Key Points About What is Known:
• Homelessness is a risk factor for both acute and chronic disease; homeless populations experience an age-adjusted mortality rate 3-4 times greater than the general population.
• Poor diet and insufficient physical activity are linked with cancer and cardiovascular disease; these conditions are associated with high homelessness mortality rates.
• Improving both physical activity and vegetable and fruit consumption has substantial beneficial effects on overall health, including the prevention of cancer, cardiovascular disease, and premature death.
• No published research exists on diet/physical activity interventions in homeless adults to date.
Key Points about What is Not Known:
• There are few studies looking at behavioral health interventions in homeless adults; therefore, there are no best practices available for this population.
• Additional research is required to assess the effectiveness of technology (relative to other services shelters provide) in eliminating homelessness.
• It is critical to develop operational and process-driven improvements that would enable and empower homeless adults both to have access to and to save food.
• Future research should assess health literacy and identify the best mediums by which to transmit information and empower homeless adults to lead healthier lives.
Keywords
Nutritional surveys; Diet food and nutrition; Health behavior; Indigents; Populations; Underserved; Physical activity; Health services needs
Introduction
In the United States, approximately 2.5 million people experience homelessness annually, with over 6.2% experiencing homelessness in their lifetime [1]. Homelessness is a risk factor for both acute and chronic disease, with cancer and heart disease as leading causes of death among homeless adults ≥ 45 years of age [1-3]. Overall, homeless adults experience an age-adjusted mortality rate 3-4 times greater than the general population, with an average age of death ranging from 42 to 52 years [4,5]. Poor diet and insufficient physical activity are strongly linked with cancer and cardiovascular disease [6-8]. Studies indicate that homeless adults consume nutritionally inadequate diet and are insufficiently physically active [1,4,9-12]. Adequate physical activity and fruit and vegetable consumption are known to have substantial beneficial effects on overall health, including prevention of cardiovascular disease, diabetes, cancer, obesity, and premature death [13,14].
Despite the high prevalence of poor health behaviors among homeless adults, there have been no published studies of diet and/or physical activity interventions in this population [15,16]. Thus, the current report describes the conceptualization of a theory-based intervention, Health-e-Strides, a recently published intervention that promoted fruit and vegetable consumption and daily physical activity among sheltered homeless adults [17]. We discuss the rationale for specific intervention strategies and barriers to intervention implementation and behavior change we encountered. Finally, we present lessons learned with the hope of informing continued work with this extremely vulnerable population.
Unique challenges
Health interventions for homeless adults have historically been understudied and underfunded, prolonging profound disparities in health care outcomes [18]. Although a variety of organizations work to improve the plight of homeless individuals, they primarily focus on mental health and emergency medical care, with substantially less attention paid to health behaviors including smoking, diet, and physical activity [19]. Often, health behaviors are perceived as low priority issues, despite the fact that tobacco use, poor diet, and obesity are among the leading causes of preventable morbidity and mortality in this population [20,21]. A change in the culture of inattention to health behaviors is needed to eliminate these health disparities.
Studying this population is not without difficulties - it is intrinsically challenging to engage people experiencing homelessness due to transience and disengagement with social services. Although there has been some preliminary evaluation of dietary and physical activity interventions for sheltered homeless children, no published research has evaluated these interventions in homeless adults. A survey of 9 shelters and soup kitchens found that while only one shelter provided nutritional education, most reported that guests preferred healthier food options [22,11]. Our preliminary work indicated that homeless adults desire diet and physical activity health promotion programs [16].
What we did
We conducted a randomized pilot study, Health-e-Strides, at The Bridge in Dallas, Texas, where over 3,100 individuals experience homelessness on a given night [17,15]. The mission of the Bridge is to end long-term homelessness by delivering services for emergency shelter, health care, education, and housing. The Bridge provides shelter for over 1,200 people daily and intensive care management, income, and housing services for over 1,800 people annually. Our previously established relationship at The Bridge provided a mutual sense of familiarity with the organizational structure and needs of the population [16].
