Research Article - (2018) Volume 26, Issue 1
Tamiru Bogale
School of Nursing, Institute of Health, Faculty of Health Sciences, Jimma University, Ethiopia
Mesfin Beharu*
School of Nursing, Institute of Health, Faculty of Health Sciences, Jimma University, Ethiopia
Temamen Tesfaye
School of Nursing, Institute of Health, Faculty of Health Sciences, Jimma University, Ethiopia
Yeshitila Belay
School of Nursing, Institute of Health, Faculty of Health Sciences, Jimma University, Ethiopia
Corresponding Author:
Mesfin Beharu
School of Nursing, Institute of health
Faculty of health Sciences, Jimma University, Ethiopia
Tel: 251913872267
E-mail: laliistuubm@gmail.com
Submitted date: November 10, 2017; Accepted date: January 12, 2018; Published date: January 18, 2018
Background: Patient centered care has received a new emphasis in recent years due to the rise in health care demand. It is increasingly recognized as a key dimension of quality healthcare, but remains poorly implemented in practice. Despite the need to transform the existed health care delivery practice into patient centered care, few have dealt on the implementation of patient centered care practice in public health care organizations in the region.
Objective: The aim of this study is to examine the scope of patient centered care practice and to identify potential factors that drive or hinder patient centered care practice in public hospitals of Benishangul Gumuze regional state, South West Ethiopia.
Methods: Institution based Qualitative case study design was employed. Thirty-two purposively selected participants from different category were interviewed. Ethical clearance sheet was obtained from Jimma University ethical review board. Seventeen face to face in depth interview, two focused group interview, document review and systematic observation was conducted. Deductive analysis was employed manually to analyze text data.
Results: The analysis result showed that the concept of patient-centered care was perceived as; providing quality care, making partnership, provision of information, patient involvement and understanding patient preference. Patient centered care practice had occurred in the health care organizations.
Conclusion: Patient centered care practice in public hospitals had clearly occurred in some degree. However patient empowerment and family and friend involvement in patient care were found far from the existed practice and which was favored by low patient health literacy levels. Investing on the improvement of patient health literacy and staff capacity may fasten the transformation of the current health care practice in to patient centered care practice in the settings.
Keywords
Patient centered care; Hospitals; Care; Patient; Ethiopia
Introduction
The principle of patient-centered care is date back to the ancient Greek, which was interested in the particulars of each patient. Its popularity began to increase in the 1970s, coming to prominence. Patient-centered care is highly valued in the discipline of nursing. The origins of this value can be traced to Florence Nightingale, who differentiated nursing from medicine by its focus on the patient rather than the disease [1,2]. Patient centered care is defined as “respectful and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions”. “Patientcentered” means considering patients’ cultural traditions, personal preferences and values, family situations, social circumstances and lifestyles [3-5].
Patient centered care (PCC) is a care that is holistic, empowering and that recognizes the individual’s priorities and needs that important to all patients. According to the Picker Institute, patient-centered care has eight delineated dimensions, including: respect for the patient’s values, preferences, and expressed needs; information and education; access to care; emotional support to relieve fear and anxiety; involvement of family and friends; continuity and secure transition between health care settings; physical comfort; and coordination of care. PCC can improve quality of care and patient satisfaction, as well as reduce healthcare costs. Currently the approach gets the emphasis from health policy makers to make the health care system more efficient to achieve the need of the patient at the primary health care level and it has become a central for the nation’s healthcare system all over the world [4,6-8].
In Ethiopia, PCC is one of the priority areas of the health sector transformation plan (HSTP) under compassionate and respectful care (CRC) transformation agenda since 2015. As ministry of health, the need of PCC is expressed as “compassionate, patient-centered care is a top priority in our efforts to improve quality and equity in service delivery”. Different reasons leading the health care system into a trap of low productivity and higher cost with lower patient satisfaction rates [9,10].
