Review Article - (2018) Volume 0, Issue 0
1Division of Hepato-Biliary-Pancreatic Surgery, Department of Surgery, Kobe University Graduate School of Medicine, Kobe, Japan
2Department of Surgery, Kohnan Hospital, Kobe, Japan
Received Date: June 02nd, 2017; Accepted Date: October 05th, 2017
Pancreatic neuroendocrine neoplasms are rare tumors with diverse biological behavior. World Health Organization classifications 2010 of neuroendocrine neoplasms based on Ki67 and Mitotic indexes has been widely accepted as correlating favorably with patient prognosis. WHO classification 2017 has been updated on the basis of recent studies on pathological differentiation of “G3 tumors” in the 2010 classification. Neuroendocrine neoplasms are largely classified into well differentiated neuroendocrine tumors and poorly differentiated neuroendocrine carcinomas based on their pathological differentiation. NETs are further classified into NET G1, G2, and G3 based on their Ki67 and Mitotic indexes; NECs are classified as NEC G3. In this review, WHO classification, TNM classification and further prognostic factors are described.
Neuroendocrine Tumors; Prognosis; World Health Organization
NECs neuroendocrine carcinomas; NETs neuroendocrine tumors
Pancreatic neuroendocrine neoplasms, rare tumors of the pancreas that constitute 1–2% of all pancreatic malignancies, are a highly heterogeneous mixture of tumors that originate from pluripotent stem cells [1, 2]. Their biological behavior varies widely from nearly benign tumors to malignant ones that give rise to metastasis and local invasion. Most are known as slow growing tumors and demonstrate better prognosis than pancreatic ductal adenocarcinoma (PDAC) [3, 4]. Despite numerous reports on newly diagnosed pancreatic neuroendocrine neoplasms, their biological behavior is still not fully understood. In particular, identifying the prognostic factors for pancreatic neuroendocrine neoplasms has been challenging because of their rarity and heterogeneous nature [5]. World Health Organization (WHO) classification 2010 classifies neuroendocrine neoplasms based on their Ki67 and Mitotic indexes [6], and it is not only the most widely accepted classification and grading system, but also valuable in predicting prognosis [7]. In 2017, the WHO classification will be updated on the basis of recent evidence.
WHO Classification 2010
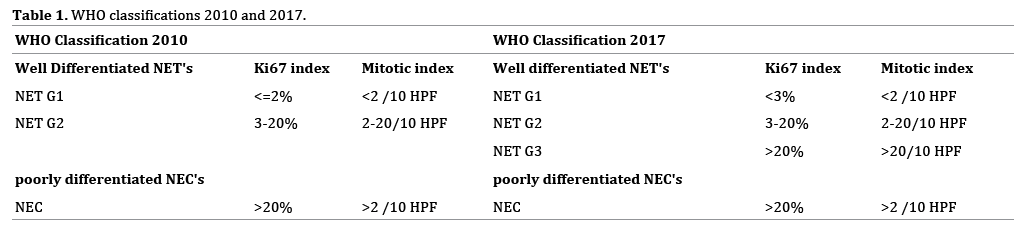
The European Neuroendocrine Tumor Society (ENETS) proposed classifying neuroendocrine neoplasms into well differentiated neuroendocrine tumors (NETs) and poorly differentiated neuroendocrine carcinomas (NECs) based on Ki67 and Mitotic indexes for the first time in 2007; the classification correlates favorably with patient prognosis [8]. Subsequently, under WHO classification 2010, neuroendocrine neoplasms have been divided into three grades by adopting the ENETS classification (Table 1): NET G1 (Ki67 index ≤2% and Mitotic index <2/10 high power field (HPF)), NET G2 (Ki67 index 3-20% or Mitotic index 2-20/10 HPF) and NEC (Ki67 index >20% or Mitotic index >20/10 HPF) [6]. The efficacy of the classification criteria in terms of predicting prognosis has been validated in numerous studies including a large international cohort study which included 1072 patients, whereby the 5-year survival rate of NET G1 is about 95%, of NET G2 about 75% and of NEC about 25% (Figure 1) [7].
WHO Classification 2017
Recent studies have shown that NECs under WHO classification 2010 is heterogeneous; it comprises well differentiated and poorly differentiated groups in terms of pathological differentiation, and well differentiated groups demonstrate significantly better prognosis than poorly differentiated ones [9, 10]. Therefore, neuroendocrine neoplasms need to be subdivided on the basis of not only Ki67 and Mitotic indexes, but also pathological differentiation.
