Key words
clinical practice, life narratives, Puerto
Rican doctors, religion, spiritism, spirituality
Introduction
There is a large literature on pastoral care at the end of
life, and on patients with terminal illnesses such as
advanced cancer, that focuses on patients’ spirituality and/or religious beliefs (Puchalski, 2006; Holmes et al,
2006). Medical doctors are now being viewed as agents
who may employ spirituality and its potential benefits for their patients. However, doctors’ particular kind of
spirituality or religiosity, as related to their culture, is
seldom taken into account (Koenig, 2007a,b). Few
studies have examined how their spirituality or religiosity
affects their relationship with and treatment of
patients, or how patients perceive these spiritual or
religious doctors (Sulmasy, 2006). This is an important
issue because the physician–patient relationship is
central to medical care. The inclusion of spirituality
and/or religion promotes a more humane and patientcentred
perspective on clinical care, although it is not
clear whether the effect is physiological or psychological,
or both (Curlin et al, 2005).
Olson et al (2006, p. 234) conducted a qualitative
study based on in-depth interviews with family medicine
residents in the south-western USA. There was
almost unanimous agreement that openness to spirituality
was important both to patients’ health and to
the physician–patient relationship. The residents also
agreed that addressing spiritual issues required sensitivity
and patience, as well as ‘tolerance of ambiguity’
and sensitivity to ‘one’s own spiritual place.’ The
residents’ own spirituality related to whether or not
they addressed spiritual issues with patients. Several
medical schools in the UK (Bell et al, 2010) employ a
‘Wholeness ofHealing’component to introduce medical
students to the spiritual dimension of healthcare, to
encourage them to adopt a holistic approach to
treatment, and to promote an appreciation of diversity
in religious beliefs and spiritual practices among
patients. However, reports of these programmes do
not discuss the medical student’s own spirituality.
Although there are a number of general discussions
and reports about spirituality in medicine (e.g.
Puchalski, 2006), there have been few qualitative studies
of clinical medical practice and spirituality/religiosity,
either in the USA or in Latin America. This is a serious
omission, as current evidence from Brazil (Bragdon,
2011; Lex, 1985), Venezuela (Matos-Romero, 1983;
Novich Hernandez, 1999) and Argentina (Marin˜o,
1963) shows that many Latin American doctors believe
in and communicate with spirits, a type of
spirituality that is largely unacknowledged yet also
present in the USA.Moreover, the cultural patterning
of the doctor–patient relationship has barely been
examined.
This paper reports on a study that aimed to examine
issues of spirituality among a group of Puerto Rican
doctors. It explores the general theme of the cultural
patterning of the doctor–patient relationship as related
to spirituality and religion. In this paperwe focus
on the doctors’ perspectives on the presence of spirituality
and religion in the clinic,we explore the various
types of spirituality and we examine their relationship
to seldom discussed aspects of the doctor–patient
relationship, namely empathy, intuition and psychic
faculties, prayer, and the presence of and interaction with spirits. An important hypothesis in our study was
the idea that there is a link between spirituality and
empathy among healthcare providers, and that this
link is essential to an effective doctor–patient relationship.
Empathy has been identified as one of three core
values necessary to establish an effective doctor–
patient relationship (Newton et al, 2008). However,
although attempts are made to foster empathy in
medical students, there is a continuous decrease in
visceral empathy, defined as ‘emotional’ empathy, versus
‘imaginative’ or cognitive empathy, during the first
three years of undergraduate medical training; in fact,
empathy is often stunted during this period (Pedersen,
2010, p. 593; Newton et al, 2008).
The overall goal of our study was to illuminate
an important life arena where the strong separation
between medical science and religion/spirituality is set
aside in the interest of fostering and responding to an
acknowledged, but unplanned, spiritual healing force
within a conventional medical–clinical context. The
focus in this paper is on the relationship between
science and religion in the lives and work of doctors;
spiritual experiences may initiate and/or enhance
caring clinical behaviour in medical professionals
(Koss-Chioino, 2006a).
Definitions
Few authors agree on how spirituality and religiosity
should be defined (Paloutzian et al, 2005). In this
study we applied the broad definitions proposed by
Kenneth Pargament and his colleagues in the American
Psychological Association’s APA Handbook of
Psychology, Religion, and Spirituality. In Pargament’s
view, religiosity refers to:
beliefs, practices, relationships or experiences having to
do with the sacred that are explicitly rooted in established
institutionalized systems or having to do with the psychological,
social or physical functions of beliefs about the
sacred; spirituality refers to beliefs, practices, relationships
or experiences not linked to established institutionalized
systems or when referring to the human motive
to develop a relationship with the sacred.
(Pargament et al, 2013, p. 5)
It is important to observe that what is deemed sacred
varies among different groups and cultures. We attempt
here to show how diverse types of spirituality
(i.e. religious beliefs and practices such as prayer,
entering or progressing on a spiritual path and/or
belief and contact with spirits) reported in the clinical
practice of conventional medicine by Puerto Rican
doctors vary between three groups self-identified as
spiritist, spiritual or religious.
