Case Report - (2017) Volume 3, Issue 4
RA Hvastunov1, VV Ermilov1, Agarwal A2*, Mouhammed HA3 and YC Yang1
1Volgograd State Medical University, Volgograd, Russia
2Department of Pathology, Faculty of Medicine, Northern Borders University, Kingdom of Saudi Arabia
3Department of Pathology, Faculty of Medicine, Suez Canal University, Ismailia, Egypt
*Corresponding Author:
Agarwal A
Department of Pathology, Faculty of Medicine
Northern Borders University, Kingdom of Saudi Arabia.
Tel: 009663836537
E-mail: dranshoo3@gmail.com
Received date: November 13, 2017; Accepted date: November 20, 2017; Published date: November 25, 2017
Citation: Hvastunov RA, Ermilov VV, Agarwal A, Mouhammed HA, Yang YC (2017) Stomach (Gastrointestinal Stromal Tumor) GIST in a Patient of Situs Inversus Totalis: A Rare Association and Brief Case Report. J Clin Epigenet. 3:42. doi: 10.21767/2472-1158.100076
Situs inversus is a rare congenital condition in which the major visceral organs are reversed from their normal positions. Usually, it involves complete transposition (right to left reversal) of all of the abdominal organs and only a small percentage is associated with GIST which is the rare mesenchymal tumors of the alimentary tract. Nowadays GISTs represents 0.1% to 3% of all gastrointestinal malignancies, making it a diagnostic challenge. Lesions are frequently located in stomach and proximal small intestine but rarely elsewhere in the abdomen. They are believed to result from mutations of proto-oncogenes c-Kit or platelet-derived growth factor receptor alpha polypeptide, this increase tyrosine kinase receptor activity, leading to uncontrolled proliferation of stem cells that differentiate into cells of Cajal. They can occur at any age but predominantly in middle-aged people and in elderly. We report a very rare case of stomach GIST in Situs inversus totalis. A 56-yearold male presented to our hospital complaining of pain in the epigastrium with melena, findings suggested a gastric GIST. Cytologic and immunohistochemistry analysis confirm diagnosis of GISTs. The reverse location of the internal organs caused no significant difficulties for surgical treatment.
Keywords
GIST stomach; Full inversion of internal organs; Situs inversus totalis; Gastrointestinal stromal tumor
Background
The term “gastrointestinal stromal tumors” was first suggested in 1983 for the description of gastrointestinal non-epithelial tumors and they differ in immunohistochemical and ultrastructural characteristics from tumors with true neurogenic and smooth muscle differentiation.
Stromal or mesenchymal tumors that affect the gastrointestinal tract typically appear as subepithelial neoplasms. The most common is Gastrointestinal Stromal Tumors Group (GIST), which arise from mesenchymal stem cells programmed to differentiate into interstitial cells of Cajal in the myenteric plexus [1]. The cells of Cajal form a complex cell network within the gastrointestinal tract wall where they function as a pacemaker system. The GIST can arise from anywhere into the gastrointestinal tract and are frequently located in stomach (66%) and small intestine (30%) particularly in duodenum, as well as in esophagus, colon, anus and rectum (<10%) They can even occur out of the digestive tube, by example in omentum, mesentery or peritoneum [2].
GIST are characterized by exhibit proto-oncogene proteins c-Kit mutations (CD117 and/or CD34) and also platelet-derived growth factor (PDGF-alpha). CD117 detected by immunohistochemistry confirms the diagnosis of GIST [3]. The tumor size by itself, does not predict the GIST biological behavior. However, the mitotic index, the size and location of tumor are used together with the end to predict the biological behavior and the risk of disease progression [2]. The term situs inversus is the short term of the Latin phrase “situs inversus viscerum” which means “inverted position of internal organs”. Dextrocardia, a condition when the top of a heart is directed to the right, was first noticed and described by Leonardo da Vinchi in 1452-1519 and then by Marco Severino in 1643. However, the condition of situs inversus was first described more than a century later by Matthew Baillie.
