- (2007) Volume 8, Issue 6
Damien Olivié1, Luigi Lepanto2, Jean Sébastien Billiard2, Pascale Audet2, Jessica Murphy Lavallée2
1Department of Radiology, University of Rennes Medical Centre. Rennes, France
2Department of Radiology, University of Montreal Medical Centre. Montréal, Québec, Canada
Received September 2nd, 2007 - Accepted September 28th, 2007
Context Computed tomography is widely used to pre-operatively evaluate patients with ductal carcinoma of the pancreas. Objective To prospectively evaluate the ability of multi-detector computed tomography to predict resectability of pancreatic head cancer. Patients Ninety-one consecutive patients (53 men, 38 women; mean age, 61 years) referred to our department with a diagnosis of cancer of the head of the pancreas underwent a preoperative contrast enhanced triphasic 16- slice multi-detector computed tomography. Sixty-three were considered inoperable because of advanced local disease, metastatic disease, or poor surgical risk. Intervention Of the remaining 28 patients, 23 underwent a Whipple procedure, whereas 5 patients underwent a palliative procedure. Main outcome measures Surgical and pathologic reports were reviewed and compared to CT results. Results Of the 91 patients evaluated, 25% had successful resection of pancreatic head carcinoma; while only 5% had a palliative procedure. When compared to surgical outcome, the positive predictive value of multi-detector computed tomography for resectability was 100%. On the basis of pathologic results, the positive predictive value of multi-detector computed tomography for resectability fell to 83%, Four patients deemed resectable following multi-detector computed tomography had positive margins at pathology. Conclusion The positive predictive value of multi-detector computed tomography for resectable disease is lower when pathologic correlation, as opposed to surgical correlation, is used as the gold standard. Compared to previous studies, there was a lower rate of palliative surgery in our cohort.
Carcinoma, Pancreatic Ductal; Pancreas; Pancreatic Neoplasms; Surgery; Tomography, Spiral Computed; Tomography, X-Ray Computed
HCT: helical computed tomography; MDCT: multi-detector computed tomography
Although pancreatic cancer accounts for only 2% of new cancers in the United States, it is the fourth leading cause of cancer deaths. It has an over-all 5-year survival rate of 4%, while localized cancers have a survival rate of 17% [1]. About 15 to 20% of patients have resectable disease at the time of presentation [2]. Surgical resection offers the only chance for cure with reported 5-year survival rates of 8% to 21% [3]. Tumors are considered unresectable when metastatic disease or local vascular invasion is present. The vessels most often involved are the celiac trunk, the hepatic artery, the superior mesenteric artery, as well as, the superior mesenteric vein and the portal vein [4, 5]. Contrast enhanced, helical computed tomography (HCT) and more recently multi-detector computed tomography (MDCT) have been widely accepted as the imaging technique of choice for the staging of pancreatic adenocarcinoma. Despite the advent of endoscopic ultrasound, computed tomography remains a mainstay of preoperative assessment [6, 7, 8]. The introduction of helical CT, less than a decade ago, improved our ability to appropriately stage disease; however, a significant number of patients are still incorrectly diagnosed as having resectable tumor on CT only to be unresectable at surgery. The proportion of patients undergoing unnecessary laparotomy may vary between 21% and 44% [5, 9, 10].
The purpose of this study is to evaluate, prospectively, the ability of MDCT to predict resectability of pancreatic cancer on the basis of surgical outcome and pathologic correlation.
Patients
Between February 2003 and June 2004, 91 consecutive patients (53 men, 38 women; mean age, 61 years; range, 36-83 years) referred to our department with a known or suspected diagnosis of cancer of the head of the pancreas underwent a preoperative contrast enhanced triphasic MDCT. Of the 91 patients, 63 (69.2%) were considered inoperable because of advanced local disease, metastatic disease, or poor surgical risk. The remaining 28 patients (30.8%) formed the basis for this study.