Doctors and religiosity/
spirituality
Harold G Koenig, a noted psychiatrist-geriatrician
researcher in the field of religion and medicine, has
written extensively on the benefits of including spirituality
and religion in patient care across all sectors of
the healthcare system (Koenig, 2007a,b). He argues
that, allowing for factors such as their religion, their
degree of religiosity and the severity of their illness, a
high percentage of patients think that their doctors
should discuss their religious and spiritual needs. A
smaller number want their doctors to pray with them.
In a national survey conducted in the USA, 55% of a
random sample of 1144 physicians stated that it was
usually or always appropriate for the doctor to enquire
about the patient’s religious or spiritual beliefs; less
than 50% stated that it was inappropriate (Koenig
2007a,b). However, only 10% indicated that they often
or always enquired about the patient’s religious or
spiritual beliefs. It must be noted once again that
praying with patients depends upon the religiosity
and/or spirituality of the doctor; 76% of this sample
who identified themselves as highly religious prayed
with patients. However, only 19% of the entire sample
sometimes or always prayed with patients. Most
doctors felt that it was appropriate to pray with the
patient only if he or she was very sick and initiated the
request.
Spiritism, spirituality and doctors
There are perhaps thousands of doctors in Latin
American countries who experience spirits and/or
attend ritual sessions in which spirits are present; this
is termed spiritism. Most follow the teachings of the
French scholar, Allan Kardec (1803–1869), but many
also follow the teachings of re-interpreters of Kardec’s
writings, such as the Spanish philosopher, Joaquin
Trincado (1856–1935), who lived and died in Buenos
Aires. It might be noted that most spiritists, especially
educated individuals, do not consider their system to
be a religion, but rather a philosophy integrated with
moral and scientific objectives (Koss-Chioino, 2006b).
Doctors who are spiritists are probably most numerous
in Brazil, where 2.5 million people declare that
they follow spiritist doctrine (Instituto Brasileiro de
Geografia e Estatı´stica (IBGE) Census of 2000).
Brazilian doctors have organised a spiritist medical
association (Asociacion Medico-Espirita de Brazil,
also de Internacional) that sponsors national and
international conferences. Reporting on the first conference
in Brazil, in 2005, the Association’s magazine
quotes from Koenig’s plenary address: ‘The last 100– 200 years of separation between science and religion
are arriving at an end. Medicine is stirring up another
vision; a human being is not only a physical body’
(Salud y Espiritualidad, undated; www.thespiritist
magazine.com, translated by the authors from the
Spanish-language version of the conference report).
The concept of spirituality refers to a universal
experience and process of seeking the sacred as defined
in varying ways within cultures. For spiritists the
sacred involves spirits, including one’s own spirit and
others of many types (e.g. deceased relatives, famous
individuals, and those spiritswho seek out an incarnated
spirit in order to redeem themselves of misdoings or
emotional difficulties). Spiritism is based on the view
that the visible world is surrounded by an invisible
world inhabited by spirits who influence human
behaviour (Comas-Diaz, 1981). It is considered by
practitioners variously as a religious, ideological, healing,
philosophical and/or scientific system in Latin
American countries (Koss, 1987; Martinez-Taboas,
2005). These influences may have a positive or negative
effect, depending on the spiritual progress of the
spirits involved. This process is based on the belief in
reincarnation which permits each spirit to evolve
through multiple lives.
Spiritist doctors appear to demonstrate a heightened
capacity for empathy with patients, related both to
their commitment as healers (a few of them are also
spirit mediums) and to their ecstatic experiences of
spirits, which are reported to occur occasionally during
clinical encounters, but more frequently during other
life experiences (Koss-Chioino, 2006a,b). Davis-Floyd
and St John (1998, p. 100) define empathic behaviour
in the doctor–patient relationship as the ‘ability to
understand another’s reality.’However, empathy among
these doctors has more to do with emotions, including
compassion, feelings about loss, and a deep identity
with bodily feelings and sensations (for a discussion of
the importance of empathic behaviour on the part of
doctors, see Astrow et al, 2001).
The study
The focus of the present study is on the therapeutic
relationship between doctors and patients, akin to
what has been called ‘medicine of the person’ (Cox
et al, 2007). The study took place in Puerto Rico and
aimed to explore how medical doctors who were
trained in diverse medical disciplines (excluding psychiatry)
integrated spirits and spiritist beliefs into
their lives and clinical practices, compared with doctors
who were spiritual/religious in other ways. In
particular we aimed to determine how a spirituality
that involves spirits, reincarnation and a doctrine of
universal evolution of the spirit through good works is integrated into clinical work and affects patients’
perception of and relationship with their doctors.