Literatures show that PCC is currently a popular concept within health care across the nation’s health policy makers because of the improved patient outcomes; more emphasis needs to be placed on the actual implementation of the PCC principles. Patient-centered care is associated with improved overall health status of patients, improved health care delivery efficiency, improved perception of satisfaction, increased meeting of expectations, and improved quality and service excellence. PCC has been championed by the World Health Organization as a main component of high-quality care and identified as a priority for healthcare improvement across the continuum of care settings (i.e., primary, acute, rehabilitation, long-term and palliative care). The outcome of having a patient-centric demonstrates that patients will be more engaged in their care, resulting in a strong positive impact on loyalty among consumers, a stronger competitive advantage, and results in more treatment compliance [1,9-11].
Despite proven benefits of patient Centered Care, significant challenges still persist in its implementation across the globe. Its integration into clinical practice is often found to be patchy and inconsistent even in developed countries. PCC in Africa is increasingly recognized as a key dimension of quality healthcare, but unfortunately remains poorly implemented in practice. Poorly implemented PCC in sub-Saharan region is contributed by three distinct factors; the performance of providers, the structural and organizational features of the health system and the broader socioeconomic environment in which health workers operate. Traditionally, provision of care in developing countries including Ethiopia has been organized around the needs and desires of healthcare professionals, particularly physicians [12,13].
As a consequence the provision of healthcare service in Ethiopia is more biomedical than bio psychosocial. Study conducted in 2016 shows, 71% of healthcare providers admitted to failing to deliver compassionate and respectful care services and 77% of them acknowledged that they did not deliver compassionate and respectful care for every patient they encounter. Another study conducted in 2015 shows, patient satisfaction is not adequate and still 30% of patients at in-patient service were not satisfied by the services they received. The baseline assessment of the Ethiopian Hospitals Reform Implementation in some hospitals of the country also shows, the nursing standard of key performance indicators were still unmet and a system for coordinating and managing nursing staff was partially completed. This means out of the eight performance indicators for nursing care standard, only one has been partially completed, resulting in an overall compliance rate of 12.5% [14-17].
As a response to a growing demand of the patient need in the health care industry, patient centered care is considered to be crucial for a health care organization that provides caring, safe and high quality care and is described as holistic, non-judgmental, empathetic, respectful, and empowering. The achievement of patient centered care is indicated by service satisfaction of the patient .Improvement in the quality of hospital care is a fundamental aspect of health system strengthening that is directly linked to the service delivery dimension of the World Health Organization (WHO) building blocks of a health system. Ethiopia’s implementation of a national system for monitoring hospital performance is proofed as an example of a low-income country that aims to improve health service delivery via the creation of a culture of accountability and decentralization [18-23].
Currently, the Ethiopian Hospital Services Transformation Guideline, which is consistent with the national focus on quality improvement in health care, which are consistent with the Health Sector Transformation Plan. Subsequently, the country developed a hospital performance monitoring system based on achievement of key performance indicators and the Ethiopia Hospital Alliance for Quality. The first focus area of the EHAQ is patient satisfaction to measure the performance of hospitals across the country including labor and delivery quality [24,25].
Therefore the study was focused on examining the scope of patient centered care practice, and identify barriers and facilitators to practice patient centered care in public hospitals, by using manager’s, health care provider’s, supportive staff and patients’ perspective at the health care organization level and system level.
Patient centered care model
As the definition implies, the most important attribute of patient-centered care is the active engagement of patients. “Whole-person" care, Coordination and communication, Patient support and empowerment and Ready access were examined as feature of patient centered care framework by Bechtel and Christine. According to the Picker Institute and Harvard Medical School Eight Picker dimension of Patient-Centered Care, were identified. Which includes: Patients’ Preferences; emotional support; physical comfort; patient empowerment; continuity of care; coordination of Care, Access to Care, and involvement of family and friends [26,27].
