Douaguibe Baguilane1*, Bassowa Akila1, Ketevi Ayoko Tina1, Baramna B1, Fiagnon Kodjo1, Akpadza Koffi1, Aboubakari Abdoul-Samadou2 and Ajavon Dede2
1Department of Gynecology and Obstetrics, CHU Sylvanus Olympio (CHU-SO), Lome, Togo
2Department of Gynecology and Obstetrics, CHU Kara, Kara, Togo
*Corresponding Author:
Douaguibe Baguilane
Department of Gynecology and Obstetrics
CHU Sylvanus Olympio (CHU-SO)
Lome, Togo
Tel: (00228)90328262
E-mail: douaguibe@hotmail.com
Received Date: January 14, 2019; Accepted Date: February 07, 2019; Published Date: February 10, 2019
Citation: Baguilane D, Akila B, Tina KA, Baramna B, Kodjo F, et al. (2019) Report of Three Cases of Osteoid Metaplasia of the Endometer at the Campus Teaching Hospital in Lome. Gynecol Obstet Case Rep Vol.5: No.1: 70. doi: 10.21767/2471-8165.1000070
Keywords
Osteoid metaplasia; Hysteroscopy; Lome
Introduction
Endometrial Osteoid Metaplasia (EOM) is a rare case characterized by the presence of bone tissue in the endometrium [1,2]. It is a pathology poorly known, insufficiently researched and consequently little diagnosed and poorly treated. It is often diagnosed when exploring a female secondary infertility.
The main objective of this work is to report three cases of EOM and hysteroscopy surgery treatment at the gynecology-obstetrics clinic of the Lome campus University Hospital between 2015 and 2017.
Case Report
Observation 1
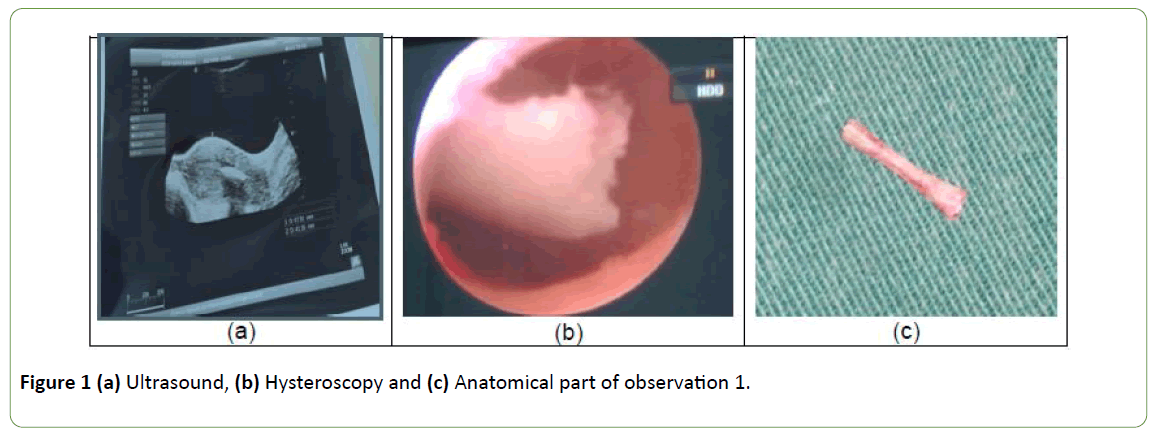
The first case concerns a 30-year-old nulliparous primigest woman who had consulted for secondary infertility in 2015. She had a history of late voluntary abortions ending with curettage. She did not complain of any other sign. The gynecological examination was normal.
Diagnostic: The transvaginal ultrasound performed as part of the infertility assessment had objectified a highly echogenic persistent, and linear in uterus cavity picture with a posterior shadow cone. It looked as an intrauterine device, but she denied any experience of having a procedure of intrauterine device insertion (Figure 1a).