Spiritist doctors’ views were compared with those of
a matched group of doctors (and their patients) who
were not spiritists but who were spiritual in other
ways, including being deeply religious. It is of interest
that the doctors who were spiritists were either socialised
into that philosophy during childhood, or experienced
spontaneous, anomalous experiences of
spirits during medical training and/or later in life.
Conduct of the study
The study was approved by the Institutional Review
Board of Arizona State University (October 2008).
Sampling
We used snowball sampling to recruit 40 doctors in
the San Juan metropolitan area; 28 of these individuals
self-identified as spiritists, and we classified the rest as
spiritual because they readily described one or more
types of spirituality in their clinical work and/or their
personal life. Referrals from the first 40 doctors enabled
us to recruit a convenience sample from outside the
San Juan metropolitan area. In this second sample
there were five spiritual doctors, and 13 doctors were
religious. They attended various churches regularly
and described their beliefs and practices. One doctor
did not mention either spirituality or religiosity. We
then recruited a third sample of 15 doctors at random
from telephone directory lists in all areas of the island.
In this third sample there were five spiritual doctors,
eight doctors were religious, and two did not discuss
either religion or spirituality. In total we recruited 74
doctors (25 women and 49 men), aged between 33 and
83 years and matched by specialty. They self-identified
as spiritist (n = 28), spiritual (n = 22) or religious (n =
21). Most (n = 72) worked in private practice, and two
worked in the Emergency Room. Finally, we recruited
a convenience sample of four patients from each
doctor.
Methods
We conducted semi-structured interviews, 45 to 90
minutes in duration, with each doctor. Informed written
consent was obtained prior to each interview. With six
exceptions, the interviews were conducted in the
doctors’ private rooms. Each doctor was also asked to
complete the Ironson–Woods Spirituality/Religiousness
Index (Ironson et al, 2002).
Patients were asked to complete a questionnaire
that focused on empathy and the doctor–patient relationship as a basis for comparing the effect on
patients of ideas and clinical practices relating to
spiritism, spirituality and religiosity.
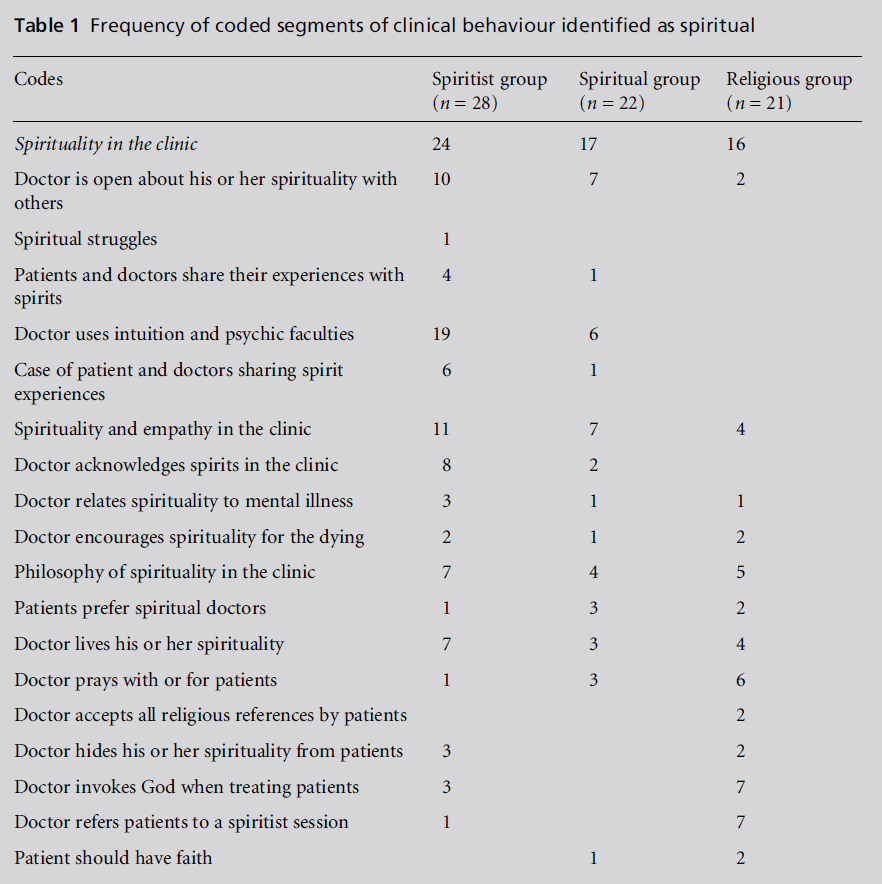
Data analysis
This paper focuses only on the interview data. Interviews
were tape recorded and transcribed verbatim.
Inductive coding was carried out jointly by the authors
on a consensus basis using a grounded theory approach.
