- (2010) Volume 11, Issue 5
Amanjeet Singh, Tanveer Singh, Adarsh Chaudhary
Department of Surgical Gastroenterology, Sir Ganga Ram Hospital, Rajinder Nagar. New Delhi, India
Received May 7th, 2010 - Accepted June 18th, 2010
Context There is limited information available about the feasibility and benefits of synchronous resection of liver metastases in patients with pancreatic and periampullary cancer undergoing pancreaticoduodenectomy. Objective We report on our experience with 7 such patients. Design Analysis of the prospective database was carried out to identify patients who underwent synchronous resection of liver metastases with pancreaticoduodenectomy. Patients Two-hundred and thirty patients underwent pancreaticoduodenectomy for pancreatic and periampullary cancer in our unit between September 2003 and September 2009. Main outcome measures The primary aim of our study was to determine the survival benefits and the secondary aim was to evaluate their safety and influence on the results of a pancreaticoduodenectomy. Results Seven patients (3%) underwent synchronous resection of a solitary liver metastasis. In these patients, the operative time and intra-operative blood loss was marginally high as compared to the overall cohort of patients undergoing pancreaticoduodenectomy; however, the complication rates and the duration of the hospital stay were not affected. In patients undergoing resection of liver metastasis, there were 4 recurrences over a mean follow-up of 21 months. Conclusions In patients with resectable pancreatic and periampullary cancer, the resection of a solitary liver metastasis can safely be performed together with a pancreaticoduodenectomy; however, its impact on improving survival has yet to be proven.
Adenocarcinoma; Hepatectomy; Neoplasm Metastasis; Pancreatic Neoplasms; Pancreaticoduodenectomy
ISGPF: International Study Group on Pancreatic Fistula
Surgery is the treatment of choice for pancreatic and periampullary cancer. With improvements in surgical techniques and better perioperative management, the morbidity and mortality of a pancreaticoduodenectomy has decreased. With these encouraging developments, the limits of pancreaticoduodenectomy are being stretched. Data about multivisceral resections together with a pancreaticoduodenectomy are being published. Though the benefits of such major procedures have yet to be conclusively proven, it is evident that they can safely be performed in experienced centers [1, 2].
In patients being considered for pancreaticoduodenectomy, despite all relevant preoperative investigations, at laparotomy, it is not unusual to find unexpected peritoneal or liver metastases. Confronted with a solitary liver metastasis in an otherwise resectable tumor, it is difficult to decide on the appropriate management. A choice has to be made between abandoning the plan for radical surgery and resorting to a palliative bypass, performing a pancreaticoduodenectomy and leaving the liver metastasis to be treated by adjuvant chemotherapy or considering synchronous resection of the liver lesion together with a pancreaticoduodenectomy. Information in the available literature is inadequate to decide upon the best option. It has now been well established that a subgroup of patients with liver metastases from colorectal cancers benefit from surgical resection. These results induced a paradigm shift in the management of liver metastases. Traditionally, liver resection for colorectal liver metastases has been performed as a separate procedure from colectomy or rectal excision. But, recently, there have been reports of a concomitant resection of liver metastasis with colonic resection with good results [3, 4, 5, 6]. Experience with surgery for liver metastases from pancreatic or periampullary cancer is limited and, as expected, experience with synchronous resection together with a pancreaticoduodenectomy is limited to a few patients only [7, 8, 9]. We report on our experience of synchronous resection of liver metastases together with pancreaticoduodenectomy.
Analysis of our prospective database of patients undergoing pancreaticoduodenectomy for pancreatic and periampullary cancer between September 2003 and September 2009 was carried out in order to identify patients who underwent synchronous resection of an isolated liver metastasis. Two-hundred and thirty patients were identified. These included 170 (73.9%) males and 60 (26.1%) females with a mean age of 53.6±11.8 years (range: 18-80 years).