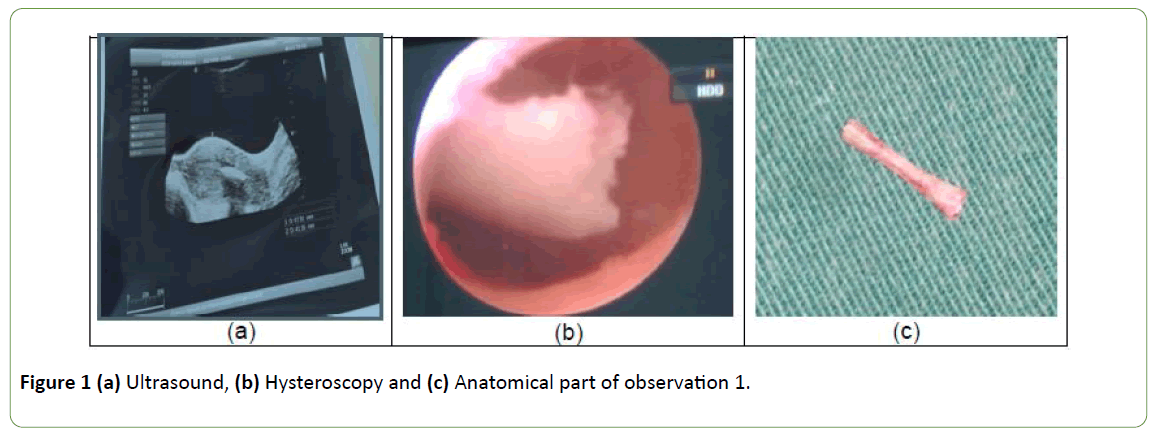
Figure 1: (a) Ultrasound, (b) Hysteroscopy and (c) Anatomical part of observation 1.
Diagnostic and surgical hysteroscopy was performed under spinal block anesthesia. We had visualized a wide endometrial cavity with linear structure seemed bone, about 1.5 cm in length, on the anterior wall of the uterus (Figure 1b). The lesion was completely removed using the grasping forceps under hysteroscopic control. There were no operative complications (Figure 1c).
Evolution: She started a spontaneous pregnancy in 2016 after treatment; this pregnancy ended in spontaneous miscarriage at 13SA. She then conceived spontaneously in 2017 and carried this pregnancy to its term with a baby boy born vaginally.
Observation 2
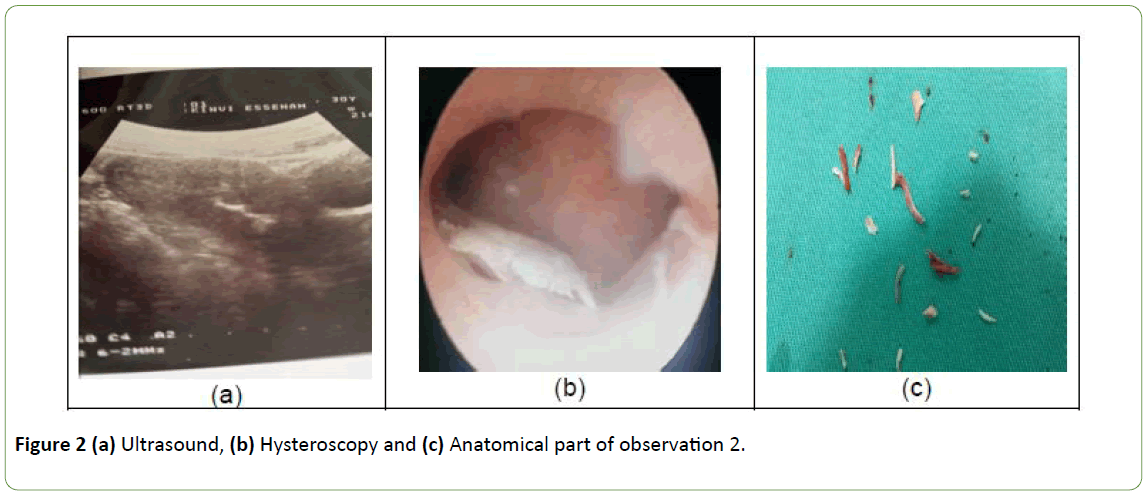
The second case registered is about a 26-year-old nulliparous primigest woman who had consulted for a secondary infertility in 2016. She also had a history of voluntary abortion by curettage. She did not complain of any other sign. The gynecological examination was normal.
Diagnostic: The transvaginal ultrasound performed as part of the infertility assessment had objectified a highly echogenic, persistent and linear image in uterus cavity with a posterior shadow cone.
It looked as an intrauterine device, but she denied any experience of having a procedure of intrauterine device insertion (Figure 2a).