First, a set of major themes was coded. Those
themes that contained the most frequent responses
were further coded with subcodes. Frequent subcodes
were in turn subdivided into sub-subcodes. This
process produced a total of 120 codes arranged under
eight major themes. The data for this article were
drawn mainly from a very frequent subcode, namely
spirituality in the clinic. This subcode had 19 subsubcodes,
as illustrated in Table 1, which shows the
distribution of the sub-subcodes by doctors’ groups.
Findings
The results of the Ironson–Woods Spirituality/
Religiousness Index will be reported in more detail
elsewhere. Although the doctors achieved quite high
scores on indicators for both spirituality and religiosity,
there were no significant differences in the levels
of spirituality or religiosity between the three groups.
The results of the patients’ questionnaire will be
reported elsewhere, but it is of interest that all of the
patients rated equally and were positive about all of the
three groups of doctors.
The findings from the interview data showed that
spiritist and spiritual doctors shared roughly similar
profiles of clinical behaviour, but religious doctors
differed. Reports of the use of intuition or other
psychic faculties (19 out of 28), and openness with
patients and colleagues about spirituality (10 out of
28), were most frequent among spiritist doctors, but
less frequent among spiritual doctors (6 out of 22 and
7 out of 22, respectively). Only two religious doctors
said that they were open about their own spirituality
with patients, and none of them reported the use of
intuition or psychic faculties. A number of spiritist
doctors reported seeing spirits in the clinic, as did two
spiritual doctors, but none of the religious doctors
mentioned spirits. However, seven of the religious
doctors referred patients to spiritist sessions. Among
the religious doctors, praying with patients, invoking
God during a clinical encounter, and respecting all
types of religious beliefs were frequent concerns. Clinical
behaviour was similar in all three groups with
regard to the number of doctors who reported their concepts of spirituality as relevant to clinical work,
and about living one’s spirituality, but the contents of
these behaviours or views varied considerably; specific
issues are described below.
Table 1: Frequency of coded segments of clinical behaviour identified as spiritual
Concepts of spirituality in the clinic
We were interested in how these doctors conceptualised
what they labelled as ‘spiritual’ in both their
own and their patients’ views and behaviour. Most of
the doctors referred to spirituality as affecting their
relationship with patients. Religious doctors who
identified themselves as Catholic, Baptist or Evangelical
described the need for what seemed to be a general
type of spirituality in their encounters with patients,
but one not necessarily attached to any particular
doctrine. One very devout doctor stated that ‘Spirituality
is embedded in everything we do, so is part of us everywhere.’ Another justified his use of spirituality in
the clinic by saying ‘We want to do the things that
make people feel better.’ Seven doctors in this group
referred their patients to spiritist sessions. A devout
religious doctor explained that ‘When one enters the
faith, you begin to see the patient with compassion,
with more charitable feelings, with more involvement
... not simply as part of a medical plan.’ Spiritual
doctors also emphasised the importance of spirituality.
One of them asserted that ‘You cannot be
scientific if you are not spiritual; it is difficult to
connect with another person; I have had better results
with the spiritual.’ When describing the use of spirituality,
another doctor reported: ‘I try to put my hand
[on the patient] in order to calm him but also maybe
to transmit positive energy. ... I believe in touching ...
and even if you don’t do anything mentally, it helps.’
One doctor described having an open Bible in an area of his office where he explained his diagnosis and
treatment plan. If he saw a patient reading the Bible, or
if the patient referred to it, he utilised this to benefit
the patient: ‘Why? Because I know that that patient
will feel more recognized, more committed and will
comply more with the treatment.’ Spiritist doctors did
not readily talk about spirits; some used ‘energy’ as a
proxy term. Several expressed their caution about
referring to spirits when speaking with patients. Indirect
references were made, such as ‘You have to heal
with energy ... because there is an energy level ... that in
some manner there is a connection between body and
spirit that will aid the healing, even the physical.’ This
doctor went on to add that it ‘helps communicate with
the patient and aids the spirit to be calmer.’ A young
woman doctor reported that her spirituality helped
her to be calm, ‘at peace’ and at ease with patients; this
ease was communicated to the patient, so that their
spirit was also calmer. Several of the spiritist doctors
identified their clinical work as running parallel to
spirit healing sessions. One claimed that doctors must
be more spiritual than other people in order to convince
all kinds of patients that their ways of thinking
must change in order for the doctor to be able to enter
into their illness. An older woman doctor, who regularly
attended spiritist sessions and was very involved
in several spiritual disciplines, reported that her
grandfather’s spirit helped her to heal patients with
his energy, as did the ‘Supreme Father.’