We recruited 32 transitional shelter residents to participate in Health-e-Strides. Eligible participants received either 1) a 4-week shelter-based diet and physical activity intervention, which offered tailored educational newsletters, twice daily fresh fruits and vegetables during weekdays, and pedometers with a 10,000-step daily goal, or 2) paid assessments only (intervention offered at study conclusion). Using an already validated tool, all participants were asked to complete weekly assessments of diet, physical activity, stress, readiness to change, and dietary knowledge, and all were issued accelerometers to objectively measure physical activity. Participants received $20 or $30 per weekly visit. The primary study outcomes are described elsewhere [17].
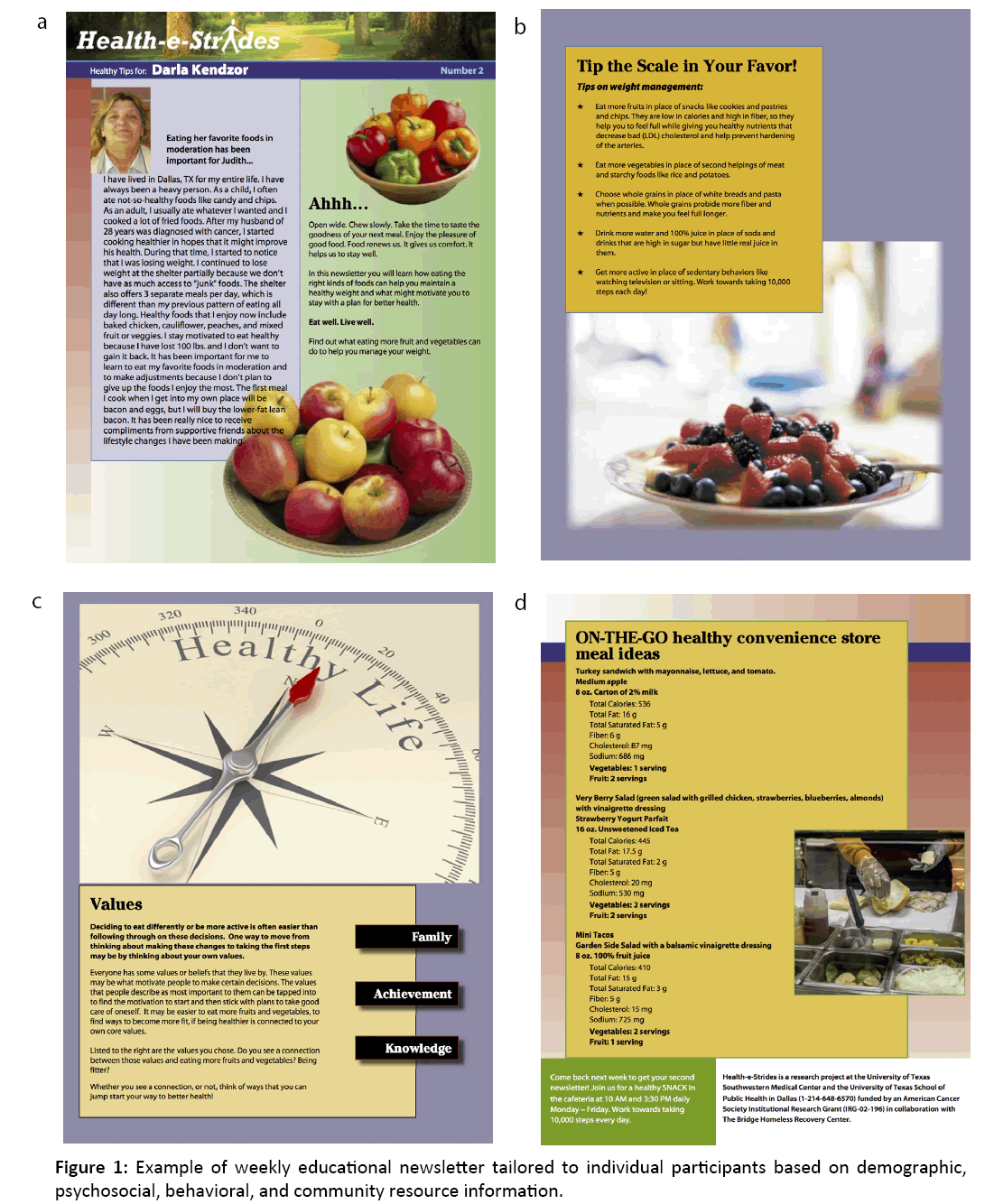
Intervention participants received a personalized, technologybased health intervention, delivered as newsletters (Figure 1a-d). Ecological models and social cognitive theory suggest interventions that emphasize both interpersonal factors (e.g., nutrition knowledge) and environmental factors (e.g., availability of nutritious foods) can impact behavior [23]. Accordingly, weekly newsletters were tailored to individual participants based on demographic, psychosocial, behavioral, and community resource information. Strategies for healthy food selection and testimonials (tailored to gender) from other shelter residents who improved their health behaviors provided relatable strategies to model positive healthy behavior. Additionally, newsletters included meal-planning examples, an advice column using a “Dear Abby” format in which an expert dietician answered questions tailored to participant-selected barriers, behavioral feedback (current behavior compared to recommendations), a stage-of-change-based action plan offering specific steps tailored to participants’ readiness to change, and information on social support for improving diet and physical activity.