Preoperative staging in our protocol included a contrast-enhanced computed tomographic scan. Diagnostic laparoscopy was not a part of our staging procedure. All patients being considered for synchronous liver resection were evaluated with intraoperative ultrasound to rule out any other liver metastases which could have been missed on palpation. Synchronous liver resection was performed only if a R0 resection of the pancreatic or periampullary tumor was possible. We aimed at achieving at least a one centimeter circumferential margin while attempting resection of the liver metastases. Resection of the primary tumor was performed first and only then resection of the liver metastasis attempted. This was done to avoid an unnecessary liver resection if a complete resection of the primary tumor was not possible. The reconstruction was performed as a final step so that, if a Pringle maneuver was required to control bleeding during the liver resection, it would not affect the integrity of the various anastomoses due to venous congestion.
All postoperative complications were recorded. Standard definitions as proposed by the International Study Group on Pancreatic Fistula (ISGPF) were used for evaluating complications [10]. Patients operated on after May 2005 were prospectively analyzed using ISGPF criteria while patients undergoing surgery before this period were retrospectively analyzed as per these criteria. The length of the hospital stay was considered to be from the first postoperative day until discharge from the hospital. Death during the same hospital stay or within 30 days of surgery was considered as operative mortality.
The primary aim of our study was to determine the survival benefits of such procedures and the secondary aim was to evaluate their safety and influence on the results of pancreaticoduodenectomy.
Since it was a retrospective analysis of data, consent was not obtained as per our institutional research committee policy. The patients were managed according to the ethical guidelines of the "World Medical Association Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects" adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964, as revised in Tokyo 2004.
Data are reported as means, standard deviations and frequencies. The median follow-up time was also evaluated. The Fisher’s exact and the Student’s t tests were applied when appropriate by using the SPSS statistical package (version 13.0 for Windows; SPPS Inc., Chicago, IL, USA). Two-tailed P values less than 0.05 were considered statistically significant.
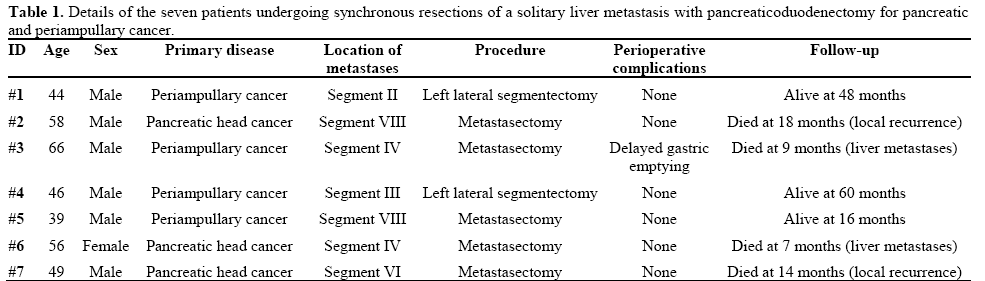
Eleven (4.8%) out of 230 patients undergoing pancreaticoduodenectomy for pancreatic and periampullary cancer were detected to have isolated liver metastases. Seven of these were diagnosed preoperatively on CT scan while four were diagnosed intraoperatively. Synchronous resection was not considered in four patients: two with locally advanced tumors (both had a diagnosis of liver metastases on preoperative CT) and another two with multiple liver metastases seen on intraoperative ultrasound (both had intraoperative detection of liver metastases). Seven patients (3.0%) underwent synchronous resection of the isolated liver metastasis together with a pancreaticoduodenectomy. Four of these patients had periampullary cancer while three underwent pancreaticoduodenectomy for pancreatic cancer. Liver metastasis was located in the left lobe in three patients while it was in the right lobe in four patients. Resections were in the form of left lateral segmentectomies in two patients and metastasectomy in five patients (Table 1). All seven patients underwent a classic Whipple procedure with a single loop reconstruction and a duct to mucosa pancreaticojejunostomy.