The detail of each element of patient centered care model is summarized at Table 1. Patient centered care model of Picker Institute and Harvard Medical School were more accepted internationally due to its specificity and comprehensiveness. The investigator was used this model to examine the status of patient centered care practice in public hospitals (Figure 1).
| Main theme | Subthemes | Quotes |
|---|---|---|
| Scope of patient centered care practice | 1. Awareness of patient centered care 2. Respect for patient's values 3. Involvement of family and friends 4. Patient empowerment 5. Access to care 6. Emotional support 7. Physical comfort 8. Continuity of care |
“We have better understanding than our patient about the care we provide to them, for example, most patients need injection than oral medication; we have responsibility to provide adequate information about the advantage and the disadvantage of both routes rather than forcing them[…]” (Health care provider participant 2).“There is waiting area with television and chair for our patients during their waiting time […]” (Supportive staff participant 4).“I am diabetic patient, currently I have taken two tablets, but I have dizziness and I report it to health care providers, still I have no relief from this health problem” (Patient participant 3). |
Table 1: Summary of themes, subthemes and quotes scope of care Benishangul Gumuze Ethiopia, 2017.
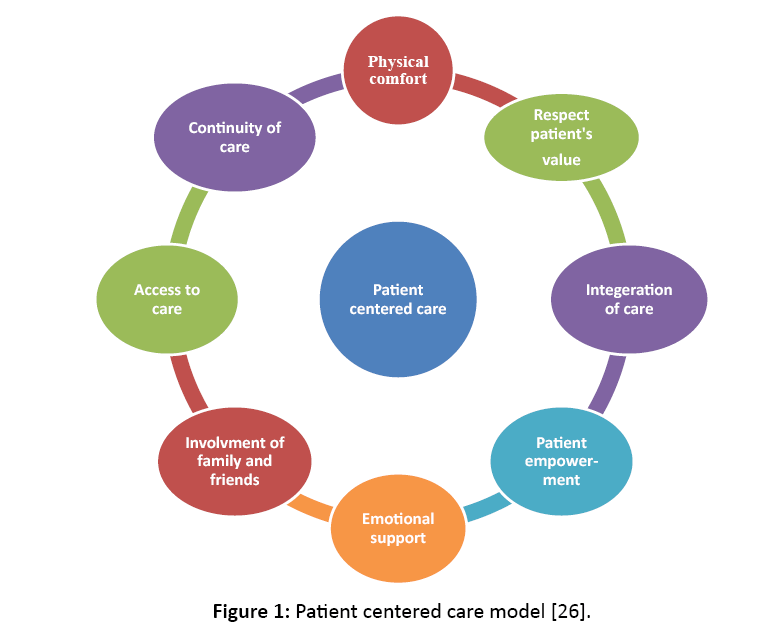
Figure 1: Patient centered care model [26].
Significance of the study
As the study was focused on examining the scope of patient centered care practice by using manager’s, health care provider’s, supportive staff and patients’ perspective in public hospitals. The finding can be used as bridge knowledge to fix the gaps that identified between the existing health care service delivery system and the patient centered care model in the public hospitals. The study will motivate the public hospital to improve service delivery practice by looking the identified gaps from the research findings and gives a chance to take attention to improve patient care and outcome. Finally, the insights obtained from the research findings can be used as base line data for fully implementation of patient centered care in public hospitals for those found in similar context across the country. It is also used as input for policy makers to optimize and strengthen patient centered care practice in public healthcare organizations.
Objective
General objective
The aim of this study is to examine the scope of patient centered care practice in public hospitals of Benishangul Gumuze regional state, South West Ethiopia.
Specific objectives
1. To explore the scope of patient centered care practice in the public hospitals.
2. To identify patient perception of level of patient centered care practice in the public hospitals.
3. To identify care providers perception of level of patient centered care practice in the public hospitals
Design and methods
The study was conducted in two public hospitals in Benishangul Gumuze regional state, South West Ethiopia, from March 1, 2017 to April 15, 2017. Assosa General Hospital is one of the public hospitals in the region, which is situated in Assosa town. The hospital was established in 1977 E.C and renovated in 1982 E.C. Pawe general hospital is one of the public hospitals in the region, which is situated in Pawe town, Metekle zone. The hospital was established in 1980 E.C.
Institution based qualitative case study design was employed because this study seeks to provide a rich understanding of the study phenomenon contextually. A sample that best represents the diverse source of information and opinions of those potential sources of information (52) was considered when choosing participants from both organizations. Therefore 32 participants from different category (health care providers, patients and administrative staff) were selected purposively. Two general managers (CEO), seven health care providers, four supportive staffs and four patients, totally thirteen staffs and four patients were participated in in-depth interview and fifteen health care providers were participated in focused group discussion. Data was collected by using multi-method strategy, which consists; individual interview, focused group interview, observation and document review.