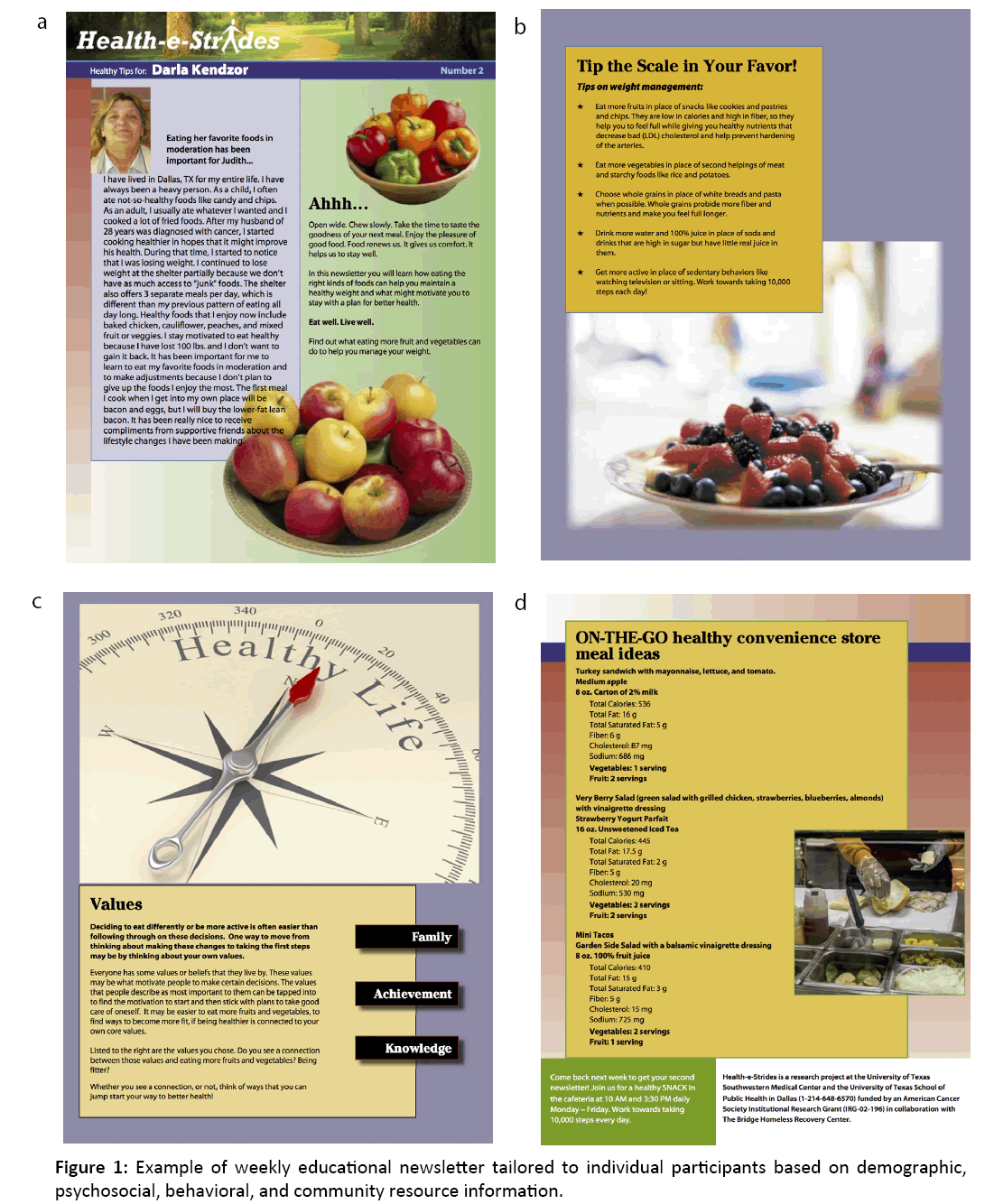
Figure 1: Example of weekly educational newsletter tailored to individual participants based on demographic, psychosocial, behavioral, and community resource information.
