Research Article - (2020) Volume 28, Issue 4
Dusty Marie Narducci*
College of Medicine Family Medicine, University of South Florida, USA
Corresponding Author:
Dusty Marie Narducci
College of Medicine Family Medicine University of South Florida, USA
Tel: 3462474753
E-mail: dustynarducci@usf.edu
Received Date: April 16, 2020; Accepted Date: June 03, 2020; Published Date: June 11, 2020
Objective: Determine the number of athletes with electronic medical record (EMR) documentation of penicillin (PCN) allergy and enroll them into a PCN relabeling program using EMR risk stratification (EMR-RS) or team physician risk stratification (TP-RS) to determine the presence of true allergy.
Design: Retrospective data analysis, prospective cohort study.
Setting: Division 1 University Athletic Program.
Patients: Athletes with an EMR document PCN allergy (27 of 415).
Interventions: Athletes labeled as allergic to PCN were enrolled into a PCN relabeling program and appropriately categorized using EMR-RS and TP-RS. Athletes who were determined appropriate were offered recommendations for potential relabeling of their PCN allergy.
Outcome Measures: This QI study sought to establish the prevalence of true PCN allergy among athletes. Both EMRRS and TP-RS relabeling strategies were used to determine which method would more accurately identify true PCN allergy.
Results: From the 6.5% of athletes identified with as allergic to PCN, TP-RS was able to identify 92.59% of athletes to be falsely labeled as allergic to PCN, compared to 40.7% identified by EMR-RS a difference of 51.89%.
Conclusions: TP-RS is superior to EMR-RS for identifying falsely documented PCN allergies in athletes. TP-RS should be used to re-label athletes to decrease the use of unnecessary antibiotics, decrease healthcare costs, limit adverse events associated with antibiotic use, and prevent antimicrobial resistance in the athletic population.
Quality improvement, Collegiate, Athletes, Penicillin, Allergy, Re-labeling.
Approximately 10% (32 million) of US residents have been labeled as allergic to PCN. Current evidence suggests that as few as 10% (1% of US residents) who report a PCN allergy have a true allergy. No studies have been done regarding the presence of documented PCN allergies exclusively in athletes. Inaccurate EMR documentation of PCN allergy can lead to unnecessary use of broad-spectrum antibiotics, healthcare costs, increased adverse events, longer hospital stays, and antimicrobial resistance [1]. To promote quality improvement in the collegiate athlete population, team physicians should consider using risk stratification to assist in determining which athletes should be considered for re-labeling. This study sought to compare the number collegiate athletes with electronic medical record (EMR) documentation of penicillin (PCN) allergy to the number of US residents. PCN allergic athletes were enrolled into a PCN relabeling program to determine the presence of a true allergy, using electronic medical record risk stratification (EMR-RS) and team physician risk stratification risk stratification (TP-RS).
Study Design
Retrospective data analysis, prospective cohort study.
Hypothesizes
We hypothesize that EMR documented PCN allergy will be seen at a higher rate in collegiate athletes compared to the general US population. Additionally we hypothesize that following EMRRS or TP-RS of PCN allergy reactions less than 10% of athletes with a PCN allergy will have true allergy to PCN. We expect TP-RS to more accurately identify athletes with true PCN allergies compared to EMR-RS.
Methods
Electronic medical records of Division 1, male and female collegiate athletes aged 18-years or older at our institution were reviewed to determine documentation of PCN allergy. The data was extrapolated at one interval which included the end of 2019 Fall semester. This data analysis derived the following information: gender, age, allergy listed (including: Penicillin, Amoxicillin, Ampicillin, Ampicillin-sulbactam, and Amoxicillin Clavulanic Acid) and type of allergic reaction.
Using the American Medical Association (AMA) Penicillin Allergy History Tool Kit Page A1 (Figure 1). Athletes with an EMR documented PCN allergy were risk stratified into one of the following categories: high, moderate, low, indeterminate risk or intolerant to PCN. The athletes than met with the team physician who reviewed and recorded their PCN allergy history using the AMA Penicillin Allergy History Tool Kit Page A1/2 (Figures 1 and 2). The team physician used PCN allergy history to risk stratify athletes into the following categories: high, moderate, low, indeterminate risk or intolerant to PCN.

Figure 1: American Medical Association (AMA) penicillin allergy history tool kit page A1.