Situs inversus totalis affects all the main organs of rib cage and abdomen. The organs re-located have mirror reflection. The heart is located in the right side of rib cage, a stomach and spleen are in the right side of abdomen, liver and gallbladder are on the left. The left lung is three-lobed; the right lung is two-lobed. Blood vessels, nerves, lymphatic vessels and intestines are also inverted. When heart is located on the right side of rib cage, this condition is called the transposition of internal organs with dextrocardia and situs inversus totalis. In case of absence of any congenital heart defects, people with the transposition of internal organs can lead a normal life without any complications. Among people with situs inversus totalis there are 5-10% of cases with heart defects, specially expressed in the form of wrong position of cardiac vessels [4,5].
Our case report of association of stomach GIST in the patient with transposition of internal organs in a same patient is very rare and of clinical interest.
Our case report of association of stomach GIST in the patient with transposition of internal organs in a same patient is very rare and of clinical interest.
Case Report
The patient G, born in 1956 (56 years), was on treatment in Thoracoabdominal Department of the clinic No 1 for the period from 20.10.2009 to the 13.11.2009. He presented with the complaints of weakness and moderate pain in the epigastrium with melena for the past one month [6-9].
On fibrogastroduodenoscopy done on 20.10.2009: the esophagus was patent and gastroduodenoscopy was possible but in gastric cardia there was obstruction and lumen was found to be narrow. The stomach lumen mucosa was smooth and the body of the stomach closer to the greater curvature showed presence spherical submucosal tumor 6 cm × 5 cm with ulceration on its surface of a size of 0.8 cm. Pylorus was patent. The duodenum bulb and post bulbar part of the duodenum had no significant findings.
On X-ray of the chest and stomach done on 10.12.2009: dextrocardia was found. The esophagus was patent. Gastric cardiac wall had elasticity. The body of the stomach had a dumbbell tumor of a size of 9 × 14 cm with smooth contours, antral part of the gastric antrum had no significant. The stomach was located on the right side. And the conclusion based on the findings made was of non-epithelial tumor of the stomach.
According to the ultrasound of abdominal organs and retroperitoneal lymph nodes done on 20.10.2009; there was identified situs inversus totalis. There were no significant local changes. In the stomach on the right side was a tumor mixed type, predominantly solid of a size of 8.2 × 5.5 × 8.0 cm.
ECG showed sinus rhythm, pulse rate was 70 per min. There was Dextrocardia and there were frequent ventricular premature beats [10].
Echo done on 28.10.2009 showed malposition of the heart i.e. there was Dextrocardia. The heart was properly formed. The heart cavity was not expanded. The valves were not changed.
A detailed physical examination showed there was no significant finding. Peripheral lymph nodes were not enlarged. Patient’s post-hemorrhagic anemia had preoperative correction in the form of hemostimulating therapy and transfusion of the erythrocyte mass. Clinical diagnosis made was of Leiomyosarcoma of the stomach body.
The patient underwent laparotomy. Patient diagnosis of situs inversus totalis was confirmed. The stomach was located in the right upper quadrant. A tumor in the stomach with a size of 12 × 8 × 7 cm was found, originating from the anterior wall of the middle third of the body with a marked exophytic component (Figure 1). There were no distant metastases. Subtotal distal stomach resection by Billroth II was performed because of the non-epithelial nature of the tumor (Figure 2). During surgery 4/5 of the stomach was removed. The tumor was found to invade all layers in the body of the stomach and was the size of 12 × 8 × 7 cm with ulceration (Figure 3).