Doctors acknowledging spirits in the
clinic
Reports about this came mostly from spiritist doctors,
although some spiritual doctors did not appear to rule
out the presence of spirits, and even referred emotionally
distressed patients to spiritist sessions. Eight spiritist
doctors reported experiences of spirits in their clinic;
this was fewer than expected. A direct statement about
the involvement of spirits was made by one doctor:
‘Asked how I made a certain diagnosis, I said that it
was a spiritual diagnosis, that spiritual doctors had
given me insight ...’ A woman doctor declared that she
could not deny to her patients the times she saw spirits
with them in her clinic. Another doctor reported that
she saw an older man whose facial structure was like
that of her deceased grandfather. He was closing in on
them in order to listen to the patient. Several doctors
recalled experiences with helpful phantom personnel
in the hospital (e.g. a deceased head nurse) during
their training years. One doctor reported the inevitability
of the souls of people who had suffered traumas,
especially traumatic deaths, being present in clinics
and other places because they ‘did not arrive at the
place they had to’ (a spiritist belief). It should be noted
that most of the spiritist doctors who reported these experiences did so with some hesitation, as if they were
expecting a negative reaction. Attitudes towards spiritism
and spirits among Puerto Rican professionals are
complex; there is both belief and some denial related
to historically entrenched social repression. This issue
will be discussed elsewhere. Only two spiritual doctors
reported their experiences with spirits, but they were
careful to state their lack of certainty about them. To
quote one of these doctors, ‘Yes, it is possible, I can’t
deny it. I have felt it, noted it, perceived it, [its] odours,
something in the environment, but I don’t know.’
Religious doctors did not mention spirits in the
context of working with patients.
Doctors praying with or for patients
Koenig (2007b, p. 164) claims that a brief prayer can
be ‘very meaningful’ to religious patients. However, in
his view, the patient should initiate a request for
prayer and supply the topic; the doctor should at least
let the religious patient know that he or she is open to
prayer. The doctors often took the initiative if they
were highly religious and prayer was integral to the
way that they practised medicine or they felt that the
patient would benefit from prayer. Moreover, some
doctors described using prayer to maintain their own
well-being. Only 6 out of 21 religious doctors mentioned
prayer. A doctor who was also a Baptist
minister asserted that ‘We pray together here. And I
always pray before seeing my patients and meditate
some minutes before beginning.’ Another doctor
added that ‘If a patient is very sick ... I carry him in
my mind and pray for him.’ Another said ‘When we
pray each day at the office or the hospital ... this place
stays impregnated with the prayer and the faith. Even
if a patient doesn’t believe in anything or has another
type of belief, he receives the blessing ... he is more
agreeable, talks, listens and is more compliant.’ Among
the spiritual doctors, only three reported that they
prayed for or with patients. One reported praying
every day because ‘A healer has to pray to maintain
strong energy ... the patients take a lot from you.’
Another prayed for each patient and called for the
presence of God to heal. Only one spiritist doctor
mentioned that she prayed with her nurse that a
terminal patient would ‘go in peace.’
Use of intuition and psychic faculties
In total, 19 out of 28 spiritist doctors reported the use
of special faculties during clinical encounters. These
faculties affected the diagnostic process by adding a
special spiritual dimension aimed at complementing
rather than replacing conventional medical procedures.
Gilson Roberto, a Brazilian doctor who is also a
spiritist medium, focuses on the faculty of intuition as central to mediumship. He defines intuition as a
‘very common psychic phenomenon’ which is ‘like a
window that opens onto another dimension’ (Roberto,
2011, p. 150). He reminds us that Jung regarded it as
one of the four major functions of consciousness, and
the philosopher Henri Bergson developed a theory
that there are ‘two ways of knowing an object ...
through concept and through intuition.’ Roberto
(2011, p. 150) notes that intuition was a more widespread
faculty in certain cultures prior to the diffusion
of a materialist world view that focuses on cognition
and science. He considers that it is more difficult now
to explain what is ‘out of the ordinary’, that is,
communications from the spirit world. However, he
claims no ‘antagonism’ between ‘his academic training
and activities as a medium.’ Rather he sees them as
complementary, since mediumship provides ‘elements
(e.g. intuition) to analyze the information’ acquired
through clinical work (Roberto, 2011, p. 153).
Spiritist doctors endorsed intuition and psychic
faculties through various metaphors and descriptions.
A gynaecologist described the situation of a patient
coming in for a routine visit and lacking symptoms.
She ordered a sonogram, which revealed a tumour,
only because she had sensed it. She attributed this
prediction to ‘a pain in my soul (alma) because when I
see the patient I have like an uncomfortable sensation
with her.’ Another doctor spoke of knowing about a
patient’s problem, without the patient having verbalised
it, because it came ‘from the heart’; yet another
referred to the ‘clinical eye.’ In all of these experiences
there is a sense of something mystical, a sense of
knowing that is beyond rational control and medical
science. Most spiritist doctors rarely spoke directly
about these experiences, but regarded them as evidence
of spirit intervention. One doctor explained
that these feelings were ‘not energy, nor due to passing
hands over the patient and producing warmth ... it
isn’t something that ... is physical, it’s something that
you are unable to explain.’ Other descriptions included
the following: ‘There is something that guides
me [in making an unlikely diagnosis]; to me it comes
as a surprise.’