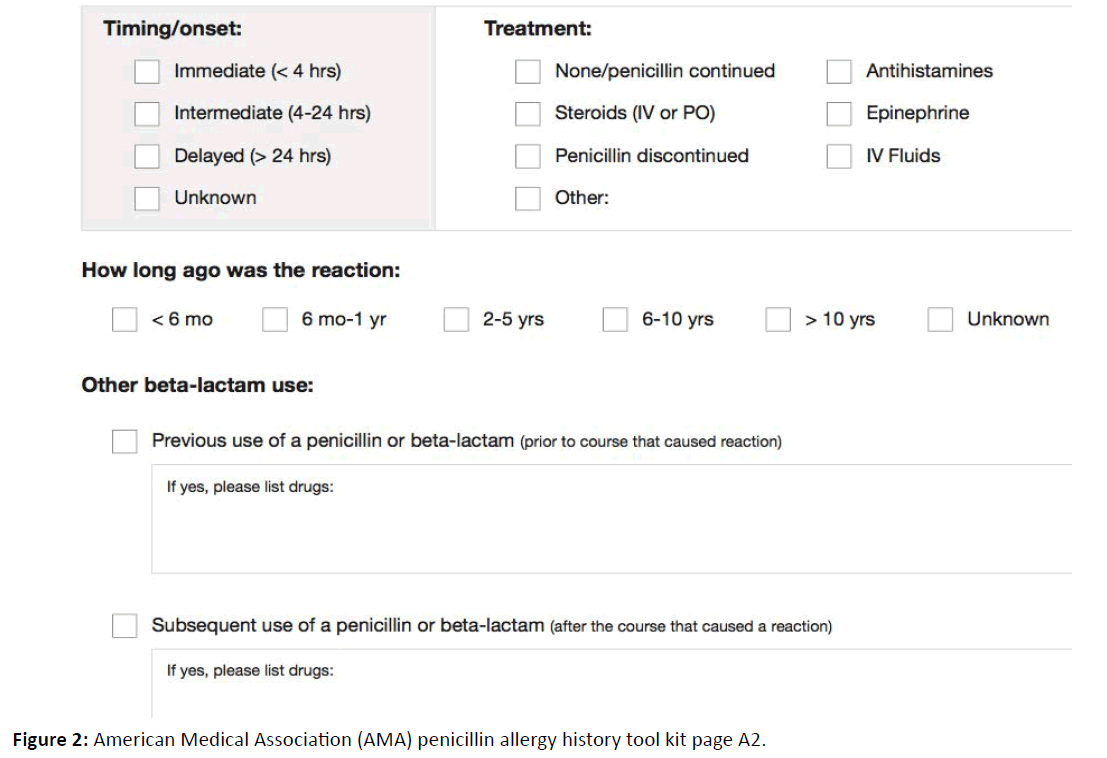
Figure 2: American Medical Association (AMA) penicillin allergy history tool kit page A2.
Following risk stratifications athletes determined to be intolerant to PCN were counseled on possible de-labeling without drug challenge. Athletes stratified into the low and moderate risk groups were offered consultation for drug challenge followed by possible re-labeling. Athletes determined to be high risk were advised that re-labeling was not recommended and to continue avoiding PCNs. No adjustments were made to athletes with indeterminant reactions to PCN.
The total collegiate athlete population was determined to be 415. 6.5% of athletes had an EMR documented allergy to PCN. 16 athletes were of female gender and 15 of male gender with all athletes being between the ages of 18 and 22 years old. Listed reaction to PCN in EMR included anaphylaxis 2 (7.4%), Hives/Rash 14 (52%) and 11 (40.6%) had no specific reaction documented.
Risk stratification
Based on risk stratification, athletes were offered [1] de-labeling without drug challenge, [2] consultation for drug challenge with possible re-labeling, or [3] advised against re-labeling. EMRRS categorized 0% of athletes to be high risk, 52% to be of moderate risk, 0% low risk and 40.6% of indeterminate risk. TP-RS determined 0% of athletes to be high risk, 37% to be of moderate risk, 29.9% low risk, 7.4% indeterminate risk and 25.9% intolerant to PCN.
Re-labeling without drug challenge (intolerant)
Athletes were not considered for de-labeling using EMR-RS. TP-RS identified 25.9% of athletes to be eligible for de-labeling without PCN drug challenge.
With the use of TP-RS, athletes with an EMR documented allergy to PCN could be decreased from 6.5% to 4.8% without drug challenge. Compared to EMR-RS, TP-RS increased the number of athletes who could undergo appropriate relabeling of PCN allergy by 25.9%.
Re-labeling not possible (high risk)
The number of athletes determined to be at high risk remained zero regardless of risk stratification method.
Re-labeling not possible (unknown pcn reaction)
Athletes with an unknown reaction to PCN was 40.6% following EMR-RS and 7.4% using TP-RS. TP-RS compared to EMR-RS increased the number of athletes who could hypothetically be re-labeled to 48% of athletes a 33.2% difference.