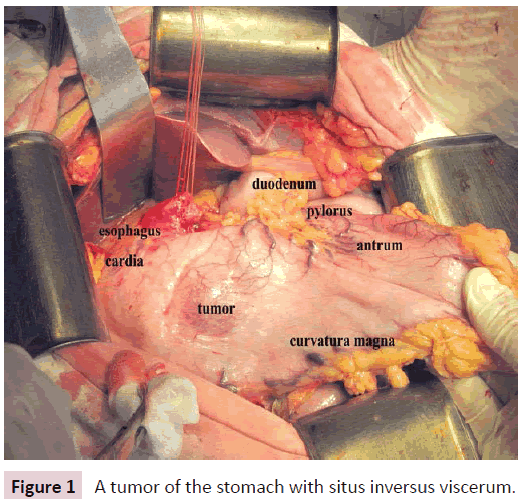
Figure 1: A tumor of the stomach with situs inversus viscerum.
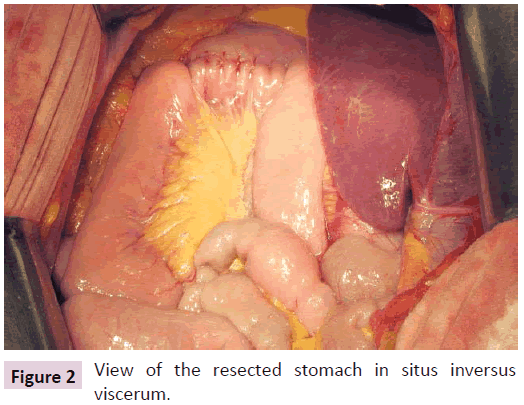
Figure 2: View of the resected stomach in situs inversus viscerum.
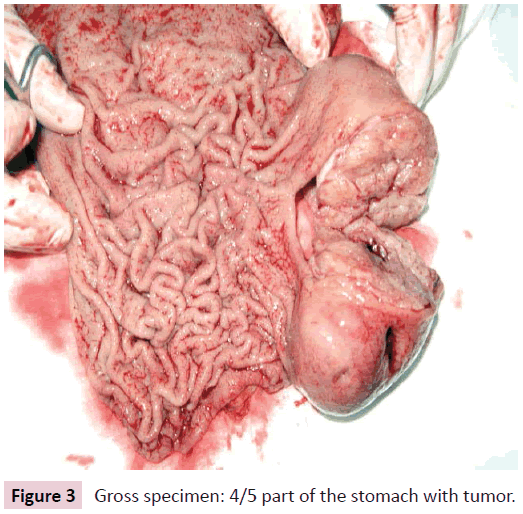
Figure 3: Gross specimen: 4/5 part of the stomach with tumor.
Histopathological examination showed that the border of resected stomach and duodenum was without tumor growth, the tumor was diagnosed as to be leiomyosarcoma with perigastritis lymphadenitis.
Immunohistochemical study of the tumor was done microscopy showed as tumor to be a combination of fusiform and histiocytomas cells expressing S-100, Vimentin, NSE, CD117, CD34, smooth muscle’s actin in some cells (Figures 4-9). The marker of proliferative activity Ki-67 was less than 10%. Findings were conclusive of morpho-immunohistochemical pattern corresponding with GIST tumors of low degree of malignancy.
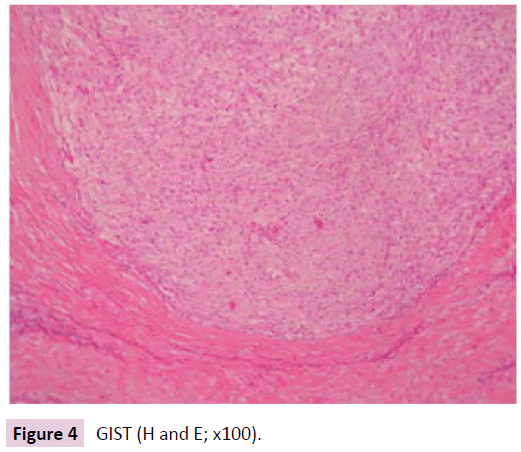
Figure 4: GIST (H and E; x100).
