- (2004) Volume 5, Issue 4
Luc G Morris1, Kathryn E Stephenson2, Sharon Herring2, Jennifer L Marti1
1Department of Surgery and 2Department of Medicine, New York University School of Medicine. New York, NY, USA
Received: 21 April 2004 Accepted: 19 May 2004
Context :Mild pancreatitis has been reported as a consequence of anorexia nervosa, bulimia nervosa, or what has been termed the “dietary chaos syndrome”. Either chronic malnutrition, or refeeding after periods of malnutrition, may precipitate acute pancreatitis through several pathogenetic mechanisms. Case report :A 26-year-old woman with a ten-year history of anorexia and bulimia presented with a third episode of acute pancreatitis in three months. The patient had been abstinent from alcohol for many years. Imaging studies during all three admissions failed to identify any biliary disease, including gallstones or biliary sludge. A cholecystectomy was performed, with a normal intraoperative cholangiogram, and no abnormalities on pathologic examination of the gallbladder and bile. The patient was discharged on hospital day 10 with no pain, and she has begun to return to regular eating habits. Pancreatitis has not recurred after 6 months of follow up. We have identified 14 cases in the literature of acute pancreatitis associated with anorexia or bulimia. Conclusion :In the absence of evidence for gallstone, alcohol or metabolic etiologies, eating disorders may contribute to the pathophysiology of some idiopathic cases of pancreatitis.
Anorexia; Anorexia Nervosa; Bulimia; Eating Disorders; Pancreatitis
In 20-30% of cases of recurrent pancreatitis, no direct cause can be identified, resulting in a diagnosis of idiopathic pancreatitis. A significant percentage of these cases are believed to actually result from occult disease: either microlithiasis or biliary sludge [1].
Nevertheless, as many as one quarter of idiopathic pancreatitis cases will have no evidence of sludge or microcrystals on pathologic examination [2], and such cases may remain truly idiopathic. We report one such case in a patient with anorexia and bulimia, eating disorders that may precipitate acute pancreatitis.
A 26-year-old Caucasian woman with a tenyear history of anorexia nervosa and bulimia nervosa presented with four days of progressively increasing epigastric pain, nausea and vomiting.
The patient had been in her usual state of health until three months prior to the current admission, when she presented to the hospital with epigastric pain, nausea and vomiting, and was found to have acute pancreatitis. At that time, imaging studies of the hepatobiliary tree were normal and without evidence for gallstones or bile duct abnormalities. The pancreatitis resolved with supportive care. One month prior to admission, she presented again with acute pancreatitis and was admitted for supportive care. Imaging studies were again unrevealing, and the patient was discharged upon resolution of disease.
Four days prior to admission, the patient again developed epigastric pain, nausea and vomiting, which progressed in severity until the patient sought medical attention. At that time, she was admitted for supportive care and given i.v. fluids, hydromorphone analgesia, and nothing by mouth. The patient described her daily intake over the past several years as less than 200 calories although she did admit to frequent episodes of binge eating. She denied any alcohol intake in many years. She also denied changes in her weight over the past several years.
Other than anorexia and bulimia, for which the patient has been under the care of a psychiatrist for many years, the patient denied any other past medical or surgical history. She has taken sertraline 50 mg daily for more than five years, and denied allergies to medications or any family history of significance. She denied alcohol, tobacco or illicit drug use. On admission, the patient weighed 52 kg and was 158 cm in height. Vital signs were stable. Physical examination revealed only mild parotid gland enlargement bilaterally and moderate to severe epigastric tenderness without peritoneal signs.
Admission serum amylase was 50 IU/L (reference range: 53-123 IU/L) and lipase was 399 IU/L (reference range: 10-150 IU/L). Hepatic function tests were significant for an alkaline phosphatase of 157 IU/L (reference range: 50-160 IU/L) and albumin of 2.5 g/dL (reference range: 3.5-5.0 g/dL). Serum calcium, triglyceride and lipid levels were all within reference ranges. Abdominal CT revealed acute pancreatitis but was unable to rule out biliary disease. Follow-up magnetic resonance cholangio-pancreatography (MRCP) failed to identify gallstones or bile duct dilatation. Transabdominal ultrasound identified no stones or sludge in the gallbladder or biliary tree.
On hospital day 3, serum amylase increased to 64 IU/L and serum lipase increased to 944 IU/L. These values began to decline on hospital day 5. On hospital day 8, the patient underwent laparoscopic cholecystectomy. The intraoperative cholangiogram was read as normal. Surgical pathology revealed no acute pathology of the gallbladder, including sludge or microcrystals. The patient was discharged on hospital day 10 with no pain.
Since discharge, the patient has been motivated by her hospital admissions to attempt to return her diet to regularity, with the assistance of her psychiatrist. She has increased her daily caloric intake and has avoided any bingeing episodes. Pancreatitis has not recurred after 6 months of follow up.