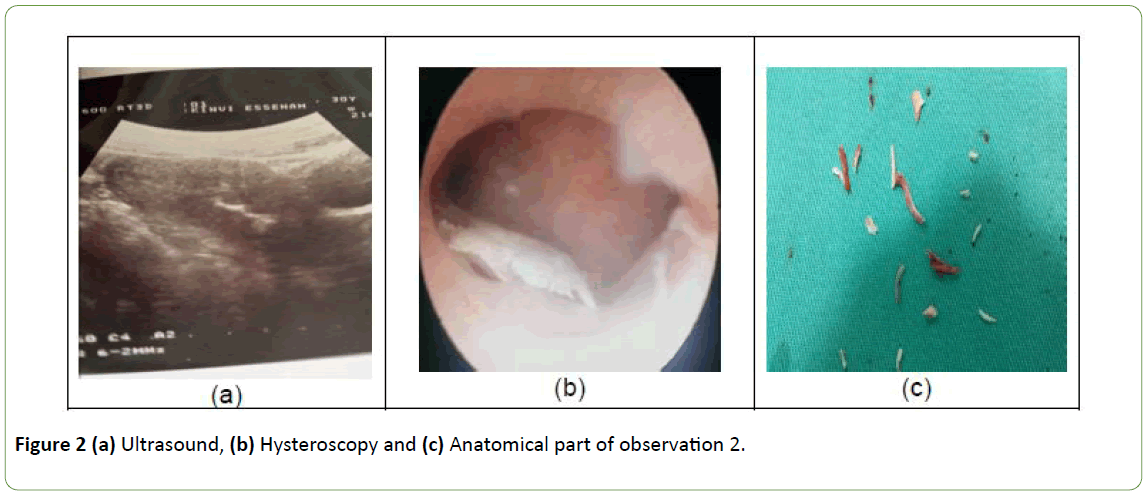
Figure 2: (a) Ultrasound, (b) Hysteroscopy and (c) Anatomical part of observation 2.
Diagnostic and surgical hysteroscopy was performed under spinal block anesthesia. Diagnostic hysteroscopy revealed of heap bone structure near to the isthmus measuring 1 cm length, extending to the lateral posterior uterine wall (Figure 2b). The endometrium mucosa appeared to be inflammated. No other lesions were seen.
Surgical hysteroscopy removed the heap of bone fragment by using mainly resectoscope mechanically without electrosurgical energy (Figure 2c).
Evolution: She was nowhere to be found after a first clinical checkup that was normal.
Observation 3
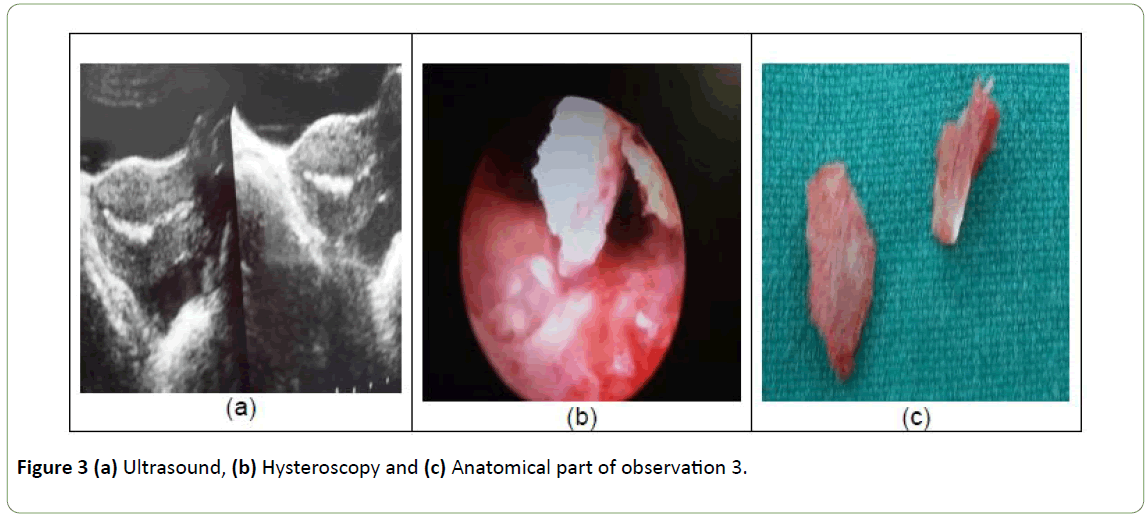
The third patient, aged 32, was examined in January 2017 for pelvic pain and menorrhagia. Three months before she had an abortion at 24SA. An intrauterine manual aspiration was carried out for retention of placental debris. Vaginal speculum examination revealed a bleeding of endo-uterine origin of minimal abundance and normal appearance of the exocervix and vaginal walls.