CT Technique
All examinations were performed with the same 16 slice CT scan (Light speed, General Electric Medical System, Milwaukee, WI, USA). Patients drank 500 mL of water to demarcate the duodenum and delineate the pancreatic head region. All patients received an intra-venous injection of 150 mL of Omnipaque® 350 (Amersham, GE Healthcare, Oakville, Ontario, Canada) at a rate of 4 ml/s. A triple-phase MDCT was then performed with a detector width of 0.625 mm, a section width of 2.5 mm and an interval reconstruction of 1.25 mm. The scan delay after the beginning of contrast infusion was 20 s for the arterial phase, 40 s for the late arterial phase, and 60 s for the portal phase. All images were interpreted on a picture archiving and communication system (PACS) workstation. Curved and multiplanar reformations were obtained at a dedicated post-processing workstation (Advantage® Windows 4.0, General Electric Medical System, Milwaukee, WI, USA). MDCT scans were analyzed prior to surgery to determine resectability.
Image Analysis
Axial images, as well as, curved and multiplanar reconstructions were reviewed. Radiological criteria of unresectability included: the presence of liver metastases, peritoneal carcinomatosis, tumor infiltration in contact with more than 180° of the circumference of the walls of major arteries (celiac trunk, hepatic artery, superior mesenteric artery) and involvement of more than 180° of the circumference of the portal vein or the superior mesenteric vein. This threshold has been shown to yield the best predictive values for resectability and unresectability [4, 5]. The MDCT findings were correlated with surgical outcomes to assess accuracy in predicting resectability. Also, the pathologic reports were reviewed to determine if the surgical margins were free of tumor.
The study protocol conforms to the ethical guidelines of the World Medical Association Declaration of Helsinki, as revised in Tokyo 2004, and was approved by our institutions Internal Review Board. Informed consent was obtained from each patient participating in the study.
The accuracy and the positive and negative predictive values for resectability of MDCT were calculated by using surgical outcome as a reference standard. The same parameters were also calculated by using pathologic findings, particularly the presence or absence of tumor infiltration at the surgical margins. Frequencies, mean and range were used as descriptive statistics.
The study group consisted of 28 patients. There were 14 men and 14 women, with average ages of 63 years (range 40-76 years). Twenty-three underwent a Whipple procedure, whereas 5 patients underwent a palliative procedure. The interval between MDCT and surgery was 22.4 days (range 3- 55 days). Surgical and pathologic reports were reviewed and compared to CT results. Correlation with surgical findings was available in 28 patients, whereas correlation with pathologic findings was available in 23 patients. The diameter of the lesions in these patients ranged from 1.2 to 3.6 cm. The average lesion diameter was 2.2 cm. Table 1 summarizes the correlation between MDCT findings, and surgical and pathologic findings. When compared to surgical outcome, the positive predictive value of MDCT for surgically resectable disease was 100% (23/23), and the negative predictive value i.e. (prediction of unresectability) was also 100% (5/5). Accuracy was 100% (28/28). Four of the 23 patients who underwent a Whipple procedure and were believed to be resectable on the basis of MDCT were found to have positive surgical margins at pathology. On the basis of pathologic results, therefore, the positive predictive value of MDCT for resectability fell to 82.6% (19/23). Two of the 4 patients with positive margins had infiltration of the root of the mesentery and tissue abutting the superior mesenteric artery. In both cases, less than 180° of the vessel circumference was involved. Follow-up scans obtained within 4 months of surgery in both these patients showed local recurrence of tumor (Figure 1).
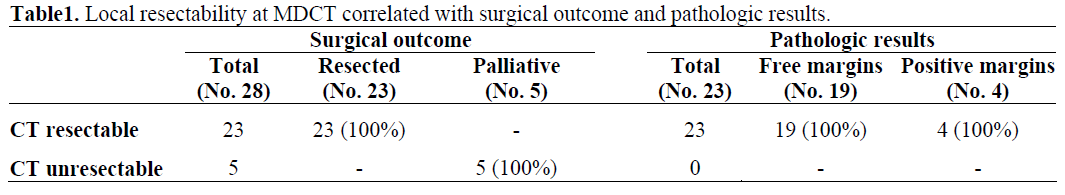
Figure 1. Adenocarcinoma of the head of the pancreas in a 71-year-old man. a. Arterial phase, transverse MDCT image, obtained during pre-operative staging, shows tumor infiltration (arrow) abutting the posterior wall of the superior mesenteric artery (arrowhead). b. Portal phase, transverse image MDCT, shows tumor recurrence (arrow) at the site of previous surgery, near surgical clips (arrowhead).