Deductive analysis was employed manually based on patient centered care framework. Looking and reading of translated text data and field note was made repeatedly to familiarize with data. Different text highlight color was used to select similar concepts from the text data and to generate initial codes. Quotes were extracted from the text data parallary and stored separately. One hundred twenty codes was initially identified and reduced into eighty codes. Similar coded datum was assembled together. After conceptualizing of related coded datum, searching of categories among codes was made. Then initial category was made. After reviewing the initial categories, categorizing of the categories into predetermined theme was done. Finally interview result was written by compiling memos, quotes and analyzed data. The observational data of the three observers was tallying up on each item of structured observation check list on the column of fully practiced, partially practiced or not practiced. Then the observation result was analyzed qualitatively by item level using category system as fully practiced, partially practiced or not practiced and the result was written based on each section of the structured observation checklist. The document review data was analyzed and interpreted based on patient centered care framework. Finally, the analysis results of reviewed documents were written cumulatively. Finally, the interview results, observation results and document review result were triangulated.
The rigor of the work was maintained by using the following supportive operational techniques: collecting rich data by careful interview of individuals and groups from heterogeneous participants, and using multi-method strategy of data collection which consists; systematic observation reviewing of the interview guide by experts. Member check of the analysis result was made to check that the analysis result is exactly as participants’ experiences before writing of final result report by inviting to read the translated data for staff participants. All interviews was tape-recorded and noted on hard copy to provide back up. All data was stored by the principal investigator on pass word protected computer and hard copy in private room.
Prior to data collection ethical approval sheet and permission letter was obtained from Jimma University ethical review board and Benishangul Gumuze regional health bureau, respectively.
Results
The extent of patient centered care practice was explored by the experience of the respondents. The extent of patient centered care was examine with the element of patient centered care frame work; respect patient’s values, access to care, information access, patient empowerment, family and friends involvement, emotional support and continuity of care.
Awareness of patient centered care
The manager respondents and the health care provider respondents had awareness about the endorsement of transformational patient centered care policy in the country. A manager respondent one said that: “I heard it before one year this issue was one of health sector transformation agendas, ‘compassionate and respectful care’, patient centered care is included under this agenda as one component” (Manager Participant 1).
The respondents were perceived the awareness of patient centered care in different ways. But most of them share; providing quality care, making partnership with patient, provision of information, patient participation and understanding patient needs as a central concept for the meaning of patient centered care. The manager and supportive staff were perceived the awareness of patient centered care as providing quality to satisfy their patients. One manager supports this idea by saying that: “…in this hospital all staffs from cleaner to specialist has a responsibility to provide quality service to satisfy the patient, this is the meaning of patient centered care for me” (Manager Participant 2).
Furthermore, the awareness of patient centered care were reported by most health care provider respondents as providing quality care, making partnership with patient, provision of information, encourage patient participation and understanding patient need as a central meaning of patient centered care.
Respect for the patient’s values
Most of health care providers perceived that the patient’s preference and need are better under stood and respected while health service is provided for the patient in all healthcare organizations. They also agree on not to providing the wrong preferred care, because patient coming to the health care organization have asked both legitimate and illegitimate service request to receive their preferred care. The study participants raised that need and preference of the patient is influenced by different factors. Health literacy level of the patient and the culture of health care provision in a private health facility take a great share for this requesting of illegitimate health service from the patient side. Focused group discussion participant seven said that: […illegitimate service request is common in private health facilities, for example one patient may prefer X-ray with no relation with his/her health problems, because the requested service is provided only on the basis of patient preference, without considering the relation between the health problem and the diagnostic methods” (FGD1P7).
Despite a principle of patient preference and expressed needs that reported from most staff respondents, some of the patient respondents stated that all their preference and expressed need are not changed into actions as their voice. One of Patient respondent illustrate it as: “I am diabetic patient, currently I have taken two tablets, but I have dizziness and I report it to health care providers, still I have no relief from this health problem” (Patient Participant 3).
