yenisey3, Tulay Kavak3, Murat Zeytunlu1, Ahmet Coker1
Departments of 1General Surgery and 2Pathology, Ege University School of Medicine. Izmir, Turkey.
3Department of Biochemistry, Adnan Menderes University School of Medicine. Aydin, Turkey
Received September 27th, 2008 - Accepted March 16th, 2009
Objective The aim of this study was to evaluate the negative effects of the Pringle maneuver on pancreatic tissue with respect to the time of performing the maneuver. Moreover, the efficacy of octreotide therapy on pancreatic changes at the time of the Pringle maneuver was assessed. Animals Fifty male Wistar Albino rats were randomized into 5 groups. Design The groups were formed as follows: Group A: sham operation, Group B: Pringle maneuver for 30 min plus octreotide (PM30-OCT), Group C: Pringle maneuver for 60 min plus octreotide (PM60-OCT) and Group D: Pringle maneuver for 30 min plus 0.9 % saline solution (PM30-SS), Pringle maneuver for 60 min plus 0.9 % saline solution (PM60-SS, Group E). Main outcome measures Blood samples for the evaluation of both amylase and lipase levels were taken via the portal vein. Levels of glutathione, glutathione reductase, catalase, myeloperoxidase, nitric oxide, xanthine oxidase, malondialdehyde, tumour necrosis factor alpha (TNF-alpha), and interleukin-1 beta (IL-1 beta) were assessed in the excised pancreatic tissue. Results In the octreotide-treated groups, the catalase level was significantly higher in Group B (PM30-OCT) as compared to Group C (PM60-OCT). Amylase, lipase, NO and IL-1 beta levels were higher in Group C (PM60-OCT). In the saline solution-treated groups, the catalase level was significantly higher in Group E (PM60- SS) than in Group D (PM30-SS) while nitric oxide and glutathione levels were found to be significantly lower in Group E (PM60- SS) than in Group D (PM30-SS). Comparison of those groups using the Pringle maneuver for 30 minutes, the octreotide-treated group (Group B, PM30-OCT) was found to have a higher degree of edematous change than the saline-treated group (Group D, PM30-SS). Among the treatment groups, TNF-alpha expression decreased with increasing occlusion time. Conclusion In this study, pancreatic damage and the duration of the Pringle maneuver are directly proportional to each other. Moreover, the administration of octreotide prior to the Pringle maneuver contributed to the pancreatic damage.
Animal Experimentation; Octreotide; Pancreas, Exocrine; Reperfusion Injury
Acute pancreatitis may occur when factors involved in maintaining cellular homeostasis become unbalanced. The initiating event could be anything which injures the acinar cell and impairs the secretion of zymogen granules. The initiative factors include alcohol use, gallstones (causing approximately 80% of the cases), certain drugs, hyperlipidemia, ERCP and trauma. In up to 10% of cases, the cause of the pancreatitis remains unknown. Although the mechanisms destructive to pancreatic acinar cells are unknown, once a cellular injury pattern has been initiated, activated neutrophils exacerbate the problem by releasing superoxide (the respiratory burst) or proteolytic enzymes (cathepsins B, D, and G, collagenase and elastase). Finally, the release of cytokines, tumour necrosis factor-alpha (TNF-alpha), interleukin-6 (IL-6), and interleukin-8 (IL-8) by macrophages further mediates the local and/or systemic inflammatory responses. The pro-inflammatory cytokines, especially TNF and IL-1, play a critical role throughout the inflammatory period.
In addition, acute pancreatitis can begin in the postoperative period of various types of surgery, including hepatic surgery [1, 2]. Some reports have addressed the hyperamylasemia and pancreatitis states present after hepatic surgery and linked those to chronic liver disease or a prolonged Pringle maneuver [1, 3]. It has also been proven that the Pringle maneuver can induce pancreatic venous congestion, hyperamylasemia and pancreatitis occurring secondarily to total clamping of the pancreatic venous system [4]. Nevertheless, how the pancreas responds to congestion and acute elevation of portal venous pressure by portal vein occlusion is not well understood.