Under WHO classification 2017 (Table 1), neuroendocrine neoplasms are primary classified into well differentiated NETs and poorly differentiated NECs based on pathological differentiation. Subsequently, well differentiated NETs are classified into NET G1 (Ki67 index <3% and Mitotic index <2/10 HPF), NET G2 (Ki67 index 3-20% or Mitotic index 2-20/10 HPF) and NET G3 (Ki67 index >20% or Mitotic index >20/10 HPF). Poorly differentiated NECs are classified as NEC G3 (Ki67 index >20% or Mitotic index >20/10 HPF). In consequence, NECs under WHO classification 2010 came to be subdivided into two groups under WHO classification 2017; well differentiated groups are NET G3 and poorly differentiated groups are NEC G3 [11].
The differences between NET G3 and NEC G3 are summarized in Table 2. The usual Ki67 index for NET G3 and NEC G3 is 30-55% and >50%, respectively. NET G3 has neuroendocrine marker (Chromogranin A and Synaptophysin) expression, somatostatin receptor scintigraphy uptake and loss of alpha thalassemia/mental retardation syndrome X-linked (ATRX) or death-domain associated protein (DAXX) protein expression. On the other hand, NEC G3 has abnormal Rb, p53, SMAD4 expression, and tumor necrosis is commonly observed [12, 13, 14]. NEC G3 rarely involves genetic syndromes like MEN1 or von Hippel-Lindau disease, and rarely has any function. NEC G3 has a poor prognosis, but a better response to platinum agents than does NET G3 [10, 15].
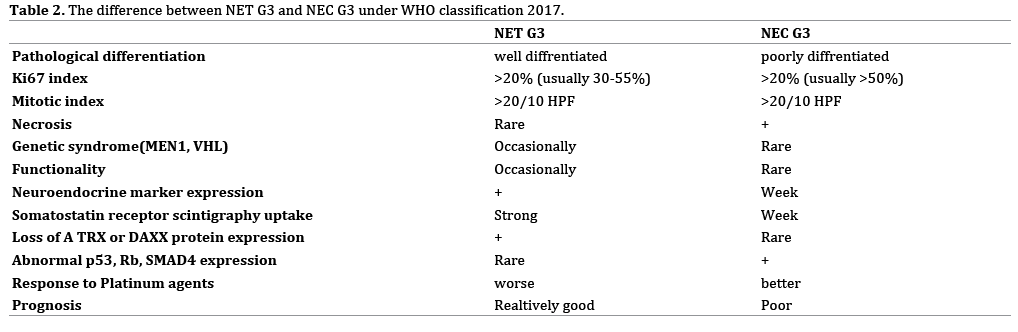
Since the population of pancreatic NET G3 and NEC G3 is small, their precise prognosis has not been well understood. There has been a small retrospective study which included 50 patients with NET G2, 19 patients with NET G3, and 42 patients with poor ly differentiated NECs. In this study, the 5-year survival rate of NETG3 has been estimated at about 29% and that of NEC G3 at about 16% (Figure 2) [9]. The prognosis of pancreatic neuroendocrine neoplasms under new WHO classification 2017 has to be further evaluated in largescale studies.
Other alterations in WHO classification 2017 include the cutoff value of the Ki67 index for NET G1/G2; several studies have shown that a Ki67 index of 5% or 10% is a better cutoff value than one of 2% [7, 16, 17]. Nonetheless, this classification shows a slightly different threshold Ki67 index of 3%, which might not significantly affect the prognosis of NET G1 and G2.
TNM Classification
Like other tumors, pancreatic neuroendocrine neoplasms are also classified by tumor/node/metastasis (TNM) classification. WHO classification is a malignancy grading based on the biological behavior of neuroendocrine neoplasms; on the other hand, TNM classification is a clinical staging for mortality risk assessment based on the anatomical extent of neuroendocrine neoplasms. Two major TNM classifications of pancreatic neuroendocrine neoplasms have been proposed by ENETS and the American Joint Cancer Committee/Union for International Cancer Control (AJCC/UICC). The ENETS TNM is specifically designed for pancreatic neuroendocrine neoplasms; on the other hand, the AJCC/UICC TNM classification (7th edition) is primarily designed for PDAC [18]. Compared with PDAC, pancreatic NETs are slow growing tumors, large at diagnosis, limited to the pancreas and metastasize during the late course of the disease. Thus, several studies have shown that the ENETS classification of TNM is more accurate than that of AJCC/UICC (7th edition) and is recommended for use on pancreatic neuroendocrine neoplasms [7].