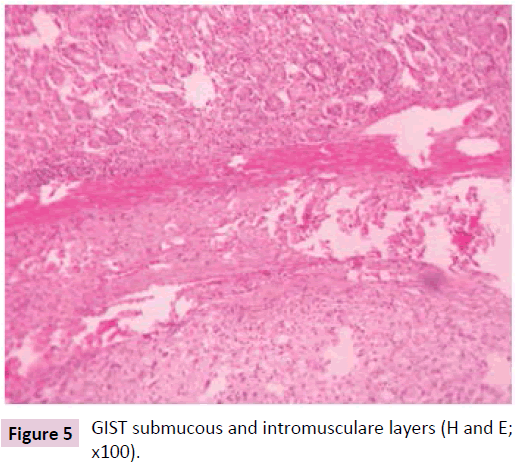
Figure 5: GIST submucous and intromusculare layers (H and E; x100).
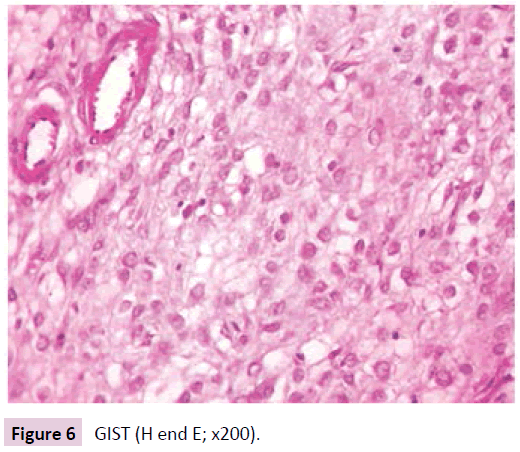
Figure 6: GIST (H end E; x200).
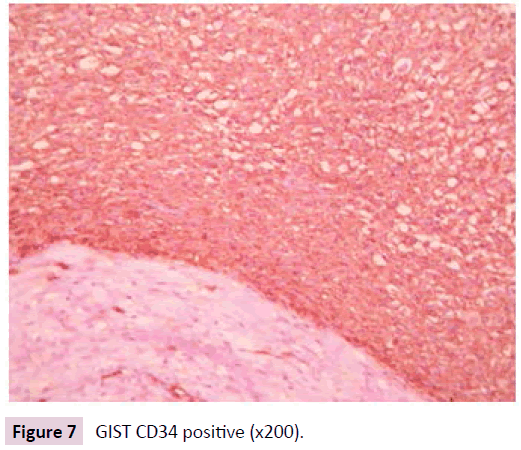
Figure 7: GIST CD34 positive (x200).
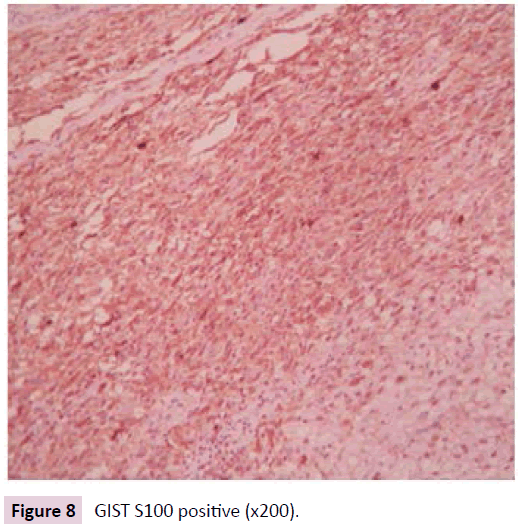
Figure 8: GIST S100 positive (x200).
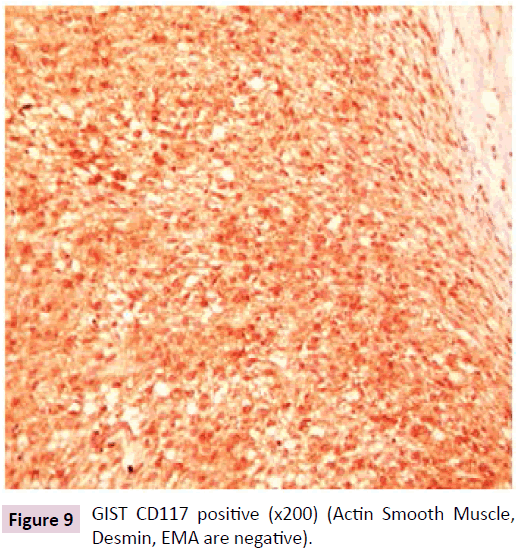
Figure 9: GIST CD117 positive (x200) (Actin Smooth Muscle, Desmin, EMA are negative).
