- (2005) Volume 6, Issue 4
M Mahir Ozmen, Munevver Moran, Murat Karakahya, Faruk Coskun
Department of Surgery, Ankara Numune Teaching and Research Hospital, Ankara, Turkey
Received May 10th, 2005 - Accepted May 24th, 2005
Context Primary pancreatic hydatid disease is rare and there have only been a few cases of recurrent acute pancreatitis due to a hydatid cyst of the pancreas. Case report We describe a case of recurrent acute pancreatitis in which the definitive diagnosis of hydatid cyst of the pancreatic head was only made during a repeat operation and the patient subsequently underwent total pericystectomy. Conclusion A hydatid cyst of the pancreas is an extremely rare condition but it may be a causative factor for recurrent acute pancreatitis, especially in endemic areas. In this case, pericystectomy might be the procedure of choice in order to release the pressure.
Echinococcosis; Pancreas; Pancreatitis
CBD: common bile duct
Hydatid disease is endemic in many countries, including those around the Mediterranean, Central Asia, the Far East and Latin America. The liver is the most commonly affected organ, followed by the lungs. Cysts are rarely found in the pancreas. The incidence of primary hydatid disease of the pancreas is less than 1% [1, 2, 3, 4, 5].
Acute pancreatitis has been identified as an acute inflammatory process of the pancreas, with variable involvement of other regional tissues or remote organ systems [6]. In 90% of cases, the cause is related to alcohol intake or biliary tract disease but acute pancreatitis may also occur after pancreatic duct obstruction [7]. Acute pancreatitis due to hydatid cysts is extremely rare; as far as we know, there are only three cases in the literature but no case in the English medical literature [8, 9, 10]. We report the rare case of recurrent acute pancreatitis caused by extrinsic compression of the pancreatic duct owing to a primary hydatid cyst in the head of the pancreas.
An 18-year-old female patient was admitted to the Emergency Surgery Department of the Ankara Numune Teaching and Research Hospital in Turkey with a persistent, severe epigastric pain radiating to the back, nausea and vomiting for two days. Her history revealed that she had had an attack of acute pancreatitis which was resolved medically and she had undergone a cystogastrostomy for a pancreatic pseudocyst six years previously. She had no previous history of jaundice, trauma or drug intake and had no known disease.
Physical examination revealed a pulse rate of 105 min-1, blood pressure of 120/95 mmHg and a body temperature of 38.5 °C. On abdominal examination, she had peritoneal irritation signs such as severe epigastric tenderness and rebound tenderness in all abdominal quadrants and mild abdominal distention. Her hemoglobin level was 14.1 g/dL (reference range: 12.3-15.3 g/dL), white blood cell count was 22.8 x109/L (reference range: 4.4-11.3 x109/L), serum total bilirubin was 1.26 mg/dL (reference range: 0.2-1.2 mg/dL), serum aspartate aminotransferase (AST) was 55 U/L (reference range: 0-40 U/L), serum alanine aminotransferase (ALT) was 17 U/L (reference range: 0-50 U/L), serum amylase level was 1,739 U/L (reference range: 25-125 U/L) and total serum calcium was 7.5 mg/dL (reference range: 8.4- 10.6 mg/dL). There were no pathological findings on plain abdominal X-ray and left pleural effusion was seen on chest X-ray. Abdominal ultrasound revealed a multilocular anechoic cystic lesion of 43x35 mm in size located in the head of the pancreas which was compressing the pancreas - with the possible diagnosis of pancreatic pseudocyst or abscess - causing pancreatic edema and heterogeneity at the body and tail of the pancreas along with perihepatic, perisplenic and pelvic free fluid collections (Figure 1). The Ranson score on admission was one (high white blood cell count) and 48 hours later, it was again one (low serum calcium).
The patient underwent surgery with the diagnosis of acute abdomen due to necrotizing pancreatitis and the suspicion of complicated cyst-abscess of the pancreas. At laparotomy, approximately 1,000 mL of reactional intraperitoneal fluid were aspirated and exploration revealed pancreatic edema and necrosis located especially on the body and the tail of the pancreas together with perisplenic, omenthal and mesocolonic fat necrosis. There was also a 4x4 cm welldefined, tense cystic lesion just behind the head of the pancreas (Figures 2 and 3). The pancreatic head and tail were mobilized and necrosectomy was performed as required; cholecystectomy and common bile duct (CBD) exploration were performed and the CBD was decompressed with a T tube due to the suspicion of a palpable stone in the CBD (but exploration did not reveal any stone). Drains were inserted and the abdomen was left open using the Bogota bag technique in order to decrease abdominal tension and perform continuous abdominal lavage.
On the third postoperative day, the patient was taken into the operating room for exploration and debridement by senior surgeons. Exploration revealed the suspicion of a hydatid cyst of the pancreas located at the back of the pancreatic head causing necrotizing pancreatitis. In order to confirm the diagnosis, a small window was opened on the cystic wall and several hydatid daughter vesicles were seen and scolicidal solution (3% NaCl) was injected into the cystic cavity to prevent possible peritoneal contamination after the aspiration of the clear cystic fluid (Figure 4). The entire endocyst, comprising both the inner germinal and outer chitinous layers, was totally extracted from the ectocyst of the surrounding pancreatic parenchyma (Figure 5). No connection was found with the pancreatic duct. All devitalized tissues on the body and tail of the pancreas were debrided; drains were placed for continuous postoperative lavage of the abdominal cavity and a Bogota bag was inserted for planned relaparotomies [11].