Currently, both therapeutic and prophylactic modalities have been targeted at protecting the pancreas against ischemia. The two most popular agents employed are somatostatin and its synthetic analogue octreotide. These drugs are administered in the case of pancreatitis and esophageal variceal bleeding with the aim of decreasing the portal pressure.
The purpose of this study was to evaluate the effects of the Pringle maneuver (which is a widespread procedure in hepatobiliary surgery) on pancreatic tissue. In addition, the efficacy of prophylactic octreotide therapy in the prevention of pancreatic complications was explored.
Animals
Fifty six-month-old male Wistar Albino rats (200-250 g each) were used in this study. All were housed in a temperature- and light-controlled environment, and fed water and rat food pellets ad libitum for 3 days before sham treatment or portal vein occlusion. After the blood and tissue samples were obtained, the rats were sacrificed using an overdose of anesthesia.
The rats were randomly allocated into five groups of 10 rats each. Anesthesia was induced by subcutaneous injection of ketamine hydrochloride and xylazine (80- 100 mg/kg and 10 mg/kg i.p.; 20-40 min of anaesthesia). Group A (control) underwent a sham operation of standard midline laparotomy. Groups B and D were respectively administered a subcutaneous injection of octreotide (OCT) and saline solution (SS: 0.9% NaCl) with a dose of 10 μ/kg 30 minutes before the surgery. Thereafter, they underwent a standard midline laparotomy, dissection of the portal structures, exposure of the portal vein proximal to its bifurcation, and portal vein occlusion with a bulldog clamp for 30 minutes. Thirteen minutes prior to the operation, Groups C and E also received a subcutaneous injection of octreotide and saline solution, respectively with a dose of 10 μ/kg, respectively. In these groups, however, the clamping of portal vein was carried out for 60 minutes. In all groups, after the sham operation or portal vein occlusion, an approximate 2 mL blood sample was taken from the portal vein just after the total clamping time, 30 minutes for Groups B (PM30- OCT) and D (PM30-SS) and 60 minutes for Groups C (PM60-OCT) and E (PM60-SS). The pancreas was then removed.
We did not include the reperfusion phase (release of portal clamping) as part of the study protocol for two reasons. In the presence of a reperfusion phase, pancreatic damage may not be detected due to a washout phenomenon. In addition, hepatic ischemiareperfusion injury may affect the pancreas by circulating the inflammatory mediators released from the liver. In this case, we may not be able to deduce whether the cause of the pancreatic damage is due to hepatic ischemia-reperfusion injury or portal venous flow occlusion
Biochemical Analysis
Determination of inorganic nitrate in serum was performed by a kinetic cadmium-reduction method according to Navarro-Gonzálvez [5]. Tissue-associated myeloperoxidase (MPO) activity was determined as reported by Suzuki et al. [6]. Xanthine oxidase (XOD) activity was assayed spectrophotometrically at 293 nm and 37°C with xanthine (Prajda and Weber) [7]. Catalase (CAT) was assayed following Aebi (1984), by the rate of decomposition of H2O2 at 240 nm [8]. For determination of cellular total glutathione (GSH), the colorimetric Beutler method [9] was used, and glutathione reductase (GR) activity was assayed using the method of Racker [10]. Blood amylase and lipase levels were measured with an auto-analyzer (C8000 Architect, Abbott, Abbott Park, IL, U.S.A.).
Histomorphological Analysis
After excision, each pancreas was fixed in a 10% formalin solution for 24 hours, embedded in paraffin, and sliced into 5 μm thick sections. For histomorphological analysis, the sections were stained with hematoxylin-eosin and then examined under a light microscope (BX40, Olympus, Tokyo, Japan). Classification of edema and infiltration of inflammatory cells was carried out according to Merriam et al. [11].