One variation on the role of psychic experience in
the clinic was the knowledge that someone important
to the patient had died without the doctor having any
prior knowledge of the relationship of the deceased to
the patient. A paediatrician commented that traumatic
events that had occurred while the patient was
still in thewomb could be the cause of a current illness,
and that the event could be healed in the clinic. This
perspective is consistent with spiritist beliefs about the
evolution of the spirit, namely that each life is an
opportunity to evolve and to improve morally.
Only six spiritual doctors reported intuition and
psychic faculties. One of these doctors, who considered
himself a healer, reported that before he sat down with a patient, and before he saw their chart, he
looked into their eyes: ‘If the patient is not looking at
me I feel it and later try again, but generally the patient
feels it [a spiritual connection].’ Several doctors claimed
to know the patient’s complaint ‘when they are coming
in the door’ and before examining them. One doctor
described this faculty as ‘a feeling, like an insight. For
example, he arrives and I feel it – it’s not something I
can stop. When it starts it flows and involves the
patient while I work [on him] ... healing.’ Another
doctor explained that ‘My spirituality is an intuition ...
a very strong and positive intuition.’
These reports illustrate a significant difference between
biomedical conventional treatment and spirituality
in the clinical encounter. The spiritual force,
however conceived, comes unbidden to the doctor or
patient and provides insight either beyond or complementary
to orthodox medical approaches. It cannot
be anticipated or planned; in order to gain more
control over a patient’s illness, the doctor must be
persuaded by the new information provided by spirit/
spiritual agencies or awareness. As shown in Table 1,
25 doctors appeared to accept these phenomena mainly
as an aid to diagnosing illness.
Empathy in the medical relationship
Many of the doctors in all three groups regularly made
home visits to ill, elderly patients. They were available
at critical moments by telephone at weekends or in the
evening, and many of them held weekend office hours
and clinics. They did not report that they solicited help
from the spirits or from God, but they stated that they
responded when contacted by spirits or mystical
feelings, which could include the Holy Spirit, on
behalf of a patient.
There is now a plethora of meanings and explications
of empathy in psychology and other literature.
For example, in the social psychological literature
the concept may be referred to as ‘social insight’,
‘interpersonal sensitivity’ or ‘interpersonal judgment.’
Although empathy has for decades been a focus of
client-centred therapy (Rogers, 1957, 1959), psychoanalysis
and object relations work by Hans Kohut
(1984), there is now growing interest in it as a
component of the clinical process. Empathy is now
seen as going beyond the idea that it is useful only as
a ‘kindly and supportive posture’ in establishing a
therapeutic relationship (Bohart and Greenberg, 1997,
p. 4). Elliott et al (2011, p. 43) described empathy as
three sub-processes: first, emotional simulation that
‘mirrors the emotional elements of the other’s bodily
experience’; secondly, a conceptual ‘perspective-taking
process’; and thirdly, an emotion regulation process
that soothes another’s pain. All of these processes were
referred to by some of the doctors in our study. In addition, emotional simulation may be an entry into
the doctor’s feeling what the patient is feeling, which is
the first step in a process I have referred to as ‘radical
empathy’ (Koss-Chioino, 2006a). Moreover, comments
from doctors in our study suggest some important
differences, at least for Puerto Rican doctors,
between physician empathy and empathy in psychotherapeutic
relationships. Pedersen (2010, p. 597)
makes a definitive statement about empathy in the
clinic with which many Puerto Rican doctors would
agree: ‘Empathic understanding is needed not only to
understand the patient’s illness or emotional reactions,
but also to understand what is at stake for the
patient and to diagnose and treat the patient adequately
... and [also] to throw into relief the patient’s
and physician’s horizon.’
Of the four religious doctors, one set the tone of his
relationship with patients by saying ‘Without love
there is nothing but a contract. I love my patients.’
For another it was important to recognise that the
‘patient, as a human being – mind, soul, body and
spirit – needs this compassion, this identification –
then you begin to hear the patients, find them ... you
begin to feel the spiritual part more deeply.’ Other
religious doctors had more of a cognitive, role-playing,
conceptual orientation towards empathy with a
patient: ‘I think about the other person and ... what
is happening – as if I had the same situation – and it is
part of spirituality.’ Another religious doctor said ‘It is
important to help the patient understand his own
spirituality.’
More of the spiritual doctors (7 out of 22) volunteered
statements about empathy in their relationships
with patients. They described deep bodily feelings. One
woman was explicit about her visceral identification
with her patients: ‘He comes in and I can tell from
what I feelwhat he is going through and I can feel what
he needs.’ Two other women gave the following
explanations: ‘I never say it but they [patients] know
that if I touch them I feel the pain ... my hands heal’
and ‘After I see the colour [i.e. the aura], after I feel the
illness with my hands, I perceive it [their emotional
state] in me ... it’s like here inside.’ Another woman
stated that ‘It is like a magnetic field, as if I was a sensor
of some magnetic field.’