Histological examination of the cyst wall, vesicles and degenerated material confirmed the diagnosis of hydatid disease and necrotizing pancreatitis.
The patient underwent ten more relaparotomies and debridements for necrotizing tissue and also had a splenectomy due to uncontrolled major abdominal bleeding from the splenic artery. She was discharged sixty-eight days after the first operation. She was given albendazole 50 mg/kg starting 7 days after surgery while she was in the hospital. Albendazole therapy was continued postoperatively for three sessions, each lasting four weeks separated by 14 day intervals [12].
host for Echinococcus and harbor the tapeworm in the small intestine. Sheep and cattle are the intermediate hosts and become infected by eggs of infected dogs shed into the environment with their feces. A grazing animal swallows the ova, which become hexacanth embryos and enter the portal circulation and are then carried to the liver, lungs and other organs leading to the formation of cysts. Humans swallow the ova after handling infected dogs or vegetation. Both grazing animals and humans are intermediate hosts in which the cystic form of the parasite develops. The life cycle is completed when dogs eat the cyst-bearing organ of the intermediate hosts.
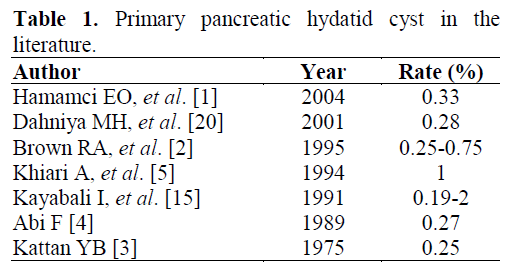
A hydatid cyst may develop in almost any organ of the body and is most commonly located in the liver. Pancreatic involvement occurs in less than 1% of the cases [1, 2, 3, 4 5]. Possible sources of infestation include hematogenous dissemination, local spread via pancreatobiliary ducts, and peripancreatic lymphatic invasion [2]. Clinical presentation is the result of pressure generated by the cyst on adjacent structures, and depends heavily on the size and anatomic location of the cyst. The cyst is localized in the head of the pancreas in 50% of cases [14, 15]. Patients may present with jaundice if the cyst is located in the head of the pancreas [1, 16, 17]. Rates of pancreatic localization differ in the literature (Table 1).
Acute pancreatitis is a non-bacterial inflammation of the pancreas caused by the activation, interstitial liberation, and digestion of the gland by its own enzymes. There may just be a single episode of pancreatitis, or several episodes may reoccur. Eighty per cent of patients will have a mild attack of pancreatitis in which the mortality rate is about 1%, while in those who have a severe attack of pancreatitis, the mortality rate ranges from 20 to 50%. The major causes of acute pancreatitis are biliary calculi which occur in 50-70% of patients and alcohol which occurs in 25% of the patients. The remaining cases may be due to rare or idiopathic causes [7, 18].
Partial duct obstruction, along with the stimulation of pancreatic secretion, produces a more severe pancreatic inflammation. Duct obstruction of brief duration may cause acute pancreatitis; when it is persistent over months or years, it is a recognized cause of chronic pancreatitis. Though a hydatid cyst of the pancreas is very rare, recurrent acute pancreatitis caused by compression of the pancreatic duct from a hydatid cyst located in the head of the pancreas is even rarer; there were only three acute pancreatitis cases in the literature but no case was found in the English medical literature [8, 9, 10].
Although cystic lesions of the pancreas may easily be identified by US and CT, the diagnosis of a hydatid cyst of the pancreas is extremely difficult and can rarely be established preoperatively unless hydatid disease is suspected [9, 10]. The cyst may easily be confused with a pseudocyst of the pancreas. In the present case, ultrasound was failed to diagnose the hydatid cyst of the pancreas but it revealed the signs of acute pancreatitis and a complicated pseudocyst.
The current definitive treatment of hydatid disease of the pancreas is surgical removal of the cysts when their location permits; however, percutaneous drainage of the cyst using hypertonic (20%) saline lavage has been used successfully in the management of a pancreatic hydatid cyst in one series [17]. At the head of the pancreas, the cyst contents should be removed and a scolicidal agent (hypertonic saline, silver nitrate, cetrimide) should be injected into the cyst. The reason for the complete removal of the chitinous endocyst with all daughter cysts as we did in our case is to prevent further episodes of pancreatitis,. In addition to this procedure, the biliary tree was drained and the necrotic pancreatic tissue was debrided; in our case, drains were inserted for continuous abdominal lavage due to necrotizing pancreatitis. The misdiagnosis of the hydatid cyst at the first operation might be attributed to the inadequate experience of the surgeons on duty.
In conclusion, a hydatid cyst of the pancreas is an extremely rare condition but it may be a causative factor for recurrent acute pancreatitis, especially in endemic areas. Although radiological examinations may help clinicians in diagnosing cystic masses in the pancreas, certain diagnosis and treatment are best established during laparotomy. If the cyst is not related to the pancreatic duct, pericystectomy might be the procedure of choice in order to release the pressure. If there is a connection with the duct, a stent should also be inserted into the duct during surgery or cystogastrostomy might be the procedure of choice [19].