Diagnostic: The transvaginal ultrasound performed as part of the pain and bleeding assessment had objectified a highly echogenic persistent, and linear in uterus cavity picture with a posterior shadow cone. It looked as an intrauterine device, but she denied any experience of having a procedure of intrauterine device insertion (Figure 3a).
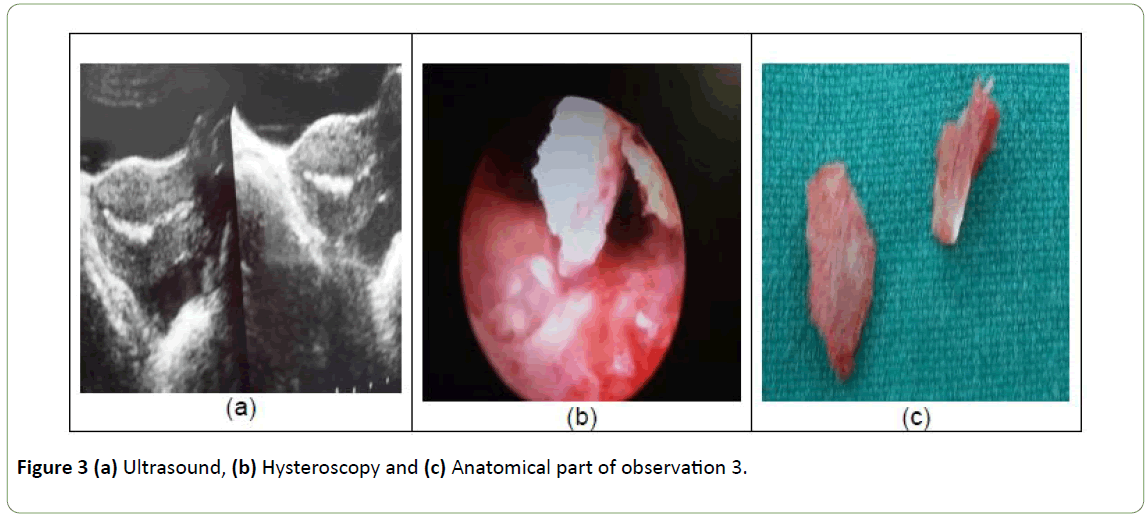
Figure 3: (a) Ultrasound, (b) Hysteroscopy and (c) Anatomical part of observation 3.
Diagnostic and surgical hysteroscopy was performed under spinal block anesthesia.
We had visualized a proliferative endometrium with linear structure picture like bone, about 1.5 cm in length, on the anterior wall of the uterus (Figure 3b). The lesion was completely removed using the grasping forceps under hysteroscopic control. There were no operative complications (Figure 3c).
Evolution: The month following hysteroscopy, there was a cessation of the menometrorrhagia and pelvic pain.
In each of the three cases, the fragments collected were sent in anatomopathology. The results were identical in all three cases: an EOM.
Discussion
The EOM is a rare pathology whose frequency is estimated at 0.3 per 1000 infertile women [1,3]. These series is the first reported in our training, and in Togo. Indeed a predisposition to this pathology of African women has been mentioned in the literature [3,4]. This fact may be related to the possible confusion of these lesions with the uterine synechiae but also that we do not think at all about this pathology. Indeed its symptomatology is variable and not specific. Often asymptomatic, it is discovered haphazardly during the exploration of a secondary infertility as in the two cases of patients described here. Sometimes, these are the signs common to other gynecological pathologies: pelvic pain, genital bleeding, vaginal discharge etc. as it is the case of third patient. According to the literature consulted, the EOM is diagnosed in the context of a history of abortion, especially late abortion, with instrumental endo-uterine maneuver [3]. The patients described here had late abortions with endo-uterine maneuvers. The period between the abortion and the diagnosis of EOM is highly variable, lasting up to several years [1]. Metaplasia would behave as an IUD and this explains it is more frequently found in patients treated for a secondary infertility [5]. The pathophysiology of this entity is still unclear [6,7]. Several hypotheses have been put forward, namely an in utero retention of fetal bone fragments, a spontaneous endometrial graft or a curettage of mesenchymal fetal cells with bone potential, an embryonic Mullerian origin and most commonly, the theory accepted, is that of the replacement of the chorion as a result of curettage or endometritis by scar tissue of maternal origin which would then see its mesenchymal cells transformed [8,9].