Immunohistochemical Analysis
For immunohistochemical analysis of the inflammation, the sections were deparaffinized in xylene, rehydrated, and incubated with primary antibodies to TNF-alpha (IBL Co., Ltd. Gunma, Japan; catalog number 17194) and IL-1 beta (IBL Co., Ltd. Gunma, Japan; catalog number 27193). The sections were then washed with phosphate-buffered saline (PBS) and homogenized with a polytron homogenizer (B. Braun, Melsungen, Germany). Homogenized tissue samples were centrifuged for 5 minutes at 7,500 rpm at 4°C. The control samples were processed in the same manner except that no primary antibodies were added. All sections were analyzed under a light microscope (BX40, Olympus, Tokyo, Japan).
The experimental procedures were approved by the Experimental Animal Research Ethics Committee of the Ege University School of Medicine. All animals received humane care according to the criteria outlined in the "Guide for the Care and Use of Laboratory Animals (1996)" prepared by the National Academy of Sciences.
Two-way analysis of variance was performed for Pringle time and octreotide. The Bonferroni test was used to calculate the comparison of means. The histological score was evaluated with the liner-bylinear chi squared test. A value of P less than 0.05 was considered significant. The data were evaluated by using the SPSS for Windows version 13.0 (SPSS Inc., Chicago, IL, U.S.A.)
Biochemical Analysis
Octreotide-treated Groups (Table 1)
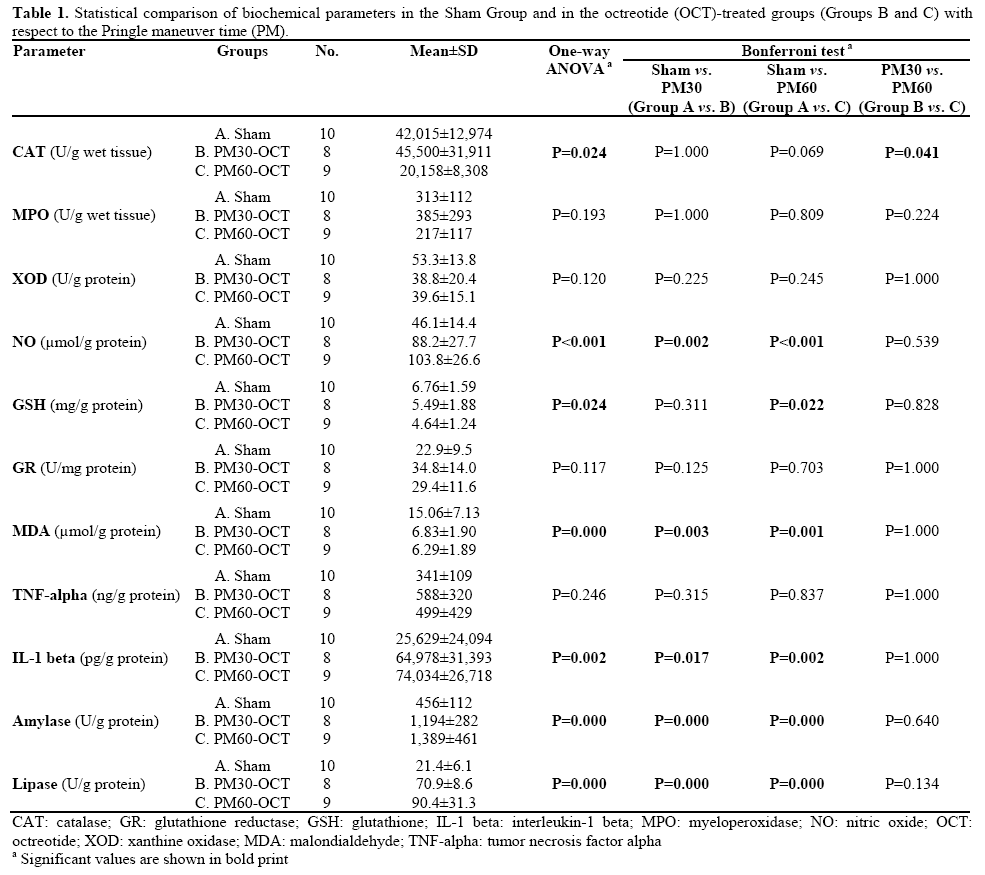
In the octreotide-treated groups, the CAT level was significantly higher (P=0.041) in Group B (PM30- OCT) as compared to Group C (PM60-OCT). MPO, XOD, GR and TNF were not found to be significantly different among the Sham Group, Group B and Group C. Amylase, lipase, NO and IL-1 beta levels were higher in Group C. MDA was found to be lower in the OCT-treated groups and it was significantly different when compared to the Sham Group. GSH was also lower in the OCT-treated groups and it was significantly different in Group C when compared to the Sham Group (P=0.022).