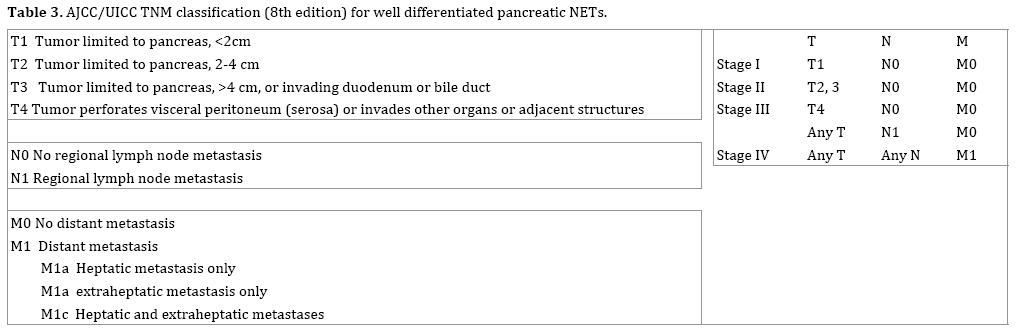
In 2016, the AJCC/UICC TNM classification was revised and updated to the 8th edition (Table 3) [19]. In the revision, pancreatic neuroendocrine neoplasms are divided into two groups based on the Ki67 and Mitotic indexes: well differentiated pancreatic NETs are defined as those with a Ki67 index of ≤20% and a Mitotic index of ≤20/10 HPF; high-grade pancreatic NECs are defined as those with a Ki67 index of >20% or a Mitotic index of >20/10 HPF. Well differentiated pancreatic NETs are classified similar to the ENETS TNM classification and high-grade pancreatic NECs are classified as PDAC. The prognostic value of the AJCC/UICC TNM classification (8th edition) for pancreatic neuroendocrine neoplasms needs to be validated through a large-scale study.
Further Prognostic Factors
Besides WHO classification and TNM classification, numerous studies have described further prognostic factors to enhance the stratification of pancreatic neuroendocrine neoplasms, which include clinicopathological, radiological, molecular and genetic features.
The presence of liver metastasis has been mentioned as one of the most valuable prognostic factors in the ENETS guidelines [20, 21]. The prognosis of patients with stage IV pancreatic neuroendocrine neoplasms is a heterogeneous because metastatic sites, number, or metastatic pattern are not specified in the present TNM classifications. There have been some studies described the liver metastatic pattern as prognostic factors [22]. The extent of liver metastasis either unilobar, bilobar or the presence of the extraabdominal metastasis is a predictor of overall survival. Nonetheless, the clinical impact of distant metastasis as prognostic factors is still controversial and can change greatly with advances in the treatment [23].
As for the radiological features, the calcification on computed tomography, the status of 18F-fluorodeoxy glucose uptake on 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) and the status of somatostatin receptor scintigraphy (SRS) uptake have been described as prognostic factors [24, 25, 26]. Previous study has shown that calcified pancreatic neuroendocrine neoplasms on preoperative computed tomography were predictive of NET G2 as opposed to NET G1 and correlate with lymph node involvement [24]. Others reported that the patients with FDG-PET-positive and/or SRS-negative had a worse overall survival than those with FDG-PET- negative and/or SRSpositive [25, 26]. We have recently published a study that focused on the tumor invasion; the patients with stenosis and upstream dilatation of the main pancreatic duct on preoperative magnetic resonance cholangiopancreatography had worse recurrence-free-survival than did those without involvement [27].
As for the molecular biological markers, plasma chromogranin A, loss of DAXX or ATRX, loss of heterozygosity (LOH) of the pleckstrin homology like domain family A member 3 (PHLDA3) gene, have been described as prognostic factors [28, 29, 30, 31, 32, 33]. Chromogranin A is a known diagnostic tumor marker for neuroendocrine neoplasms. Previous studies have shown that the increase of plasma chromogranin A levels is associated with poor clinical outcomes for the patients with pancreatic neuroendocrine neoplasms [28, 29]. Mutations in DAXX or ATRX have been detected in 40% of pancreatic neuroendocrine neoplasms. These mutations were associated with better clinical outcome [30]. Loss of DAXX or ATRX is associated with chromosome instability in pancreatic neuroendocrine neoplasms and correlated with tumor stage and metastasis, reduced time of relapse-free survival, and decreased time of tumor-associated survival [31]. PHLDA3 have a tumor suppressive function of pancreatic neuroendocrine neoplasms via repression of Akt activity and various Akt-regulated biological processes. The patients exhibiting LOH at the PHLDA3 locus seemed to have a poorer prognosis compared with the patients without LOH [32, 33].
Various novel prognostic factors based on clinicopathological, radiological, and genetic features are increasingly identified and contributed to more detailed prognostic stratification in association with the WHO classification and TNM classification.
The WHO classification is useful to predict the prognosis and select proper therapeutic options of the pancreatic neuroendocrine neoplasms. Recent studies have shown that NECs under WHO classification 2010 comprises well differentiated and poorly differentiated groups in terms of pathological differentiation, and well differentiated groups demonstrate significantly better prognosis than poorly differentiated ones. The WHO classification has been updated in 2017 and NECs under WHO classification 2010 came to be subdivided into well differentiated NET G3 and poorly differentiated NEC G3. In addition to WHO classification, TNM classification and further prognostic factors are also valuable to predict the prognosis. In this review, we described the alterations in the latest upgrade of these classifications and introduced further prognostic factors.
The authors have no financial conflicts of interest concerning the manuscript to disclose.