Main outcomes included the number of servings of fruit and vegetables consumed daily and physical activity. At study follow-up, most participants reported that the intervention was extremely/very helpful (70.6%) for increasing daily intake of fruits and vegetables and extremely/very (70.6%) helpful for increasing physical activity [17].
Throughout study development and implementation, we encountered challenges that deserve discussion, including unstable housing, lack of resources, and barriers to acquiring and storing produce. Given the paucity of homeless health interventions, we detail how these challenges were addressed.
Addressing the barriers
Unstable housing: Each night, many shelters, including the Bridge, must turn people away secondary to capacity constraints, resulting in persons being inconsistently sheltered at a variety of locations. Consequently, it can become logistically difficult to follow transient residents over time. However, different levels of stability within homeless populations exist - from living on the street to shelters or transitional housing - which can impact intervention implementation. To address this, we enrolled participants housed in The Bridge’s Transitional Shelter. Residents must return nightly by evening curfew for 4 weeks to become eligible for transitional shelter residency, where they reside in semi-private rooms while staff secure permanent housing. Many have jobs and are stable relative to individuals utilizing shelter services irregularly, allowing us to follow participants over time.
Funding, resources, and information: Lack of funding and resources further complicates implementing effective strategies for improving homeless health. The Bridge receives public funding but relies heavily on donations by private entities to fund services [24]. Though the homeless population is declining nationwide, shelters sometimes struggle to provide basic needs for their clients, including food and enough shelter space for all who arrive [25]. Pressure to provide essential services often precludes the possibility of maintaining ancillary, yet critical, health and social services. For example, while the information needs of homeless individuals range from housing and job information to health education, homeless individuals are negatively affected by limited internet access [26,27]. While other shelter services are often prioritized above technology access, technology in shelters can empower clients to take advantage of web-based health education services.
For Health-e-Strides, we provided access to 7 computers and a printer that were transported to the shelter for sessions, and the Bridge provided internet connections. Limited study funding did not cover the cost of new computers for the shelter; however, the investigators intend to seek funding for computers in future grant applications, which will serve as a resource beyond the study period.
Individualized health recommendations: Services that consider individual circumstances are viewed more favorably by homeless individuals, and self-management interventions using tailored approaches are effective for improving diet and physical activity [28-30]. Tailored newsletters, based on a previously developed and empirically supported intervention, were generated for each participant to avoid the “one-size-fitsall” approach. Newsletters were geared towards increasing selfefficacy [31]. To ensure intervention fit, the letters were further tailored to provided local resources and appropriate visuals.
Providing fresh fruit and vegetables: Shelter rules aimed at maintaining a safe environment also impacted our study. Direct provision of produce was convenient because there was no cost to participants and food preparation was not required. This was crucial given that residents did not have access to cooking facilities. However, working within the shelter’s preexisting meal schedule created a challenge for produce distribution. Because food was permitted only in the cafeteria, participants were unable to save their food, and those who could not attend scheduled distributions (who worked or were otherwise away) were unable to access the fresh produce offering. This may explain low snack time attendance (around 25% of possible snacks were dispensed). Despite this, snack times involved pleasant interaction with participants and may offer opportunities to engage and educate shelter residents in future studies.
Opportunities for intervening
Health is frequently accorded a low priority when there is housing instability. Though there appears to be high motivation and interest in adopting positive health behaviors among homeless adults, interventions are not usually available. Next, we identify unique opportunities and considerations for intervening [16].