Saline Solution-treated Groups (Table 2)
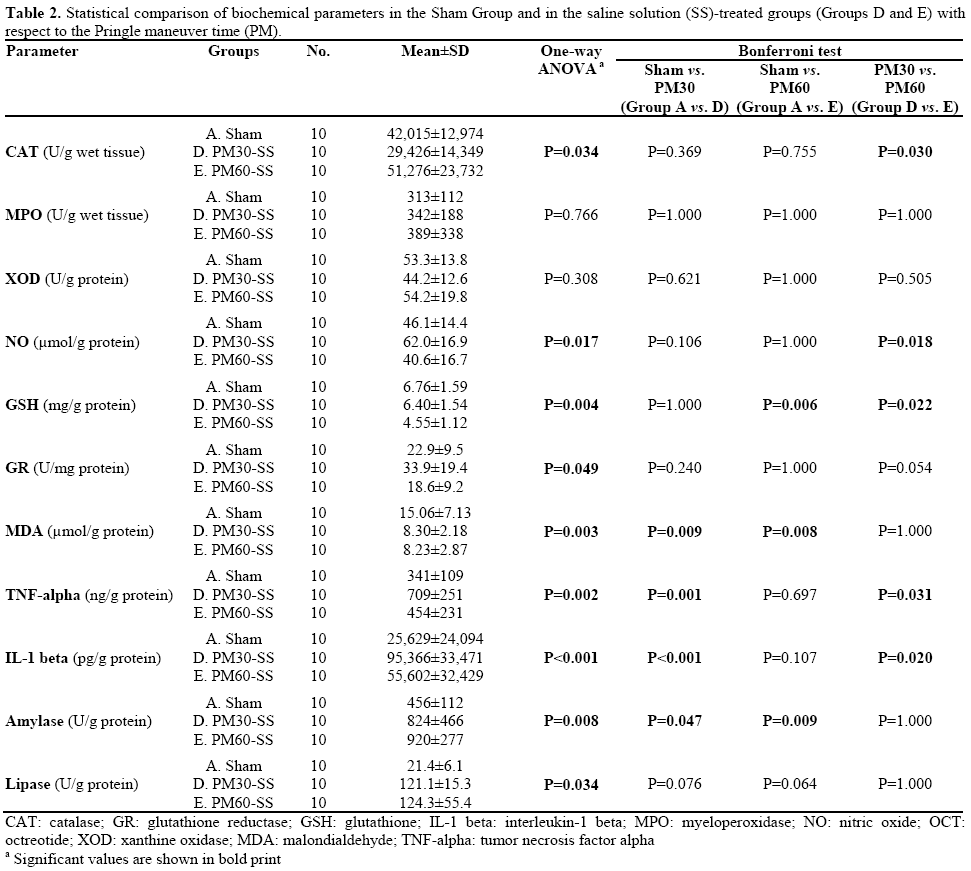
In the saline solution-treated groups, the CAT level was significantly higher (P=0.030) in Group E (PM60- SS) than in Group D (PM30-SS). No significant differences were found for MPO, XOD, GR and lipase levels. TNF-alpha and IL-1 beta were both highest in Group D and, when compared to both the Sham Group and Group E, they were found to be statistically significant. Amylase was higher and MDA level was found to be lower in Group E than in the Sham Group. When compared to the Sham Group, the results of both parameters in Groups D and E were significantly different. NO levels were found to be significantly lower (P=0.018) in Group E than in Group D. GSH was also lower in Group E and it was statistically significant when compared to both the Sham Group and Group D. Amylase and lipase values were both significantly greater in the study groups as compared to the Sham Group.