However showing respect to the patient further explained by focused group discussants as, it should be started from choosing words while they communicate with the patient. Greeting and involving the patient on decision is frequently reported opinions from respondents as a way of showing respect. One of focused group two discussant explain it as “To show respecting for our patient, we have participate them while we providing the care. We have also provided enough information about their disease condition and the treatment option” (FGD2P2).
Involvement of family and friends
Interviewees were noted well the need of patient involvement, but the patient and their family involvement on plan of care are not fully practiced and not as expected in the public hospitals. According to the manager respondents, there are systems that allowing the patient and their family to participate on their plan of care. However, little is practiced on the ground due to different reasons. One of the manager respondents explain it as: “[…in the other hand the patient and their families are not participated as expected, because most of them have information deficits about their care and their health status and even they did not ask the health care providers....]” (Manager Participant 1).
Most of health care provider respondents believe that, there are situations that the patient and their family involvement is a must. In the other view, some respondents belief that involving the patient and their family on plan of care is considered as time consuming task by few individual interviewees and focused group discussion participants. Focused group discussion one participant eight said that: “Sitting and discussing about everything with patient is unnecessary as me. For example, if you plan to do nursing care plan for your patient, the patient may participate by providing answer for my question, otherwise participating on the development of each nursing care plan is time consuming” (FGD1P8).
Patient empowerment
As most respondents’ view, system for information and education is placed in their organization, but the extent, the regularity and information utilization is under question mark and they believe that, the provision of health information is non-specific, most of the patient commonly hooked only on the curative aspect of service rather than preventive aspect.
As a principle, most of the respondents agreed that, providing health information to their patient is considered as a core activity in their organization to empower the patient regarding the health condition and care option. Health care provider respondent five reported as: “I agreed that information provision to the patient is important, for example the patient who knows about the requested laboratory test is different from patients who do not know about his /her requested laboratory test” (Health care Provider Participant 5).
Despite this principle, individual patient teaching is minimal and the time given for individual patient to teach them is also not enough to provide clear and specific information. In the other hand, the desire of the patient to use information from the available information desk as a source of information is almost none. Health care provider respondent seven said that: “…in our case the amount of time given for each patient is too small. Too general information is given only once, there is no chance to meet the patient again if they need, this is due to patient load” (Health Care Provider Participant 7).
Access to care
Most interviewees report shows that, different promotion and announcement method is employed to access care for the patient within the organization and outside the organization from paper based to electronic media. Community forum and catchment area review meeting are the common methods to promote the existing care and to announce the newly starting care. The manager respondent one said that: “…different strategies are made in our hospital as well as outside the hospital, quarterly catchment area review meeting, community forum and sometimes formal letter was used to promote the existing service and to announce the newly started services.” (Manager Participant 1)
In addition to the commonly used methods, posting health service menu at visible area and Local FM radio is also sometimes used in one of the two organizations. Supportive staff respondent three said that: “Efforts were made to make the accessible for our patients, in addition to posting of health service menu; sometimes the services are promoted by local FM radios to the community.” (Supportive Staff Participant 3)
Emotional support
The extent of fear and anxiety, and mechanism of emotional support to relieve fear and anxiety is reported by most respondents and they agreed that, most of the patient visiting the health facility for the first time is very distressful by searching their respective service units. Focused group discussion two participant two said that: “We provide direction for those patients who have difficulties to reach the respected service units, because our patients commonly develop fear and anxiety due to difficulty of reaching their respected service units” (FGD2P2).
Most respondents perceived that, reassurance and guiding the direction of their respective service unit for the patient is the common remedy to relieve fear and anxiety. The emotional support is not only the responsibility of some service staff; it is a responsibility of all the staffs of the organization.
Most of the patient respondents reported that, emotional support is provided by hospital staffs and most of emotional support is related with reassurance and information provision. Patient respondent two said that: “I was admitted with appendicitis, my first arrival was at card room then to the emergency department, the doctor advise me not to fear, and he said that ‘it is simple, surgery will be done soon and you will return back to your home” (Patient Participant 2).