The histopathological examination of the resected specimens revealed adenocarcinoma in all patients with negative resection margins for both the primary and metastatic lesions. One patient had delayed gastric emptying which was resolved with conservative management. There was no operative mortality in these 7 patients. Though the operative time (420±41 min vs. 362±36 min; P<0.001) was significantly longer and the intraoperative blood loss (372±75 mL vs. 320±84 mL; P=0.107) was only marginally elevated as compared to the other 223 patients undergoing pancreaticoduodenectomy, the overall complication rate (3/7, 42.9% vs. 73/223, 32.7%; P=0.687) and the duration of the hospital stay (9.7±4.8 days vs. 9.4±5.1 days; P=0.878) were comparable. None of the seven patients undergoing synchronous resection required perioperative blood transfusion versus 21 (9.4%) of the other 223 patients (P=1.000). All patients who had synchronous liver resections received chemotherapy versus 134 (60.1%) of the other 223 patients undergoing pancreaticoduodenectomy (P=0.576).
Over a mean follow-up of 24.6±20.8 months (median: 16 months; range: 7-60 months), there were four recurrences in patients undergoing synchronous resection of a liver metastasis (57.1%); two of them were in the liver and two had a locoregional recurrence. Three patients are disease free at follow-up times of 16, 48 and 60 months (Table 1).
The presence of liver metastases in abdominal malignancies has been regarded to be a sign of disseminated disease with a poor outcome. In recent years, this pessimistic view has undergone some change with evidence of good results of surgical resection in selected patients with colorectal liver metastases. Interest in the surgical treatment of liver metastasis started with the premise that the liver forms the first filter for the colorectal region; therefore, patients with colorectal cancer with metastasis confined to the liver may not have disseminated disease in contrast to patients with hematogenous metastases. Good results of surgical treatment for colorectal liver metastases led to surgery also being recommended for liver metastases from non-colorectal primary tumors. Meaningful prolongation of survival has also been achieved in these patients also [11, 12]. Pancreatic and periampullary cancer, such as colorectal cancer, also drain into the portal system, and the liver is one of the most common organs to be affected by these tumors. Surgical resection of liver metastases from these tumors has not generally been acceptable. This is because, biologically, pancreatic and periampullary tumors are inherently aggressive with poor long-term survival especially in patients with pancreatic cancer. Moreover, the required surgical procedure for these tumors, i.e. pancreaticoduodenectomy, itself carries significant morbidity and possible mortality. Combining another procedure, such as a liver resection, with pancreaticoduodenectomy makes it a formidable proposition. These are the possible factors for withholding the use of resectional surgery in hepatic metastasis from pancreatic and periampullary tumors. In colorectal cancer, the availability of newer chemotherapies has also contributed to improving both the resectability and the survival rates. Chemotherapy has yet to show similar promise in pancreatic cancer.