Between-study-group Analysis (Table 3)
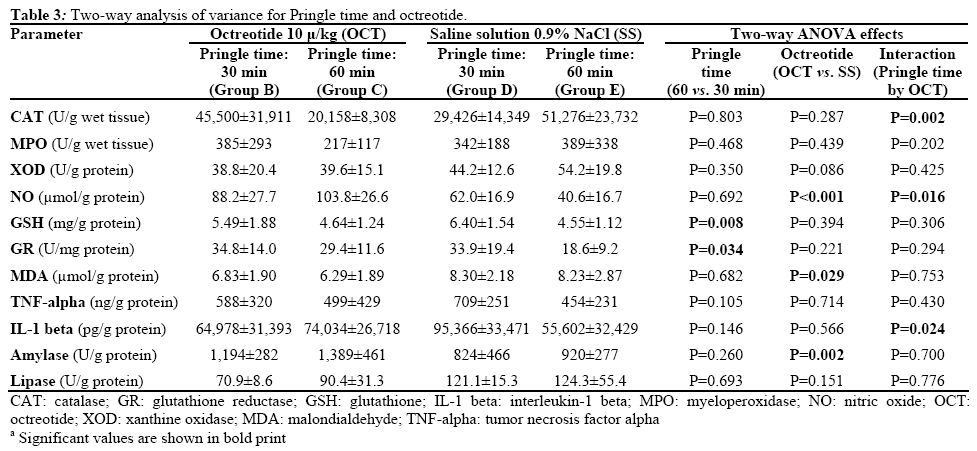
The catalase level was the highest in Group E (PM60- SS) and the lowest in Group C (PM60-SS). The significant interaction showed that the effect of increasing Pringle time was significantly different depending on octreotide treatment; i.e., it induced a reduction of catalase in OCT-treated rats while it induced an increase of catalase in saline-treated rats. MPO and XOD levels were not significantly different between the groups, although highest levels were measured in Group E. NO was significantly higher in Groups B and C (OCT groups) when compared to the Sham Group (P=0.002 and P<0.001, respectively; Table 1). Between-studygroup analysis with regards to duration showed that the rats in the OCT groups had a significantly higher level of NO than the rats which had received an isotonic solution (P<0.001); in particular, the difference in the PM60 rats was significantly higher than that of the PM30 rats (P=0.016). On the other hand, between the 30 and 60 minute portal clamping groups, when the treatment was fixed (OCT or SS), there was no statistically significant difference.
Total glutathione levels and glutathione reductase activity were not significantly different between OCTand SS-treated rats but Groups B and D (30 min portal clamping) had higher levels (P=0.034) of total glutathione (P=0.008) and glutathione reductase activity (P=0.034) as compared to Groups C and E (60 min portal clamping). In addition, total glutathione was greater in Group A as compared to Groups C (Table 1; P=0.022) and E (Table 2; P=0.006).
The amylase level was significantly higher (P=0.002) in the OCT groups (Groups B and C) than in the SS groups (Groups D and E). This was not the case for lipase levels.
Grade 0 and Grade 1 inflammation was found, for the most part, in Group A. Grade 2 injuries were higher in the octreotide-treated groups when compared to Groups D and E. But the comparison of the Sham Group with the other four groups was statistically significant. No significant differences were obtained between the octreotide- and saline-treated groups. Detailed findings are shown in Table 4.
