- (2015) Volume 16, Issue 6
Eugene Pahk1*, Raphael Jesin2, Yoram Kluger3, Ron Epelbaum4, Jesse Lachter5
1Technion Medical School, Haifa, Israel
2Staten Island University Hospital, New York, U.S.A
Departments of 3Surgery, 4Oncology and 5Gastroenterology, Rambam Healthcare Campus, Haifa, Israel
Received: June 04th, 2015 Accepted: July 26th, 2015
Objective To determine the time to recurrence of pancreatic adenocarcinoma of the head of the pancreas after curative resection at one tertiary-care Health Care Campus and to determine the factors that predict early recurrence. Methods Retrospective data was gathered from 64 consecutive pancreatic adenocarcinoma patients undergoing curative Whipple procedures from 2007-2011. Patients were divided into early recurrence, within 185 days, and late or no recurrence. Results Disease-free survival after 6 months was 64%; at 8 months, it was 50%. Factors that contributed to early recurrence included increased age at surgery (P=0.03746), larger tumor size on pathology (P=0.0093), and resection margins less than 0.1mm (P=0.0471). Larger tumor size as measured by endoscopic ultrasound showed a trend for early recurrence (P=0.086821). Conclusions Aggressive screening and detection mechanisms for pancreatic carcinoma should be applied more frequently and with increased age to ensure identification of pancreatic carcinoma before large growth in tumor size.
Adenocarcinoma; Carcinoma; Pancreas; Pancreatic Neoplasms; Recurrence; Whipple Disease
Pancreatic cancer is one of the most lethal malignancies. During 2011, in the United States, approximately 37,660 patients died due to pancreatic cancer. The yearly incidence of pancreatic cancer is around 44,030 men and women [1]. In Israel, it ranks third among cancer related deaths despite only being between twelfth to fifteenth in incidence [2]; the overall five year survival rate is less than 5% [3]. The main reason for these poor results is the combination of late onset of symptoms and lack of efficient screening and detection. The progression to adenocarcinoma is a long process with the first DNA somatic mutations of oncogenes occurring at least ten years before the patient presents clinically [4]. However, investigations usually only begin by the time the patient begins to experience weight loss, jaundice, or pain, at which point 80-85% will be deemed to be at an unresectable stage of their disease [5, 6]. This has a huge impact on patient outcomes and response to treatment.
The surgical procedures used for extirpation of pancreatic cancers include distal pancreatectomy and mid-pancreatectomy(rarely), but the most common is the pancreatoduodenectomy, also known as the Whipple operation. Even with early diagnosis, 80% of those patients undergoing tumor resection will eventually have recurrence of their disease within 2 years. This usually presents as either as local recurrence or hepatic metastases [7]. The median time to recurrence has been reported to be approximately 8 months [8].
Given that the Whipple’s operation is far from benign with significant peri-operative mortality and morbidity [9], the possibility of recurrence of pancreatic adenocarcinoma should be considered strongly as part of the indications for the Whipple procedure. There have been numerous studies looking at factors that influence both survival and recurrence after curative resection. Some factors that have been shown to be significant include, tumor size, histological grading, node status, resection margins, and positive family history [10-12]. While these studies have been useful in establishing prognoses, they are limited in their ability to evaluate how well we can predict whether a patient is a suitable candidate for surgery. This study, while including many of the factors studied previously, attempts to focus on preoperative evaluation techniques and their ability to predict outcome.
The aim of this study is to look at various parameters that may affect the time to recurrence of adenocarcinoma of the head of the pancreas after curative resection. This information could lead to a reduction in the amount of unnecessary surgeries that lead to significant mortality and morbidity without providing any advantage to long term patient benefits. While many previous studies have looked at both survival and recurrence, recurrence might be a better end point as it provides a better indication of the progression of the disease itself without being influenced by co-morbidities.
The patient population was selected from the past 200 consecutive pancreatic operations performed in a single healthcare campus. This was a retrospective study looking at operations that occurred between January 2007 and September 2011. They were all performed by the same surgeon to remove physician proficiency as a confounding factor. The patients were only included if they were operated on for adenocarcinoma of the pancreas with curative intent. Patients who died peri-operatively within three weeks were excluded, and several patients who were citizens of foreign countries who returned to their home countries afterwards were not included due to inability to follow-up. After excluding criteria were taken into account, a total of 64 patients were examined in this study. The patients were determined whether to have had early recurrence or not by documentation of imaging studies showing secondary disease within six months (185 days) of their surgery or suspicion of recurrence(e.g. rises in Ca19-9) within six months that led to confirmatory imaging of secondary disease.