Consultation for drug challenge for possible re-labeling (moderate & low risk)
52% of athletes qualified for drug challenge with EMR-RS. Using TP-RS a total of 66.9% athletes were determined to be of moderate or low risk and eligible for drug challenge. TPRS compared to EMR-RS increased the number of athletes who could undergo hypothetical relabeling of PCN allergy through drug challenge by 14.9%. Among the 18 athletes offered consultation, 44.4% refused consultation and 55.5% agreed. The total number of athletes who successfully completed consultation and determined eligible for drug challenge were not included in this study.
Quality improvement using risk stratification
In the absence of risk stratification the total number of athletes with an EMR documented allergy to PCN from our institution was 6.5%. Based on EMR-RS 16 of the 27 athletes with a listed PCN allergy were falsely labeled. Therefore the total number of athletes with a true PCN allergy is hypothetically 11 or 2.65%. EM-RS was able to identify 3.85% of athletes who were inappropriately labeled as allergic to PCN.
TP-RS determined 2 or 0.48% of athletes with a documented PCN allergy to have a true allergy. TP-RS identified 6.02% of 6.5% of athletes who were inappropriately labeled as allergic to PCN. TP-RS was able to identify 92.59% of athletes to be falsely labeled as allergic to PCN, compared to 40.7% identified by EMR-RS, a difference of 51.89%.
Approximately 32 million Americans have a reported allergy to PCN. Approximately 10% of US residents have been labeled as allergic to penicillin, often since childhood. Current evidence suggests that as few as 10% of people who report they’re allergic to the antibiotic have a true allergy [1-6]. Therefore less than 1% of US resident are expected to have an allergy to PCN. This quality improved study sought to establish the prevalence of a true PCN allergy among collegiate athletes. When compared to our current evidence which suggests 1% of the US population has a true allergy to PCN rather than 10% who report an allergy to PCN, our collegiate athlete population of 415 athletes would theoretically have 41.5 athletes with a documented PCN allergy in their EMR. Based on previous research 1% of the 41.5 athletes with a documented allergy to PCN would have a true allergy. Hence the number of athletes with appropriate documentation of PCN allergy on their EMR would be 0.415%.
EMR analysis determine that 6.5% of collegiate athletes had an EMR documented allergy to PCN. Against our hypothesis this was less than the 10% of US residents with a documented PCN allergy determined by previous research. From our analysis 27 athletes had a documented PCN allergy on their EMR, but following TP-RS theoretically only 2 athletes would have a true allergy to PCN. Although our collegiate athlete population with inappropriately documented EMR PCN allergy is less than that reported among US population studies our quality improvement efforts found 92.59% of athletes with a PCN allergy listed on their EMR unlikely to have a true allergy. For that reason a quality improvement stewardship program to relabel PCN allergies should be considered in the collegiate athlete population. The use of quality improvement stewardship to care for collegiate athletes is not of common practice. This study is an example of how quality improvement research can make a significant impact in the welfare of our athletes and for healthcare as a whole.
Although EMR data analysis can assist in appropriately labeling PCN allergies in the EMRs of collegiate athletes there is a potential for misleading results and subsequent missed opportunities for quality improvement. As seen in this study, although EMR-RS is useful it does not have the potential impact that TP-RS has for the purpose of appropriately relabeling PCN allergies in athletes. Evident from this study, TP-RS compared to EMR-RS can significantly improve the outcomes of relabeling PCN allergies in collegiate athletes (TP-RS identified 39.9% more false PCN allergies compared to EMR-RS). Team physicians should use clinical assessment in addition to EMR analysis to provide high quality care to their athletes.
Role of the team physician
Our study has identified the superiority of team physician involvement compared to data analysis alone warranting a promotion of team physician PCN allergy risk stratification education. Team physicians should undergo training to learn how to appropriately alter listed allergies in the athlete’s EMR in addition to using guided toolkits to assist in risk stratifying athletes with a documented PCN allergy.
In cases where the athlete is confident that he/she has tolerated a penicillin class antibiotic since the index reaction the team physician can consider documenting administration in the EMR of a penicillin class antibiotic that was tolerated since the index reaction and subsequently de-labeling the athlete. If the athlete has a history of an intolerance (e.g. gastrointestinal upset, chills, headache, fatigue) that is listed as an allergy or adverse reaction, the EMR should be updated to reflect this reaction as an intolerance and not an allergy. De-labeling without a drug challenge should be determined by the comfort level of the team physician. If the team physician is not secure in removing the PCN allergy by chart review and patient history only, the athlete should be referred for specialist consultation.
When further verification is desired by the team physician, athletes qualifying for direct oral challenge should include athletes with one or more of the following [1] unknown, remote (>10 year ago) reaction, [2] itching (pruritus) without rash, [3] family history, and [4] the athlete denies allergy or unsure of where it came from but cannot confirm he/she tolerates a penicillin class antibiotic by patient history or chart review. Athletes who meet qualifications for PCN skin test followed by oral challenge include those with (1) Moderate – High risk allergy histories after risk stratification. It is recommended that athletes with an anaphylaxis type reaction that has occurred in the last 5 years are not referred to allergy/immunology for consultation. The lag time for PCN skin testing and oral challenge varies by type of clinical practice. The cost for skin test and oral challenge is dependent on athlete’s insurance and/ or athletic department’s insurance [1,2,6].