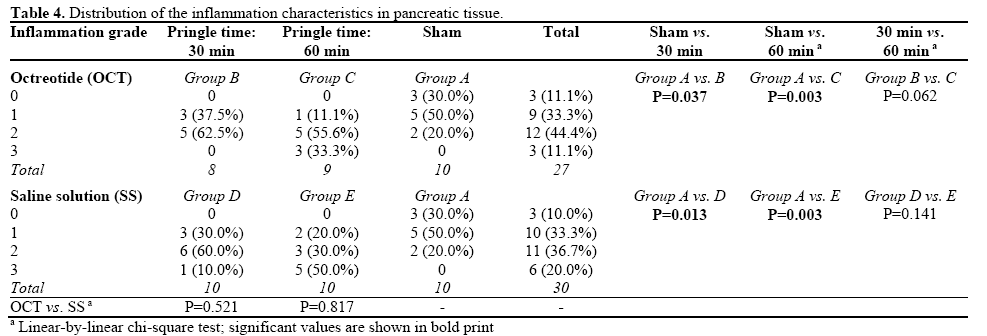
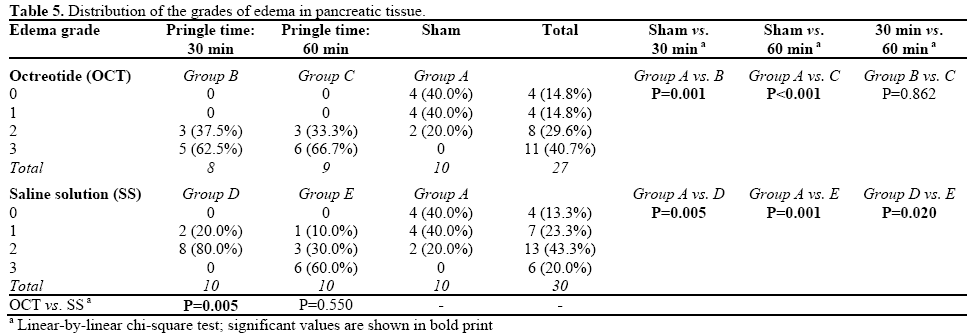
The distribution of the edematous findings in pancreatic tissue is shown in Table 5. Grade 0 and grade 1 edema formation was detected, for the most part, in Group A while grade 2 and grade 3 edema formation was detected, for the most part, in Groups B and C (OCT groups). Edema formation in all the groups was significantly different when compared to the Sham Group. Considering the Pringle time, significantly different findings were found within the SS-treated rats only (Group D vs. Group E; P=0.020). Comparison of those groups with the Pringle maneuver for 30 minutes showed that the octreotide-treated group (Group B) was found to have a higher degree of edematous change (P=0.005) than the saline-treated group (Group D). A normal rat pancreas is shown in Figure 1, and grade 3 edema and inflammation are shown in Figures 2 and 3, respectively.
TNF-alpha and IL-1 beta expression were found to be the highest in Group D (Table 3). The TNF-alpha level in Group D was significantly higher when compared to the Sham Group and Group E (P=0.001 and P=0.031, respectively; Table 2). Neither increasing occlusion time nor preoperative administration of octreotide significantly affected TNF-alpha expression (Table 3). Considering IL-1 beta expression, there was a significant difference between Group A and the other four Groups with the exception of Group E (Tables 1 and 2). The effect of the Pringle time on IL-1 beta was significantly different (P=0.024; Table 3) in OCT- and SS-treated rats; in particular, increasing the Pringle time had no significant effect in OCT-treated rats (P=1.000; Table 1) while it induced a significant reduction in SS-treated rats (P=0.020; Table 2).
An ischemic period during hepatic surgery (in particular, liver transplantation and extensive resectional procedures) is usually experienced. This can often lead to subsequent liver failure depending on ischemia-reperfusion injury. The duration of the Pringle maneuver is a decisive factor in determining whether ischemia-reperfusion injury in the liver is irreversible or not, as an ischemic period of more than 60-75 minutes causes destruction of the liver parenchyma [12, 13]. Interestingly, however, intermittent portal pedicle clamping with a total amount of 120 minutes was reported to be advantageous by Ishizaki et al. [14]. The Pringle maneuver leads not only to pathologic changes in the liver but also to pancreatic changes including venous congestion [15] and, in the case of prolonged clamping, hyperamylasemia and pancreatitis [4]. Oxygen-free radicals have been experimentally implicated as an important factor on the development and histological patterns of acute pancreatitis [16, 17]. Guice et al. showed the beneficial effects of superoxide dismutase and catalase on pancreatic injury when they were administered prior to the development of pancreatitis [16, 18, 19, 20]. According to the results in this study, catalase levels were found to be lower after a minimal rise in the octreotide-treated groups and this change was statistically significant. On the contrary, in the saline-treated groups, the catalase level was found to be significantly higher in the group in which a Pringle maneuver was performed for 60 minutes. Therefore, octreotide may cause oxidative injury in the case of prolonged portal vein clamping.