A wide number of parameters were examined with regards to both early recurrence and late recurrence. The parameters chosen include demographic information(e.g. place of birth, age), clinical presentation(e.g. pain, jaundice), imaging modalities(e.g. EUS, CT), various surgery and pathology parameters, serum tumor markers, adjuvant therapy, and smoking.
Descriptive statistics such as frequencies, median, and percentiles, are demonstrated to the whole variable. Fisher’s exact test was used for differences between categorical variables. Students two sampled unpaired t-test was used for analyzing continuous variables. P values less than 0.05 were considered significant while P values between 0.05 and 0.1 were considered to be trending.
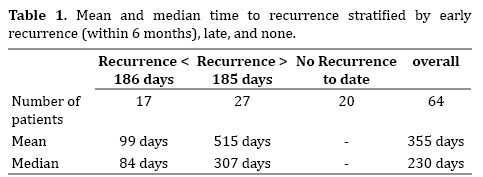
Of the 64 patients in the study, there were 33 males and 31 females. 54 were Jewish. 9 were Arab. 17 had evidence of recurrence within 6 months with the mean and median time being 99 and 84 days respectively. 47 patients either had evidence of recurrence after 6 months or no evidence at all. The overall mean time to recurrence was 355 days with a median of 230 days (Table 1).
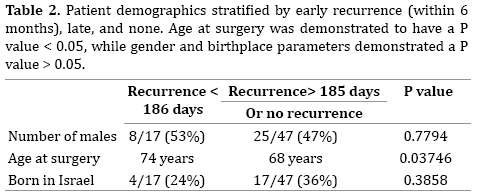
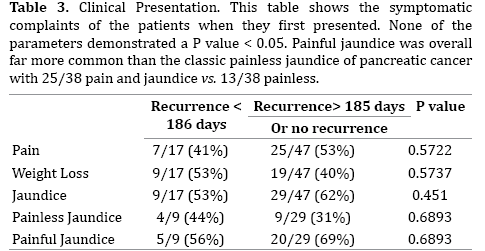
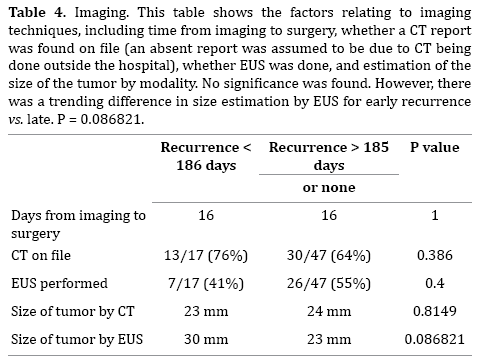
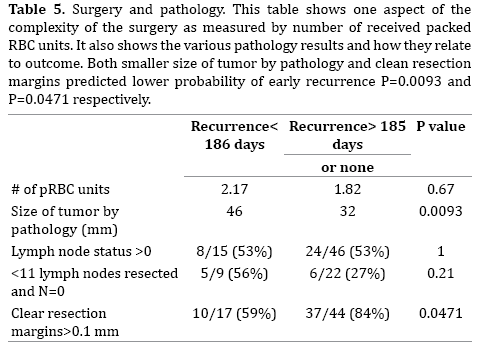
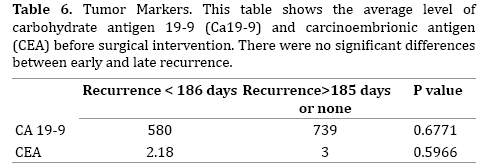
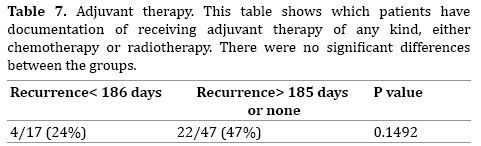
Age at surgery between early and late recurrence was significant (P-value= 0.03746), while birthplace and gender were not demonstrated to be statistically significant (Table 2). Presenting symptoms demonstrated no statistical significance, although it was found that a larger percentage of pancreatic cancer patients presented with painful jaundice as opposed to painless jaundice (Table 3). The difference in imaging modalities demonstrated no statistical significance with P-values < 0.05, but the use of EUS as an imaging modality with regards to tumor size was shown to have a P-value = 0.08682 (Table 4). Both smaller size of tumor by pathology and clean resection margins demonstrated lower probability of early recurrence P=0.0093 and P=0.0471 respectively (Table 5). None of the other findings with regards to other parameters chosen(tumor markers, adjuvant therapy, smoking) demonstrated statistically significant results (Tables 6, 7, 8).