The accurate determination of resectability in patients with pancreatic cancer is the most important contribution of pre-operative staging; the goal being to reduce needless surgery to a minimum. Laparotomy in patients with pancreatic cancer carries significant perioperative morbidity (20-30%), even in expert hands [11]. Moreover, prognosis is not improved for patients whose tumors are resected with positive margins or vascular invasion [12, 13]. On the other hand, for most patients with unresectable lesions, laparotomy for palliative procedures has become unnecessary because of recent advances in endoscopic and percutaneous methods of biliary and duodenal decompression.
The improvement in CT technology has been paralleled by an improvement in the ability of CT to predict resectability. In a meta-analysis, Bipat et al. found a sensitivity and specificity of HCT for determining resectability of 81% and 82%, respectively [14]. This represented a significant improvement over conventional CT. Predictive values of HCT for resectability ranging from 56% to 79% have been reported [5, 9, 10, 15, 16]. Most of these studies reported better results when predicting unresectability, with predictive values ranging from 96% to 100%. Only Phoa et al. found a predictive value for unresectability of 57%, well below that found by other investigators [16]. In a recent study evaluating the ability of MDCT to detect resectability, Vargas et al. reported a predictive value for resectability of 87% [17]. This represents a further improvement over HCT. Our results show a predictive value of 100% for resectability when compared to surgical outcome. The rate of patients who underwent resection of pancreatic adenocarcinoma was higher in our study; in fact, only 5% of all patients evaluated by MDCT in our study eventually had a palliative surgical procedure. With so few patients deemed unresectable on the basis of MDCT submitted to surgery, it is difficult to evaluate the predictive value for unresectability.
Comparing CT results to pathologic findings modifies the results somewhat. When the absence of positive margins is considered the requirement for successful resection, the positive predictive value of MDCT for resectability fell to 83%. Similarly, Phoa et al. also showed an increase in the predictive value for unresectability (from 57% to 82%) and a decrease in the predictive value for resectability (from 72% to 50%), when pathologic, rather than surgical, correlation was considered [16].
The proportion of patients submitted to surgery whose pancreatic adenocarcinoma was successfully resected was 82% in our series. In the series reported by Vargas et al., the resection rate was 80% [17]. The advent of MDCT has seen an increase in the rate of successful resection of pancreatic cancer in patients submitted to surgery. In previously published series using HCT, the resection rate varied between 28% and 73.5% [5, 9, 10, 15]. In the study published by Phoa et al., using a twin detector HCT, the resection rate was 57% [16].
Our study does present some limitations. No instances of small liver metastases were seen at laparotomy in cases with CT resectable disease. There is no clear explanation for this; possibly, the detection of early local invasion such as infiltration surrounding the superior mesenteric artery and accompanying infiltration of the root of the mesentery, precede peritoneal seeding and small liver metastases. Also, a detailed analysis of why 63 of 91 patients initially assessed were deemed inoperable was not carried out, because there is no way to correlate the CT findings with accurate staging. However, the 19 patients who had their cancers successfully resected, in our study, represented 21% of all patients initially evaluated. This correlates well with findings in the literature, reporting that only 15 to 20% of patients have resectable disease at the time of presentation [2]. In our institution, venous resection is not routinely performed during Whipple procedure. This technique is used in certain centers and thus the criteria for resectability will necessarily differ from the ones used in our study.
In conclusion, there is improved prediction of resectability and unresectability with the introduction of MDCT. When compared to HCT studies, there is a rise in the rate of successful surgical resection with a concomitant decrease in the rate of palliative surgery, leading to a difficulty in measuring the predictive value of unresectability since fewer patients with unresectable disease undergo laparotomy.