As it was a local form of GIST of the stomach without nodal metastases and hematogenous metastases to the liver, radical surgery was done and there were no complications after surgery. The patient was discharged on the postoperative 13th day.
The final clinical diagnosis was GIST of the stomach. Follow up after subtotal distal gastric resection by Billroth II, was done in in 2012 (28 months after operation), x-ray of the stomach stump, CT of the chest and abdomen (Figures 5-11) and other data supported no relapse or progression.
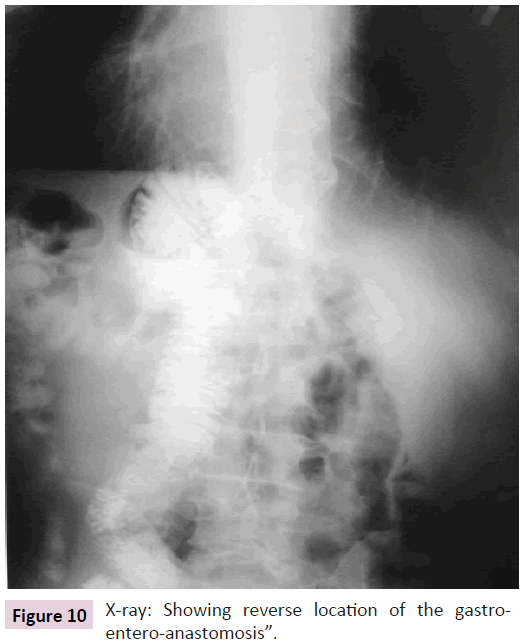
Figure 10: X-ray: Showing reverse location of the gastroentero- anastomosis”.
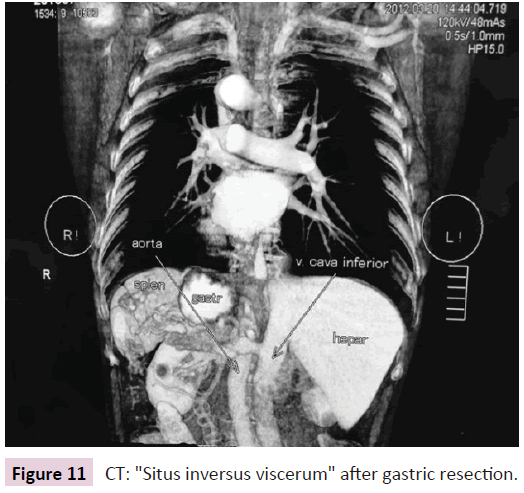
Figure 11: CT: "Situs inversus viscerum" after gastric resection.
Thereby, due to the low potential of malignancy of the tumor and as the radical surgical treatment was done it was possible to ensure a sufficiently long period of survival without progression and relapse. The reverse location of the internal organs caused no significant difficulties for surgical treatments.