These statements appear to be ‘radical empathy’ in
which soul pain, bodily pain, deep inner feelings and
emotions and/or spiritual knowledge of a person’s life
experience are involuntarily felt within another individual.
It is as if the boundaries between patient and
doctor are blurred or even completely erased (Koss-
Chioino, 2006b).
Among spiritist doctors a typical approach to healing
as a healer was reported by one doctor: ‘What has
manifested in me is the ability to feel and know the
personal life of the patient. I don’t always succeed
because there has to be affinity.’ Spiritist doctrine was also evident in the views of another doctor: ‘How do
you console an adult who has lost his mother or father
or other family member? The body doesn’t die, nor
does the spirit. The spirit will always be with you and
love will always exist between the two [persons].’ A
third doctor expressed another tenet of spiritism in
relation to empathy with a patient: ‘She is very special,
but we have a brutal connection. I don’t know what
happened in [her] past lives. I believe in reincarnation.’
Commenting on empathy, one doctor quoted
his elderly patients as saying ‘Doctor, it is you. You
come to the house and I amwell.’ For this doctor itwas
the trust that patients had in him: ‘It’s not the
spirituality that I bring, it’s the empathy I have with
these patients and they with me.’ For him, the curewas
‘more than 50% empathy.’ There were also reports of
deep emotion in relation to and with patients, especially
if the patient was dying: ‘I have been able to cry
with patients when one is dying ... and have been
known to close myself in a room to cry, because I
cannot hold back the feelings of deep upset for the
patient ... if you have to cry – well [you] cry.’
Conclusion
The contention of Puchalski and her colleagues
(Astrow et al, 2001; Astrow and Sulmasy, 2004), namely
that the healthcare professional needs to examine the
sources of meaning and value in their work and
cultivate empathic relationships with patients, focuses
on the role of spirituality and/or religion as a source of
personal centring and renewal. In one study (Craigie
and Hobbs, 1999, p. 581), a family practitioner reported
that ‘I gain strength, remain at peace and sometimes
experience inner joy when things don’t look so good.’
This is similar to what spiritist doctors express, but
they have also accepted a doctrine that goes beyond
these feelings, since their medical work acquires moral
meaning related to an existential perspective on life
that is not at all common in conventional medical
practice. According to spiritist doctrine, healing work
helps one’s own spirit to evolve, and to move up
towards the light of humanistic values. The doctor,
through his or her work, assists spiritually receptive
other-patients to move upward on the same sacred
trajectory.
What all three types of doctors who are spiritual
and/or religious report is that they bring to their
clinical work what might be characterised as a bridge
between ordinary and extraordinary human consciousness.
This is especially the case for many of the
spiritist doctors who experience the spirit world. With
all doctors it is a way to transcend the less than precise
application of the science of clinical medicine, and is
particularly valuable in situations in which patients are under great stress. Moreover, the relationship
between doctor and patient takes on a deeper, more
emotional dimension that speaks to an affinity, a
deeper connection between two human beings.
Touching and/or embracing are at times part of this
connection, just as they are normative among family
and friends in Puerto Rican culture. Although it is
difficult to demonstrate, it is also the case that this
clinical intimacy, as described by some of the doctors,
opens a space for greater healing potential for both
patient and physician.
References
- Astrow AB and Sulmasy DP (2004) Spirituality and the patientÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
âphysician relationship. JAMA 291:2884.
- Astrow AB, PulchalskiCMandSulmasy DP (2001) Religion, spirituality and health care: social, ethical and practical considerations. American Journal of Medicine 110:283ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â7.
- Bell D, Harbinson M, Toman G et al (2010) Wholeness of healing: an innovative student-selected component introducing United Kingdom medical students to the spiritual dimension in healthcare. Southern Medical Journal 103:1204ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â9.
- Bohart AC and Greenberg LS (1997) Empathy Reconsidered: new directions in psychotherapy. Washington, DC: American Psychological Association.
- Bragdon E (ed.) (2011) Spiritism and Mental Health: practices from Spiritistcenters and Spiritist psychiatric hospitals in Brazil. London: Singing Dragon Press.
- Comas-Diaz L (1981) Puerto Rican espiritismo and psychotherapy. American Journal of Orthopsychiatry 51:636ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â45.
- Cox J, Campbell AV and Fulford B (KWM) (2007) Medicine of the Person: faith, science and values in health care provision. London: Jessica Kingsley Publishers.
- Craigie FC and Hobbs RF (1999) Spiritual perspectives and practices of family physicians with an expressed interest in spirituality. Family Medicine 31:578ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â85.