Idiopathic recurrent pancreatitis is a difficult but unfortunately not uncommon diagnostic problem: approximately 20-30% of cases of recurrent acute pancreatitis are given the idiopathic diagnosis after thorough clinical investigation [1]. Venu et al. [3], in a series of 116 cases of idiopathic recurrent pancreatitis, performed endoscopic retrograde cholangiopancreatography and sphincter of Oddi manometry in an effort to better define the nature of pathology in these mysterious cases. Even with this additional intervention, 62% of cases in this study remained “truly” idiopathic, in that there were no gross anatomic or functional abnormalities of the pancreas.
In this case, there was no evidence of gallstone, alcohol, or metabolic etiologies for the patient’s recurrent pancreatitis. Pathologic examination of the gallbladder revealed no evidence of inflammation, stones, sludge, or microcrystals.
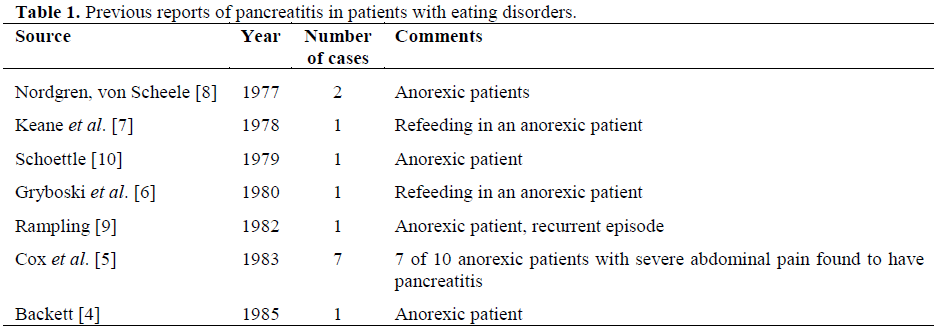
We have identified 14 cases in the literature of pancreatitis in the setting of anorexia nervosa [4, 5, 6, 7, 8, 9, 10] (Table 1). Severe malnutrition is known to be associated with pancreatic injury, through a number of pathogenetic mechanisms. At the cellular level, pancreatitis is believed to ultimately depend on activation of trypsinogen to trypsin within the pancreas, leading to the subsequent activation of other proteases. Together, these enzymes cause cell damage and trigger further inflammatory processes.
Chronic malnutrition has been demonstrated to eventuate in a number of processes within the pancreas. Sandhyamani et al. identified marked acinar cell atrophy, islet cell hyperplasia, and mucoid metaplasia in malnourished monkeys [11]. Other investigators have also identified acinar cell atrophy, epithelial metaplasia, and increased zymogen granule release in malnourished patients [12, 13]. Even in the absence of frank pancreatitis, high trypsinogen levels may be found in malnourished patients, reflecting either acinar cell injury or obstruction of pancreatic ducts [14].
Keane et al. have suggested that both rapid weight loss and refeeding after starvation episodes can cause visceroptosis (gastrointestinal ileus and dilatation), leading to retrograde pressure or reflux of duodenal contents into the pancreatic duct [7]. Retrograde pressure may also prevent pancreatic enzymes from leaving the pancreatic duct.
Nevertheless, the proposed pathogenesis of pancreatitis in eating disorders is largely speculative. Indeed, occult microlithiasis not visible on radiologic imaging has been suggested as a cause for many cases of “idiopathic” pancreatitis [2, 15, 16, 17]. Pathologic examination of this patient’s gallbladder and bile was negative for sludge or microcrystals. Although surgery was not performed until hospital day 8, resolution of biliary sludge or microlithiasis is usually on the order of months to years [18]. While the patient has been free of recurrence since cholecystectomy, it is unclear whether this is a result of surgical cure of occult biliary disease, or whether it is simply a result of her return to regular eating habits. However, even if eating disorders were not the sole cause of recurrent pancreatitis in this patient, it is likely that anorexic or bulimic pancreatic pathology made the patient more susceptible to otherwise insignificant biliary disease. Although there are two reported cases of acute pancreatitis in patients taking sertraline [19], this patient had been on sertraline without incident for many years. Furthermore, a comprehensive review of the World Health Organization adverse event database by Spigset et al. [20] concluded that sertraline and other selective serotonin reuptake inhibitors (SSRIs) are not associated with pancreatitis, although tricyclic antidepressants may be. We therefore considered sertraline an unlikely contributor to this patient’s disease. This case report suggests that combined modality treatment targeted at both occult biliary disease, as well as eating disorders, may be successful in treating idiopathic recurrent pancreatitis in patients with anorexia or bulimia.
This case report illustrates the contribution of eating disorders such as anorexia and bulimia to pancreatitis. Although a rare finding, the association has been reported and a likely pathogenetic mechanism has been suggested. Eating disorders may derange normal pancreatic physiology, and may precipitate acute pancreatitis alone, or in combination with other etiologic factors. This association should be kept in mind when the clinician is faced with idiopathic cases of pancreatitis, or with anorexia nervosa patients who complain of abdominal pain.