If a team physician(s) should decide to pursue a quality improvement stewardship PCN allergy relabeling program within their institution, regardless of outcome, a shared EMR list (e.g. outpatient PCN assessment) of athletes who undergo PCN allergy assessment should be created. In athletes who are de-labeled, antibiotic usage should be assessed 1 year prior and 1 year after intervention by searching outpatient/inpatient dispensing records Inpatient and outpatient drug acquisition costs will be utilized to estimate costs before and after allergy de-labeling. Consider following athletes after de-labeling to assess if relabeling occurs due to inaccurate documentation or new reaction to a PCN class antibiotic. Prior to exiting their athletic program, athletes should be re-educated to prevent relabeling in the future.
Study limitations
Although this study was limited to a sample population of only Division 1 athletes at a single institution the sample was diverse and included almost equal number of female and male athletes who played a variety of sports. Indeed the age range of our population was small (18 to 23 years old) it represents the age range of other collegiate athletic populations within the United States.
Recall bias is a concern in this study as participants were asked about an allergy that was diagnosed most commonly during childhood. This will be a challenge in all populations being asked to recall their PCN allergy reaction and possibly even more so in older populations who have more lag time from initial allergic reaction to clinical interview.
The reduction in PCN allergy labeling in our study was theoretical and not based on actual results from oral or skin PCN challenge. Regardless, this data provides useful insight regarding the inappropriate documentation of PCN allergy within the EMR. It should be mentioned that our findings may have been skewed by the 2 athletes with indeterminate PCN reactions although other population samples would likely have participants with similar findings.
8 of the 18 athletes who qualified for drug challenge deferred allergy/immunology consultation when offered. Their true understanding of a PCN drug challenge is questionable and may be different in a non-theoretical situations. Although 10 athletes agreed to allergy/immunology consultation the true number who underwent drug challenge was not determined. Our study assumed that all 10 athletes underwent drug challenge and were determined to not have a true allergy to PCN. It could be assumed that 1 of the 10 athletes had a true allergy given US population studies showing that 1% of report PCN allergies are indeed true allergies [1]. In this case our outcome would have shown less benefit of TP-RS for relabeling of falsely documented PCN allergy.
The advantages of a PCN relabeling program for collegiate athletes has not been confirmed. How re-labeling of PCN allergy within an athletes EMR affects the use of unnecessary broad-spectrum antibiotics, healthcare costs, hospital stays, and antimicrobial resistance as well as antibiotic adverse events, is outside the scope of this study and likely depends on specific demographics.
Future directions
Determining the true rather than hypothetical number of falsely documented PCN allergies following drug challenge in collegiate athletes should be verified in future studies.
The reasons that athletes may defer consultation for drug challenge should consider multiple barriers including but not limited to athlete awareness and fear, access to resources, financial ability, insurance, and time. Further investigation should focus on the reasons collegiate athletes refuse or fail to complete PCN allergy drug challenge. The details encompassing limited compliance should be compared to other study populations.
Prospective trends should establish potential advantages of utilizing quality improvement research to optimize care in the athletic population. Team physician understanding of quality improvement research and how it can be incorporated into their practice should not only be assessed but also promoted. Influencing team physicians to incorporate quality improvement research into their already demanding schedule poses a challenge. The use of TP-RS should be assessed in other clinical scenarios not related to PCN allergy re-labeling. Team physicians who excel at superior primary care or live in remote areas where specialty clinics are not available should be encouraged to ascertain the skills necessary to provide drug challenges for appropriate athletes.
Whether or not relabeling of inappropriate PCN allergies within the EMR leads to a decrease in the use of unnecessary broadspectrum antibiotics, healthcare costs, longer hospital stays, and antimicrobial resistance as well as increased antibiotic adverse events, should be assessed in future research.
Our current literature suggests that 10% of the US population has a documented allergy to PCN with less than 10% being a true allergy (1% of the US population). Among our collegiate athlete population, 6.5% had a EMR documented allergy to PCN which is less than the US average. Among the 6.5% of athletes with a PCN allergy documented on EMR, TP-RS identified only 0.48% of these athletes to be truly allergic to PCN. TP-RS was able to identify 92.59% of athletes to be falsely labeled as allergic to PCN, compared to 40.7% identified by EMR-RS, a difference of 51.89%.
Quality improvement projects can be used within the collegiate athlete population. Team physician involvement is superior to EMR data analysis alone for identifying false documentation in the EMR of collegiate athletes.
The University of South Florida Athletic Department