As already mentioned, with a definite decrease in mortality and a reduction in morbidity associated with pancreaticoduodenectomies, data are emerging regarding the potential benefits of multivisceral resections in locally advanced pancreatic cancer. In a recent study, 19 patients underwent additional organ resections together with a pancreaticoduodenectomy in the form of a right hemicolectomy in 12, right nephrectomy in 2, liver resections in 2 and a combination of colon, kidney, adrenal and small bowel resection in 3 patients. There was no significant difference in the complication rates, and the authors concluded that additional organ resections can be performed without any significant added morbidity [2]. Multivisceral resections for pancreatic malignancies have been shown to be safe and have survival rates comparable to standard resections [13]. There have been reports of long-term survivors of pancreatic cancer (more than 5 years) undergoing pancreatectomies, and a multicentre study has concluded that long-term survival after pancreatic cancer is a reality after R0 resections, even with advanced disease [14]. There is still a paucity of evidence regarding the benefits of surgery in patients with metastatic liver disease associated with pancreatic and periampullary cancer. In a study involving 16 patients with synchronous and 7 patients with metachronous resections of a solitary liver metastasis of pancreatic and periampullary cancer, Klempnauer et al. [15] showed a median survival time of 8.3 months after synchronous and 5.8 months after metachronous hepatic resections with one-year survival rates of 41% and 40%, respectively. The authors concluded that, although distant metastases are a definite sign of advanced tumor stage, the prognosis of patients with hepatic metastases should not be uniformly considered hopeless. Shrikhande et al. [9] have also published their experience with synchronous resection of liver metastases in pancreatic cancer in 11 patients. They reported a median survival of 11.4 months in the synchronous resection group as compared to 5.9 months in patients undergoing exploratory laparotomy with or without a palliative bypass. The morbidity and mortality of synchronous liver resection with pancreaticoduodenectomy was comparable to patients undergoing pancreaticoduodenectomy alone. In a systematic review of patients undergoing synchronous resections of liver metastases together with pancreaticoduodenectomy, 103 patients were included from three case reports and 18 studies involving fewer than 10 patients; it appeared that liver metastasis resection for locally resectable pancreatic cancer can be performed in selected cases with low morbidity and mortality. Overall survival in cases with only one or a few liver metastases resected concomitantly with a pancreaticoduodenectomy seemed to be comparable to cases undergoing pancreaticoduodenectomy without evidence of metastasis [16]. On the contrary, Gleisner et al. [17] have questioned the benefits of synchronous liver resections together with pancreaticoduodenectomy in patients presenting with isolated liver metastases detected intra-operatively in pancreatic and periampullary cancer. In their experience with 22 patients, out of which 15 had periampullary or pancreatic head cancer, they demonstrated that aggressive surgical resection combining resection of the primary lesion with liver resection for these patients yielded an overall survival rate similar to a palliative bypass alone, yet with increased morbidity, hospital stay and, perhaps, mortality. They preferred performing a palliative bypass on these patients as it appeared to be associated with less morbidity and might have expedited postoperative recovery and institution of systemic chemotherapy. There was no difference in survival between pancreatic (median 5.9 months) and non-pancreatic (median 9.9 months) primary tumor histology in patients who underwent synchronous resection for liver metastases (p=0.43). We performed resection of the liver metastasis together with a pancreaticoduodenectomy with the expectation that a possible R0 resection might benefit patients with resectable tumors. Confirmation that the metastasis in the liver was isolated was made intraoperatively by using intraoperative ultrasound. It was our belief that merely carrying out a palliative bypass would be unfairly depriving the patient of possible prolongation of survival and we were reluctant to rely on chemotherapy alone to manage the liver metastasis, mainly because, in the event of a complication developing after pancreaticoduodenectomy, chemotherapy would be delayed or not used at all. The three patients in our series who have survived had surgery performed for periampullary tumors; all 3 patients with pancreatic cancer died. It could be that, since periampullary cancer has also traditionally been shown to have a better prognosis as compared to pancreatic head cancer, this could indicate that periampullary cancer might be a better candidate for synchronous resection of liver metastases. On follow-up, only two of our patients had recurrence of disease in the liver while, in the remaining five patients, the liver was free of disease until death or until the last follow-up. Though the numbers in our study are too small to have any definitive correlation, it appears that, in centers with liver and pancreatic surgery experience, minor liver resections can be safely performed together with a pancreaticoduodenectomy without adding any additional morbidity or mortality. Though the operative time may be prolonged and the complexity of the surgery increased, the overall complication rates remain unaffected. The addition of a metastasectomy or left lateral segmentectomy does not increase blood loss enough to necessitate the need for blood transfusion. Though weak, there is some evidence to suggest a poorer long-term outcome in patients with pancreatic cancer who receive an intraoperative blood transfusion [18]. We hope our experience contributes to developing heightened awareness regarding the possible potential of aggressive surgery in this complex clinical situation and stimulates the start of a larger multicenter study
The authors have no potential conflict of interest