Physical comfort
Most respondents believed that, providing comfort for the patient is varied from physical comfort device to anti pain. Hospital beds, waiting area with television and lounge are frequently listed by health care provider as a common comfort measures for the patient. Supportive staff respondent four said that: “There is waiting area with television and chair for our patients during their waiting time…” (Supportive Staff Participants 4)
Continuity of care
Effort is made for the continuity of care and to secure transition between health care settings, which ranges from financial support to availing of transportation for referral. By most respondents, information is seen as an engine for the continuity of care within the health care organization and outside the health care organization. Guiding and providing information, availing ambulance for referral and providing appointment card are the common methods that employed in hospitals to secure the continuity of care. As some respondents, financial support is made by the social committee for twenty four hours only. But it is informal and not consistent. Manager respondent two said that: "Sometimes the social committee of our hospital is providing financial support for patients those who can’t afford cost for their health care for only twenty four hours." (Manager Participant 2)
Different stakeholders are involved for continuity of care, but liaison, referral and social service, and runner play a great role to facilitate continuity of care. In this regard, health care respondent three said that: “…the liaison communicate with the liaison of other health facilities as an agent to facilitate referral system, like checking the availability of bed from the referral health facilities and the availability of bed from our hospital to receive referral from other health facility and they also arrange ambulance for referral” (Health care provider participant 3).
Discussion
In Ethiopia, patient centered care is a component of compassionate and respectful care (CRC) agenda in the health sector transformation plan since 2015. However the inclusiveness of patient centered care as a quality dimension in the health delivery system was date back to 2010. Slow pace is seen between the respondents’ awareness regarding the patient centered care policy endorsement in the country. In the other hand, lack of patient centered care training for organization staffs play a great role on this limitation. Patient-centered care in healthcare context is defined as care provision that is consistent with the values, needs and desires of patients and is achieved when health care providers involve patients in healthcare discussions and decisions [3,28]. In this study, the concept of patient-centered care was perceived as; providing quality care, making partnership with patient, provision of information, patient involvement and understanding patient preference even if slow pace seen on the ground/truly practiced.
The study conducted in South Africa shows, patient-centered care was perceived as an awareness of the importance of the patient's culture, involving the patient's family, incorporating values of love and respect, optimal communication in all facets of patient care and accountability to the patient. According to international alliance of patients’ organization (IAPO), in clinical point of view, patient centered care is a useful concept if its definition is used to ensure the patient needs and preferences and it is at the center of all aspect of patient care. The concept of patient centered care in this study is supported well by other previous studies. However the involvement of patients’ family and friends were not a well-practiced in this study area unlike that of study conducted in south Africa. Most of staff respondents have not received patient centered care training ever.
Based on systematic interview and systematic observation of each feature of patient centered care framework, patient centered care practice had occurred in the public health care organizations by both perceived and observation data. In all aspect of most respondents’ experience, the patients’ literacy level is raised as a reason for not occurring of the patient centered care practice as expected. Patient empowerment is a necessary process towards a patient-centered care approach [28].
A key component of patient centeredness is patients’ access to accurate and high quality information about their disease and the treatment options available to them. Despite the inclusiveness of patient centered care in the health care quality as one dimension in the health care delivery system, the practice of patient centeredness in public hospital is found on up and down motion and the stated patient centered care in the health care delivery system was lack detail description of framework and integrity to understand and exercise patient centered care practice in the healthcare organization context. So that this up and down motion of patient centered care practice was hampered by lack of specific and comprehensive patient centered care guidelines and poor communication of the organizational value and vision within the healthcare organization.
Limitations
The generalizability of this finding is limited to the setting of this study. There might be respondents bias and recall bias.
Conclusion
Patient centered care practice in public hospitals had clearly occurred in some degree. However patient empowerment and family and friend involvement in patient care were found far from the existed practice and which were favored by low patient health literacy levels. Information related factor, stakeholder and partner support, service expansion, monitoring and feedback mechanism, and national policy were identified as perceived facilitators. In contrast patients’ health literacy level, health care provider characteristics, patient empowerment, shortage of resource, organizational capacity, shortage of specialty care, managerial skill, legislation related factor and organizational culture were identified as a barrier to practice patient centered care in public hospitals of the region.