- Curlin FA, Roach CJ, Godwara-Bhat R et al (2005) How are religion and spirituality related to health? A study of physiciansÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ perspectives. Southern Medical Journal 78: 761ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â6.
- Davis-Floyd R and St John G (1998) From Doctor to Healer: the transformative journey. New Brunswick, NJ: Rutgers University Press.
- Elliott R, Bohart AC, Watson JC et al (2011) Empathy. Psychotherapy 48:43ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â9.
- Holmes SL, Rabow ML and Dibble SL (2006) Screening the soul: communication regarding spiritual concerns among primary care physicians and seriously ill patients approaching the end of life. American Journal of Hospice and Palliative Care 23:25ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â33.
- Ironson G, Solomon GF, Balbin EG et al (2002) The IronsonÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
âWoods Spirituality/Religiousness Index is associated with long survival, health behaviors, less distress, and low cortisol in people with HIV/AIDS. Annals of Behavioral Medicine 24:34ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â48.
- Koenig HG (2007a) Medicine, Religion, and Health. West Conshohocken, PA: Templeton Foundation Press. Koenig HG (2007b) Spirituality in Patient Care: why, how, when, and what. West Conshohocken, PA: Templeton Foundation Press.
- Kohut H (1984) How Does Analysis Cure? Chicago: University of Chicago Press.
- Koss JD (1987) Expectations and outcomes for patients given mental health care or spiritist healing in Puerto Rico. American Journal of Psychiatry 144:56ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â61.
- Koss-Chioino JD (2006a) Spiritual transformation, ritual healing, and altruism. Zygon 41:877ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â92.
- Koss-Chioino JD (2006b) Spiritual transformation, relation and radical empathy: core components of the ritual healing process. Transcultural Psychiatry 43:652ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â70.
- Lex A (1985) AsoperacoÃÆÃââââ¬Ã¹ÃÆââ¬Å¡Ãâ¦Ã¢â¬Åesespirituais [Operations performed by spirits]. BoletimMeÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâôdico-EspiÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâôrita 3:141ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â52.
- MarinÃÆÃââââ¬Ã¹ÃÆââ¬Å¡Ãâ¦Ã¢â¬Åo M (1963) El Espiritismo en la Argentina [History of Spiritism in Argentina]. Buenos Aires, Argentina: Editorial Constancia.
- Martinez-Taboas A (2005) Psychogenic seizures in an espiritismo context: the role of culturally sensitive psychotherapy. Psychotherapy: Theory, Research, Practice, Training 42:6ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â13.
- Matos-Romero M (1983) HistoriadelEspiritismo en Venezuela [History of Spiritism in Venezuela]. Maracaibo, Venezuela: TipograiÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡ÃâôaUnioÃÆÃââââ¬Ã
¡ÃÆââ¬Å¡Ãâô n.
- Newton BW, Barber L, Clardy J et al (2008) Is there hardening of the heart during medical school? Academic Medicine 83:244ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â9.
- Novich Hernandez H (1999) Salud, Enfermedad y Muerte [Health, Illness and Death]. Caracas, Venezuela: Ediciones CIMA.
- OlsonMM,Sandor MK, Sierpina VS et al (2006) Mind, body and spirit: family physiciansÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢ beliefs, attitudes and practices regarding the integration of patient spirituality into medical care. Journal of Religion and Health 45:234ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â47.
- Paloutzian RF (2005) Religious conversion and spiritual transformation: a meaning-system analysis. In: Paloutzian RF and Park CL (eds) Handbook of the Psychology of Religion and Spirituality. New York: Guilford. pp. 331ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â47.
- Pargament KI, Mahoney A, Exline JJ et al (2013) Envisioning an integrative paradigm for the psychology of religion and spirituality. In:
- Pargament KI, Exline J and Jones J (eds) APA Handbook of Psychology, Religion, and Spirituality. Volume 1. Context, theory, and research. Washington, DC: American Psychological Association. pp. 3ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â20.
- Pedersen R (2010) Empathy development in medical education: a critical review. Medical Teacher 32:593ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â600.
- Puchalski CM (2006) A Time for Listening and Caring. New York: Oxford University Press. pp. 149ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â53.
- Roberto G (2011) When medical doctors are mediums. In: Bragdon E (ed.) Spiritism and Mental Health: practices from Spiritistcenters and Spiritist psychiatric hospitals in Brazil. London: Singing Dragon Press.
- Rogers CR (1957) The necessary and sufficient conditions of therapeutic personality change. Journal of Consulting and Clinical Psychology 21:95ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â103.
- Rogers CR (1959) A theory of therapy, personality and interpersonal relationships, as developed in the clientcentered framework. In: Koch S (ed.) Psychology: a study of a science. New York: McGraw Hill. pp. 184ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â256.
- Sulmasy DP (2006) The healthcare professional as person: the spirituality of providing care at the end of life. In: Puchalski C (ed.) A Time for Listening and Caring. New York: Oxford University Press. pp. 101ÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Ã
â14.