Case Report - (2016) Volume 17, Issue 3
Elias Makhoul, Neemtallah Basile, Georges Aftimous, Anthony Zaarour
Department of 1Gastroenterology, 2Surgery, and 3Anatomopathology, University Hospital Notre Dame de Secours, Byblos, Lebanon
*Corresponding Author:
Elias Makhoul
Hepato Biliary & Pancreas Division
Faculty of medicine and sciences Holy spirit University
University hospital Notre Dame De secours Jbeil
BP: 3 Byblos
Lebanon
Phone +9613711787 / +9619944480
E-mail eliemakhoul@hotmail.com / eliasmakhaoul@chu-org.lb
Received November 04th, 2015-Accepted Janaury 02nd, 2016
Hydatidosis remains endemic in many countries of the world and is caused by the tapeworm Echinococcus granulosus which produces cysts. The liver and the lungs are the most commonly involved organs although cysts can occur in other viscera. Primary Pancreatic location is uncommon with a frequency of less than 1% of the various locations. We hereby report one observation of isolated hydatid cyst of the caudal part of the pancreas in a patient suspected to have an Intraductal Papillary Mucinous Tumor.
Keywords
Pancreas
INTRODUCTION
Hydatidosis remains endemic in many countries of the world, caused by the tapeworm Echinococcus granulosus which produces cysts. The incidence rates reach more than 50 per 100 000 person-years, and prevalence levels as high as 5%–10% occurring in parts of Argentina, Peru, East Africa, Central Asia and China. The liver and the lungs are the most commonly involved organs although cysts can occur in other viscera. Primary Pancreatic location is uncommon with a frequency of less than 1% of the various locations. We hereby report one observation of isolated hydatid cyst of the caudal part of the pancreas in a patient suspected to have an Intraductal Papillary Mucinous Tumor.
CASE REPORT
A fifty-two-year-old female patient with unremarkable past medical and surgical history presented to our department with a chief complaint being a diffuse abdominal pain which began three months ago associated with nausea, repeated vomiting and weight loss of 6 kilograms in the last month.
Her situation deteriorated 15 days prior to her presentation, as she began to suffer from severe localized epigastric pain along with complete loss of appetite to the extent of which anti-emetics and pain medications were no longer of a good relief.
Upon examination, the patient had normal vital signs and was well conscious and oriented with normal skin color. Her abdomen was soft with a moderate to severe pain on palpation of the epigastric region; as per the rest of the exam, it was strictly normal.
The patient was admitted and treated by intravenous PPI and antispasmodics. Routine laboratory tests showed hypereosinophilia (15%) and a high ESR (50), liver function tests, lipase and CRP were normal. An abdominal CT scan showed a mutilocular (8 cm x 5 cm) corporeocaudal pancreatic mass with no other structural changes (Figure 1).
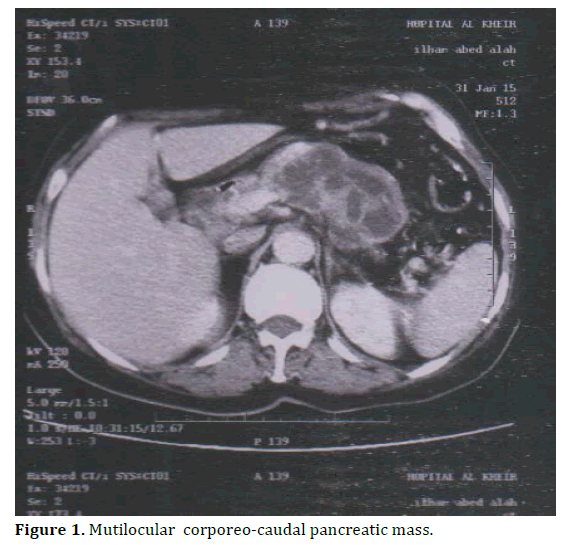
Figure 1. Mutilocular corporeo-caudal pancreatic mass.
Based on these findings, the hypothesis of an IPMN was raised, among other less probable diagnoses such as pancreatic pseudocyst. An MRCP was done and the results came back incompatible with the previously raised diagnoses. Tumor markers (CEA, CA 19-9) were negative. The anti- Echinococcus serum antibodies were undetectable. Upon these findings, a biopsy under ultrasonographic guidance was done without any complication.
The pathology results showed a flaky, structureless acidophilic membrane and a pancreatic fibro-hyaline wall infiltrated with leukocytes and eosinophils. This aspect was compatible with a hydatid cyst. (Figure 2). The patient was given Albendazole for 3 months, after which a CT scan was done and found no improvement of the lesion (Figure 3). The decision was made to go for a caudal pancreatectomy which was done successfully. We noted the presence of daughter cysts into the lesion (Figures 4, 5).