First, access to technology can assist with job acquisition, life-skills development, and health-related services, including diet and nutrition education [26,32,33]. These immediate and substantial benefits for shelter residents argue for ways to leverage technology-based interventions for health promotion. For shelters with existing technology resources, such as internet and public computers, there is potential to initiate and sustain the dissemination of technology-based interventions.
Second, individual limitations to understanding information, including low health literacy, are important considerations in creating effective interventions. Intervention materials can be disseminated in various formats, including written and audiovisual, to address different learning styles.
Third, consider optimal timing for interactions. Our intervention worked around the established shelter schedule. Though attending scheduled snack times was not possible for some, they provided an opportunity to engage with residents. Future interventions may collaborate with shelters to provide healthy snacks in a flexible manner (e.g., distributions over a wider time period or outside of the cafeteria) to maximize resident participation.
Fourth, think creatively about how to increase access to healthy meals. A noteworthy barrier for sheltered individuals to improve their diet is the lack of personal food storage (e.g., pantry, refrigerator) or cooking area. This severely limits individuals’ ability to store their own food, significantly diminishing options in diet selection. Shelters could consider offering opportunities to cook and store purchased food to improve dietary quality as residents transition to independent living. It is important to note that 54.8% of Bridge residents receive SNAP benefits.
Shelter operations also create potential opportunities to intervene, especially as individuals must return by curfew and thus have unscheduled evening hours, during which several participants anecdotally reported inactivity and feelings of boredom. Shelter curfews provide interested audiences that may be engaged repeatedly, including those not in the transitional shelter. Therefore, there is potential for delivering educational programming (e.g. fitness or cooking classes) compatible with existing shelter schedules. On-site gym equipment could also be a valuable resource for residents.
Conclusion
There are many effective interventions aimed at improving the health of the general population. However, individuals experiencing homelessness are part of a socially and politically disenfranchised population and do not always benefit from existing services designed for broader populations. In the Healthe- Strides intervention, we focused on direct, personalized care to improve lifestyle behaviors. We adapted our methods to reach homeless adults by delivering the intervention at an established shelter and augmented health behaviors by incorporating the intervention into the shelter’s existing infrastructure.
Looking forward
Recently, the U.S. Interagency Council on Homelessness allocated a budget dedicated to social welfare programs, aiming to end chronic homelessness by 2017 [34]. Despite funding for hospital services and support for substance abuse and mental illness, modifiable risk factors such as diet and physical inactivity received no mention 2017 [35]. The development of innovative methods for reaching marginalized homeless communities is necessary to address these traditionally neglected health behaviors. This requires a shift in the culture of care and developing effective interventions for prevalent and modifiable risk factors.
Participant transience, lack of resources, and logistical obstacles should be anticipated and accommodated in planning for homeless health interventions. The desire of homeless individuals to improve health behaviors provides an excellent opportunity to intervene. Future research should explore longterm solutions that span many sectors - not limited to health organizations, shelters, and housing organizations - to provide continuity of services. These interventions require special consideration for unique barriers to healthy lifestyles, and the ethical principles of beneficence and justice demand that we challenge the status quo and afford a group that constitutes one of the most vulnerable segments of our society the opportunity to adopt health-promoting behaviors.
References
- Fazel S, Geddes JR, Kushel M (2014) The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 384:1529-1540.
- Singer J (2003) Taking it to the streets: homelessness, health, and health care in the United States. J Gen Intern Med. 18:964-965.
- Baggett TP, Singer DE, Rao SR (2013) Food insufficiency and health services utilization in a national sample of homeless adults. J Gen Intern Med. 26:627-634.
- Baggett TP, Hwang SW, O'connell JJ (2013a) Mortality among homeless adults in Boston: shifts in causes of death over a 15-year period. JAMA Intern Med. 173:189-195.
- O’connell JJ (2005) Premature mortality in homeless populations: A review of the Literature. National Health Care for the Homeless Council. Nashville, TN.
- Anand P, Kunnumakkara AB, Sundaram C (2008) Cancer is a preventable disease that requires major lifestyle changes. Pharm Res. 25:2097-116.
- Key TJ, Schatzkin A, Willett WC (2004) Diet, nutrition and the prevention of cancer. Public Health Nutr. 7:187-200.