Discussion
Gastrointestinal stromal tumors are mesenchymal tumors of stomach. The GIST morbidity is to 10-20 cases in 1 million of population per year. The malignant GIST are 20%-50% of all cases and the 5-year-survival of these cases are approximately 70%-80%. The general phenotype (expression CD117) and morphological resemblance with interstitial cells of Cajal shows that GIST develops from these cells of their predecessors. Interstitial cells of Cajal form a net in a muscular wall of gastrointestinal tract and regulate its autonomic peristaltic activity, in other words they appear to be pacemaker cells providing the connection between smooth muscle cells and nerve endings. The presence or absence of the activated c-KIT receptor particularly defines the following differentiation of primitive mesenchymal cells-predecessors, which may go in the direction of either interstitial cells of Cajal or smooth muscle respectively. In present time the mesenchymal tumors of gastrointestinal tract which are positive for CD117 are referred to as GIST and the results of immunohistochemical analysis showing the presence of expression CD117 are significant in defining and helpful in differential diagnostics. The other markers, which help to immunophenotype and differentiate GIST from other tumors of gastrointestinal tract with mesenchymal origin, are CD34-antigen, S-100 protein, smooth muscle actin (SMA) and desmin. Thereby immunohistochemical markers contribute significantly and are an essential part of the diagnostic process and hence immunohistochemistry must be done in all the cases of mesenchymal neoplasms of gastrointestinal tract and those located in retroperitoneal space for confirmation and making the final diagnosis. c-KIT is not only expressed by GIST cells and interstitial cells of Cajal, but also by the normal cells (mast cells, melanocytes, Leydig cells, spermatogonia, hematopoietic stem cells) and play important role in melanogenesis, spermatogenesis and hemopoiesis. Furthermore, the expression of given receptor is seen in small cell lung cancer, seminoma, Ewing\s sarcoma, angiosarcoma, melanoma, acute myelogenous leukemia, ovarian cancer, neuroblastoma. However, these tumors are rarely considered in the differential diagnosis of GIST, because they have their own remarkable morphological features and they do not cause any significant difficulties to the pathologists in diagnosing them. Depending on the predominance of one or another component on morphology they have been categorized into spindle cell (70%), epithelioid (20%-25%) and mixed variants of GIST. The majority of tumors at the time of diagnosis and in the absence of dissemination and infiltration of organs/tissues look like benign neoplasms (up to 70%). However, pathologist prefer not to use the term “benign” because it is considered that almost all the GIST have malignant potential and possibly with the prolonged observance the benign tumor also may change into malignant neoplasm. For this reason, another criterion, like mitotic activity and size of the neoplasm indicates the risk of the aggressiveness of the tumor and is more important [2,4].
A typical localization for GIST is a stomach (60%-70%), small intestine (25%-35%), colon and rectum (5%). In rare cases a tumor may appear in esophagus, mesentery, gland, retroperitoneal space (10%). As soon as a primary tumor localizes in submucosal layer, there are certain difficulties in histological confirmation of diagnosis during the preoperative phase. The histological diagnosis is established through endoscopic methods only in 50% of cases. Small neoplasms most frequently do not present with any clinical symptoms and detected accidentally during endoscopic studies or laparotomy.
GIST is not many times diagnosed during emergency surgeries, associated with organ perforation or bleeding. By the time diagnosed 15%-50% of patients already have metastases but the extent of the disease as a rule is limited to the abdomen. At the same time metastases into liver is seen in 60% of cases, dissemination along the peritoneum is observed in 21% of cases. Regional lymph node, bones and lungs are hardly ever affected. The surgical methods remain the main form of treatment in absence of any signs of dissemination of the malignancy. However, its effectiveness is limited and depends on the level of local prevalence of the disease and radicality of operation. In case of local involvement, the frequency of relapses after the radical operation approximates to 35%, in locally invasive disease (when nearby organs and tissues are involved) it reaches 90% and In case of relapse, the tumor process is basically localized intra abdominally. On average, the 5-year-survival after the surgical treatment varies from 35% to 65%. The prognosis for the diseased depends on the mitotic tumor activity, the sizes of the primary neoplasm and its localization.
Conclusion
Recent studies also detect correlation between the extent of c-KIT mutation and relapse-free survival of patients. Chemo and radio therapy are not very effective in GIST, so the need to search new methods of treatment is required. Target therapy has become one of the methods of choice and includes giving Glivec (imatinib-) protein tyrosine kinase inhibitor, suppressing the proliferation of Bcr-Abl-positive tumor cells, inducing their apoptosis. Multiple studies of III phase have proved the increase of relapse-free duration and increased 5-year-survival in this type of the tumor diagnosis.