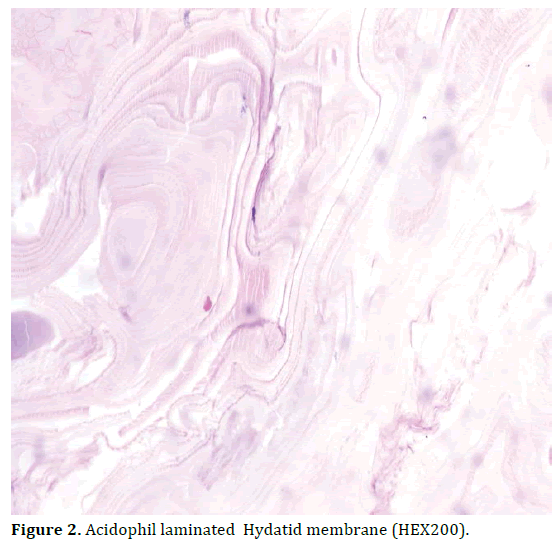
Figure 2. Acidophil laminated Hydatid membrane (HEX200).
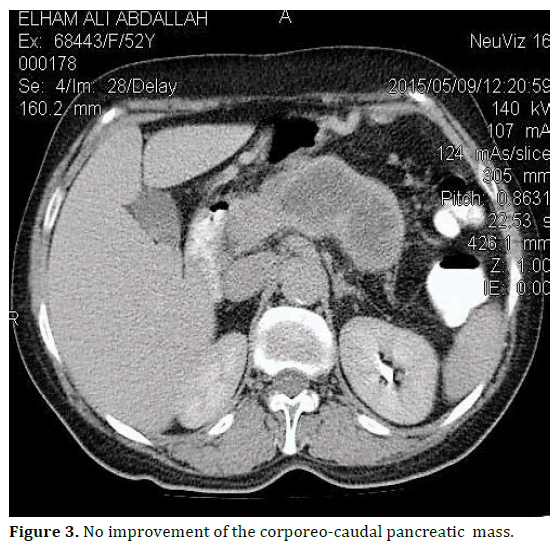
Figure 3. No improvement of the corporeo-caudal pancreatic mass.
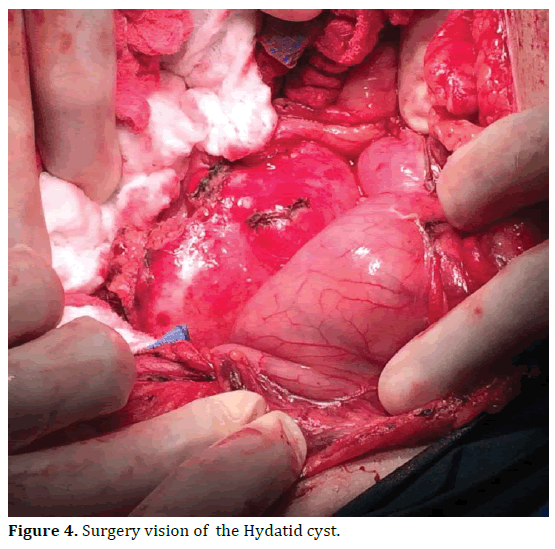
Figure 4. Surgery vision of the Hydatid cyst.
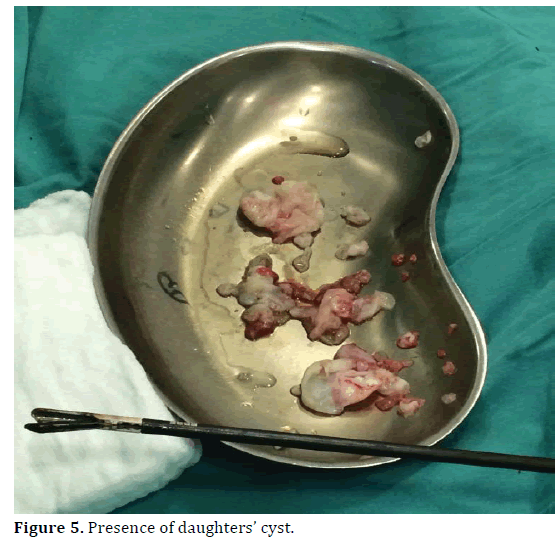
Figure 5. Presence of daughters’ cyst.
The postoperative period was uneventful and the patient was discharged on postoperative day 7. The patient was given Albendazole for 3 months. The clinical and ultrasonographic follow-up did not show any recurrence (Figure 6).
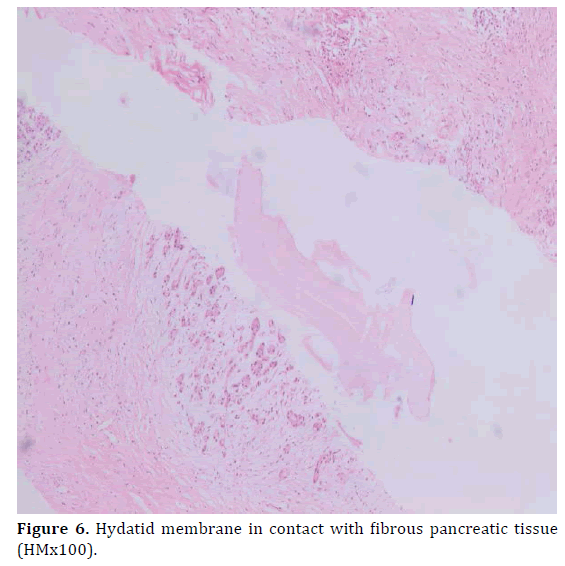
Figure 6. Hydatid membrane in contact with fibrous pancreatic tissue (HMx100).