DISCUSSION
In the general population, there seems to be a male predominance in incidence of pancreatic cancer (1.3:1). This predominance is mostly seen in younger patients and becomes more balanced in the elderly [13]. Although the population for this study was taken from consecutive eligible patients without gender bias, there were 33 males and 31 females, effectively no male predominance. Another interesting effect is the ethnic predominance of Jews vs. Arabs. Individuals of Ashkenazi Jewish descent have an increased risk of developing pancreatic cancer when compared to other populations (in this case Arab Israelis). This is due largely to genetic factors such as BRCA1, BRCA2, MSH, and others [14]. This study included 55 (86%) Jewish patients and 9 (14%) Arab patients, while the population in the area that Rambam serves is approximately 70% Jewish and 30% Arab [15] (P=0.0062).
Approximately 36% of the patients had recurrence within 6 months. The median time to recurrence excluding those who did not demonstrate recurrence yet was approximately 8 months, consistent with values found in the literature [8]. An open, multicenter, randomized control study on the efficacy of adjuvant therapy with gemcitabine found a median disease-free survival time for the control arm of the study to be 6.9 months (6.1-7.8) [16].
In terms of demographics, there were no significant differences found with gender or birthplace. However, the group of patients with early recurrence were significantly younger than those that recurred late. Most studies have not shown this difference [11]. A possible explanation for this could be the hesitancy to perform surgery on the older population, thereby being more conservative when selecting which patients would benefit from it.
There was no significance in the clinical presentation of the patient. The data for this was dependent on the thoroughness of documentation by the physicians that admitted the patients and therefore, it may not have been reflective of the actual symptoms of the patients. Of interest was the prevalence of painful jaundice (66% of jaundice) compared to painless jaundice (34%). Painless jaundice is often what jumps to mind when one thinks of symptoms of pancreatic tumors due to its specificity. However, as seen in this study, it is important to note that painful jaundice may be is a far more common presenting complaint.
While investigating the imaging techniques, there were difficulties locating many of the diagnostic CTs. Many patients were diagnosed outside of the hospital and therefore did not have their results on file. This did not seem to have any effect on their outcome. In terms of using EUS for diagnosis and staging, while other studies have shown that EUS significantly reduces futile surgeries [17], this study did not show the same results. This could possibly be due to small sample size, or alternatively, the results of EUS not being used effectively. Evidence for the latter would be the trend of larger tumor size (P=0.086821), as measured by EUS, of the tumors that recur earlier. It’s possible that the potential of EUS for discriminating between useful and futile surgeries exists but is not being fully utilized.
Many studies have already shown that the number of packed RBC units received, tumor size, lymph node status, total number of lymph nodes resected, tumor grade and resection margins correlate with survival and disease free survival [8, 11, 18]. This was demonstrated with significance in tumor size (P=0.0093) and resection margins (P=0.0471), but no correlations were found with the other parameters listed.
Several studies have shown significance of tumor markers, specifically CA19-9, in predicting early recurrence [19-21]. This was not seen in the results. In this center, very high CA19-9, over 1000, is considered as pointing towards likely inoperability, and thus neoadjuvant chemotherapy is particularly considered for such patients, with surgery to be reconsidered only after a course of neoadjuvant is shown to have been effective and that no new criteria of inoperability appear during the oncotherapy.
The recording of adjuvant therapy is reliant on the physician and many patients received therapy that was only recorded in handwriting. While the assumption was made that the recording of therapy was random and should not have affected the results, this could have been a reason for the failure to reproduce the results of previous studies that showed delay in recurrence with adjuvant therapy [22].
Our study has demonstrated a recurrence rate on par with other major and leading institutions (36% at 6 months, 50% at 8 months). It is important to continue to endeavor to reduce these values in order to provide the best possible care for patients. One strategy would be to accurately screen which patients will recur early and avoid operating on them. The results have shown that increased age at surgery, tumor size, and resection margins less than 0.1mm correlate to earlier recurrence. Unfortunately, the latter two are only obtained post surgery. However, if imaging techniques to accurately estimate tumor size can be improved, it should facilitate making more informed decisions. The results showed a promising trend with EUS tending to estimate tumors that recurred earlier as being larger. As further development occurs in imaging techniques, adjuvant and neoadjuvant therapies and the ability to decrease futile surgeries, it will lead to increasing both patients’ quantity and quality of life.
The authors declare that they have no competing interests.