Despite advances in experimental studies on the pancreas, the mechanism involved in pancreatic changes resulting in an acute increase of portal pressure secondary to portal venous clamping has not been fully clarified. Aydede et al. pointed out that portal bed congestion can trigger an inflammatory response in the pancreas, with a directly proportional relationship between congestion and the changes [21]. Although they reported a correlation between the levels of TNF-alpha and the duration of portal clamping, in our study, elevated levels were found only in Group D when compared to the Sham Group and Group E. As a result, there was an indirect relationship between the Pringle maneuver and the TNF-alpha level.
In an experimental study by Kingsnorth, it was suggested that the IL-1 receptor antagonist decreased pancreatic and lung injury, and mortality rate [22]. In our series, in all groups, there was a statistically significant increase in IL-1 beta levels when compared to the Sham Group, with the highest value present being found in Group D. While it can be concluded that increased IL-1 beta levels following portal clamping caused a significant inflammatory reaction, there was no evidence about the effects of the clamping time or the administration of octreotide on the level of IL-1 beta
There have been several reports about hyperamylasemia secondary to portal congestion or the Pringle maneuver during hepatic resection [1, 3, 23, 24]. In our study, amylase levels were also significantly different in study groups in comparison to the Sham Group. When comparing Groups B and D (30 min clamping) with Groups C and E (60 min clamping), amylase levels were found to be higher in the groups in which octreotide was administrated (Groups B and C). However, the Pringle time was not found to have an effect on amylase levels. Thus, octreotide was determined to be a stimulant for pancreatic hyperamylasemia. In previous studies, it was emphasized that, although prophylactic octreotide administration had no beneficial effect in preventing pancreatitis-like changes following therapeutic endoscopic interventions, it was successful in decreasing serum amylase levels and severe pancreatitis [25, 26, 27]. On the other hand, published data indicate that prophylactic or therapeutic use of octreotide has no beneficial effect [28, 29, 30, 31, 32, 33]. In this study, although amylase levels were found to be elevated after the Pringle maneuver, lipase levels were not. This was associated with the late increases of lipase in serum.
Previous experimental studies have shown that NO can induce cellular injury in pancreatic tissue [24, 34]. On the other hand, glutathione has been known to be a protective agent, alleviating the severity of pancreatitis [35]. Nevertheless, glutathione levels decrease in the case of an acute pancreatic attack. But, the order in which this phenomenon appears remains a controversial topic [36, 37]. Glutathione levels were found to be significantly lower in the long-term clamping groups. This provides evidence of the positive relationship between prolonged clamping time and increased oxidative stress.
In all groups, except the Sham Group, both inflammation and edema were rather remarkable and it was considered as evidence of the harmful effects of the portal vein clamping on pancreatic tissue. On the other hand, octreotide administration caused more findings of edema; this was statistically significant with a direct proportion existing between the duration of the Pringle maneuver and inflammatory infiltration. These changes can be attributed to the harmful effects of octreotide therapy on pancreatic tissue.
In conclusion, the findings of our study have shown that the alterations in pancreatic tissue were related to portal vein clamping duration. In other words a longer duration of the Pringle maneuver yielded more severe injury to the pancreas. Moreover, octreotide administration prior to the Pringle maneuver led to an increase in pancreatic injury. Further experimental studies are needed to determine the precise mechanisms of the injury observed.
There are no conflicts of interest to declare
Many thanks to Neda Amiri for their language assistance and helpful suggestions. We also thank Hatice Uluer for the help received in the statistical analysis of the data