DISCUSSION
Hydatid disease is an important pathogenic, zoonotic and parasitic infection of humans mainly caused by infection in the larval stage of the dog tapeworm Echinococcus granulosus. The disease is spread when food or water that contains the eggs of the parasite is eaten or by close contact with an infected animal [1]. Echinococcus eggs contain an embryo that is called an oncosphere .These embryos penetrate the wall of the intestine into the portal vein and are carried in the bloodstream to vital organ. In 50-70% of cases, the liver is the final destination of the intermediate host. If the embryo bypasses the liver; the lung is the next most frequently involved organ. If the embryo continues through the pulmonary capillary bed, the hydatid cyst may develop by arterial passageway at any site in the body like bone, brain, kidney, spleen and orbit [2, 3].
The hydatid cyst of the pancreas is rare. The frequency varies from 0.2 to 0.6% [2, 4, 5] and the location is usually single and isolated. According to Dahniya et al, it occurred in only 1 of 357 cases of hydatid disease over a 20-year period [6]. An association with other sites may be encountered in 9% of cases where it is usually hepatic and rarely pulmonary [2, 3, 5, 7]. The seat of the cyst in the pancreas is cephalic in 57% of cases, corporeal and caudal in 24% and 19% of cases respectively [2, 3, 7, 8, 9]. Furthermore, the cyst could develop as being intraparenchymal in 35% of cases and peripheral externalized to the surface in 65% of cases [8, 9]. With our patient, the cyst was caudal and parenchymal.
Clinical presentation is variable and insidious, depending on the cyst’s location and size. The patient could be asymptomatic even though the cysts are too large. On the other hand, if the patient is symptomatic, the localization of the cyst is the main factor affecting the type of symptoms that will occur. 60% of patients present with an abdominal mass, epigastric pain or discomfort, vomiting and weight loss. Obstructive jaundice, Cholangitis, duodenal stenosis or fistula, acute and chronic pancreatitis, pancreatic abscess due to compression and erosion into the pancreatic ducts are unusual complications of hydatid cysts involving the head of the pancreas [7, 10]. A cystobiliary- digestive fistula can also be seen in 0.5% of cases [3, 11, 12]. Cysts in the body and tail of the pancreas may be asymptomatic or may present as a palpable mass. Mesenteric vein thrombosis and portal hypertension is found in 14% of cases, and it is often asymptomatic [12, 13, 14]. Rarely, the cyst ruptures spontaneously into the peritoneal cavity or gastrointestinal tract, causing abscess formation [10, 13].
The definitive diagnosis of Hydatid disease of the pancreas can be made only during surgery [10, 15]. The serological diagnosis is based on enzyme-linked immunosorbant assay (ELISA) for anti-echinococcal antibody, indirect fluorescent antibody test, or latex agglutination test which is positive in over 85% of infected patients [16, 17]. Ultrasound, CT Scan and magnetic resonance imaging (MRI) [10, 16] of the abdomen should be performed although a proper detection of a cyst is not always present using these modalities. However, the presence of multiloculation, curvilinear calcifications or presence of daughter cells is very helpful in identification of these lesions. Moreover, hydatid cyst should be included in the differential diagnosis of cystic lesions of the pancreas such as pseudocysts whose prevalence range from 6% to 18.5 % in acute pancreatitis and from 20 % to 40 % in chronic pancreatitis [1], cystadenomas, cystadenocarcinomas or Intraductal Papillary Mucinous Tumors [2, 3, 9] especially in endemic areas, even with a negative serological indirect test for Echinococcus granulosus [16].
The definitive treatment of hydatid cyst of the pancreas after failure of oral treatment is surgical. Sterilization of the cyst before surgery, with a scolicidal solution to prevent dissemination, is indicated. As per the choice of surgery, it usually depends on the localization of the cyst and the presence of cysto-biliary or cysto-digestive fistula [3, 6, 7, 10, 11, 14].
In the case of corporeo-caudal cysts such in our case, a radical caudal pancreatectomy or splenopancreatectomy is indicated. As per cephalic ones, the choice of conservative percutaneous drainage is an alternative to surgery for patients with high surgical risk, because a pancreaticoduodenectomy is deemed excessive for a benign pathology [14]. In such cases, drainage must be combined with medical chemoprophylaxis using Albendazole and Praziquantel [6, 10, 17].
CONCLUSION
The hydatid cyst of the pancreas is a rare disease. The diagnosis should be considered when facing any pancreatic cystic mass especially in endemic countries. Additionally, a unique and isolated pancreatic location tends to make the diagnosis difficult whereas it is easier in the presence of hepatic hydatid cyst.
Conflict of Interest
The authors declare that they have no competing interests.