- Reddy KS, Katan MB (2004) Diet, nutrition and the prevention of hypertension and cardiovascular diseases. Public Health Nutrition. 7:167-186.
- Sprake EF, Russell JM, Barker ME (2014) Food choice and nutrient intake amongst homeless people. J Hum Nutr Diet. 27:242-250.
- Jenkins M (2014) An assessment of homeless families' diet and nutrition. Community Pract. 87:24-27.
- Koh KA, Bharel M, Henderson DC (2016) Nutrition for homeless populations: shelters and soup kitchens as opportunities for intervention. Public Health Nutr. 19:1312-1314.
- Kendzor DE, Reitzel LR, Businelle MS (2015) Characterizing stressors and modifiable health risk factors among homeless smokers: An exploratory pilot study. Health Educ Behav. 42:642-647.
- Warburton DE, Nicol CW, Bredin SS (2006) Health benefits of physical activity: the evidence. CMAJ. 174: 801-809.
- Wang X, Ouyang Y, Liu J (2014) Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. BMJ. 349:g4490.
- Metro Dallas Homeless Alliance (2015) Point-in-Time Homeless Count and Survey Report.
- Taylor EM, Kendzor DE, Reitzel LR (2016) Health risk factors and desire to change among homeless adults. Am J Health Behav. 40:455-460.
- Kendzor DE, Allicock M, Businelle MS (2017) Evaluation of a shelter-based diet and physical activity intervention for homeless adults. J Phys Act Health. 14:88-97.
- Bogira S (2009) Starvation diet: coping with shrinking budgets in publicly funded mental health services. Health Aff (Millwood). 28:667-675.
- Baggett TP, Tobey ML, Rigotti NA (2013b) Tobacco use among homeless people--addressing the neglected addiction. N Engl J Med. 369:201-204.
- Gelberg L, Andersen RM, Leake BD (2000) The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 34:1273-1302.
- Hwang SW, Wilkins R, Tjepkema M (2009) Mortality among residents of shelters, rooming houses, and hotels in Canada: 11-year follow-up study. BMJ. 339:b4036.
- Rodriguez J, Applebaum J, Stephenson-Hunter C (2013) Cooking, healthy eating, fitness and fun (CHEFFs): qualitative evaluation of a nutrition education program for children living at urban family homeless shelters. Am J Public Health. 103: S361-S367.
- National Cancer Institute (2005) Theory at a Glance: A guide for health promotion practice (NIH Publication No. 05-3896).
- The Bridge (2016) The Bridge Homeless Recovery Center [Online]. Dallas, TX. Available: https://bridgenorthtexas.org/Services/
- Rosales C (2013) Dallas’ Bridge Homeless Shelter Juggles Basic Needs of Homeless, Transition Program. Dallas Morning News.
- Hersberger J (2002) Are the economically poor information poor? Does the digital divide affect the homeless and access to information? CJILS. 27:44-63.
- Orrick R (2011) Envisioning an internet center for homeless individuals: one group’s quest to reduce the digital divide open access connections: Homeless hub.
- De Rosa CJ, Montgomery SB, Kipke MD (1999) Service utilization among homeless and runaway youth in Los Angeles, California: rates and reasons. J Adolesc Health. 24:190-200.
- Lorig KR, Hurwicz ML, Sobel D (2005) A national dissemination of an evidence-based self-management program: a process evaluation study. Patient Educ Couns. 59:69-79.
- Wagner EH (1998) Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1:2-4.
- Campbell MK, Carr C, Devellis B (2009) A randomized trial of tailoring and motivational interviewing to promote fruit and vegetable consumption for cancer prevention and control. Ann Behav Med. 38:71-85.
- Mcinnes DK, Sawh L, Petrakis BA (2014) The potential for health-related uses of mobile phones and internet with homeless veterans: results from a multisite survey. Telemed J E Health. 20:801-809.
- Miller KS, Bunch-Harrison S, Brumbaugh B (2005) The meaning of computers to a group of men who are homeless. Am J Occup Ther. 59:191-197.
- United States Interagency Council on Homelessness (2010) Opening doors: Federal strategic plan to prevent and end homelessness.
- United States Interagency Council on Homelessness (2015) The President’s 2016 Budget: Fact sheet on homelessness assistance.