The ultrasound pictures described in this series are identical to those described in the literature: hyperechoic image with a posterior shadow cone, blurring contours, often linear in appearance, intra-cavitary and persistent throughout the cycle [10]. However, this aspect may be confusing with other etiologies such as uterine synechiae, calcified endometrial polyp, genital tuberculosis, post-cesarean stellate scar or post myomectomy, or a typical copper-bearing IUD. One must know how to think about it in front of ultrasound images and indicate a diagnostic and hysteroscopy surgery. Hysteroscopy is the golden standard for diagnosis and treatment [11]. The pictures described in hysteroscopy in our series are similar to pictures described by other authors. Removal of all fragments is essential to achieve uterine emptiness, to treat the symptoms and to have a pregnancy in some cases of infertility [12] as in one of the patients who conceived spontaneously twice after the hysteroscopy surgery. The pathological study had made it possible to diagnose and exclude other endometrial pathologies which management differs from that of the EOM. Curettage is not indicated because it does not allow a complete treatment and it is very traumatic for the endometrium and, finally and more frequently, it gives uterine synechiae. Clinical and ultrasound monitoring or even hysteroscopy is essential to detect recurrences and see its effectiveness after treatment.
In practice, in front of endocavity linear anomaly at the ultrasound, the diagnostic hysteroscopy must be done. in our areas with lack of materials. The grasp forceps can be used for removal the fragments of bone.
Conclusion
This study showed that osteoid metaplasia of the endometrium exists in Togo. All the patients had abortion history voluntary or not. The transvaginal ultrasound and Hysteroscopy were used for diagnostic and the treatment. Pathological examination allows a histological diagnosis. We got good results with surgical hysteroscopy.
References
- Benchimol M, Seince N, Tigazin A, Carbillon L, Uzan M (2003) Osteoid metaplasia of the endometrium: About a case. Gynecol Obstet Fertil 31: 841-843.
- Kouakou F, Loue V, Kouame A, Adjoby R, Koui S, et al. (2012) Endometrial osseous metaplasia and infertility: A case report. Clin Exp Obstet Gynecol 39: 559-561.
- Creux H, Hugues JN, Sifer C, Cedrin-Durnerin I, Poncelet C (2010) Fertility after elective hysteroscopic resection of osteoid metaplasia lesions of the endometrium. Gynecol Obstet Fertil 38: 460-464.
- Graham O, Cheng LC, Parsons JH (2000) The ultrasound diagnosis of retained fetal bones in West African patients complaining of infertility. BJOG 107: 122-124.
- Jilly L, Samuel M (2012) Severe endometrial ossification with subsequent conception and placenta accreta: a case report. Am J Obstet Gynecol 207: e7-e8.
- Singh P, Kapur K, Singla S, Naz N (2011) Endometrial osseous metaplasia and mature bone formation with extramedullary hematopoiesis. J Hum Reprod Sci 4: 56-57.
- Umashankar T, Patted S, Handigund R (2010) Endometrial osseous metaplasia: Clinicopathological study of a case and literature review. J Hum Reprod Sci 3: 102-104.
- Van den Bosch T, Dubin M, Cornelis A (2000) Favorable pregnancy outcome in a woman with osseous metaplasia of the uterus. Ultrasound Obstet Gynecol 15: 445-446.
- Moon HS, Park YH, Kwon HY, Hong SH, Kim SK (1997) Iatrogenic secondary infertility caused by residual intrauterine fetal bone after midtrimester abortion. Am J Obstet Gynecol 176: 369-370.
- Madaan M, Suman S, Sharma R, Kapoor N, Garg P, et al. (2015) Osseous metaplasia of the endometrium and successful hysteroscopic resection: A report of two cases and a review of the literature. Asian J Endosc Surg 8: 63-66.
- Pace S, Torcia F, Palazzetti PL, Piazze JJ, Cipriano L, et al. (2001) Successful diagnostic and surgical hysteroscopy for endometrial ossification. Clin Exp Obstet Gynecol 28: 24-25.
- Adamson NE, Sommers SC (1954) Endometrial ossification; Report of two cases. Am J Obstet Gynecol 67: 187-190.