Original Article - (2017) Volume 18, Issue 6
M Bassir A Fakhree, Abdolreza Mehdinavaz Aghdam, Farshad Mahdavi, Ramin Azhough, Alireza Omidi
Department of General Surgery, Tabriz University of Medical Sciences, Tabriz, Iran
Received Date: September 15th, 2017; Accepted Date: November 27th, 2017;
Background and purpose Patients with severe acute pancreatitis are at risk of complications such as sepsis and organ failure that cause significant morbidity and mortality. In current clinical trial, we aimed to evaluate feasibility of plasmapheresis in treatment of severe acute pancreatitis. Materials and methods In this phase 1 clinical trial, twenty patients with severe acute pancreatitis (Ranson’s score ≥ 7) were enrolled. Patients admitted to intensive care unit and standard pancreatitis treatment including bowel rest and intravenous fluid administration started. Subsequently, all patients underwent plasmapheresis up to three sessions every other day, with 2 units of fresh frozen plasma. Results Of twenty patients, 10 (50%) patients were male. The underlying etiology for pancreatitis was recognized to be cholelithiasis in 17 (85%) patients and hypertriglyceridemia in 3 (15%) patients. Eighteen patients presented with abdominal pain that resolved after plasmapheresis (P<0.0001). Fever was reported in 9 patients, resolved in all patients subsequent to plasmapheresis (P=0.001). Adult respiratory distress syndrome was found in 7 patients. All patients recovered subsequent to plasmapheresis (P=0.004). None of the patients died, or suffered plasmapheresis or catheter related complications. Mean length of hospital stay was 10.625 days, and mean intensive care unit length of stay was 5.75. Conclusion Plasmapheresis is a safe modality in treatment of patients with severe acute pancreatitis. It can be used to improve clinical status and patient outcome, although randomized trials are necessary to establish its efficacy.
Pancreatitis; Plasmapheresis; Respiratory Distress Syndrome, Adult
ARDS adult respiratory distress syndrome; FFP fresh frozen plasma; ICU Intensive care unit; ICU LOS intensive care unit length of stay
Acute pancreatitis is a common disease that may lead to serious conditions associated with considerable morbidity and mortality [1]. Severe acute pancreatitis (SAP) will develop in 20% of the patients with acute pancreatitis that may result in pancreatic necrosis, serious organ failures and increased rate of morbidity and mortality [2, 3, 4]. Several etiological factors have been described for acute pancreatitis, including alcohol consumption, biliary tract disorders (e.g. gallstones), endoscopic retrograde cholangiopancreatography, trauma, infection and hyperlipidemia [5, 6, 7].
SAP clinical course is comprised of pro-inflammatory and anti-inflammatory phases. Pro-inflammatory response phase leads to systemic inflammatory response syndrome (SIRS) and subsequent early multisystem organ failure (MOF) [3, 8, 9]. Although clinical signs and symptoms are key features of SAP, laboratory tests and less frequently diagnostic imaging are needed to approve diagnosis [10].
Prompt diagnosis and treatment are of considerable importance in patients suffering severe acute pancreatitis to prevent life-threatening conditions and achieving optimal outcomes. Regardless of primary etiology and underlying factors, primary treatment of SAP includes fluid resuscitation, pain control and further supportive care such as bowel rest and fasting [11, 12]. Nonetheless, management of these patients depends on the severity of acute pancreatitis, so that SAP cases require transfer to intensive care unit.
Considering its established role in treatment of familial hypercholesterolemia, plasmapheresis was first introduced in 1980s to provide satisfying outcomes in treatment of patients with severe acute pancreatitis due to hyperlipidemia by improving both symptoms and laboratory findings [12]. Plasmapheresis consists of replacement of patient’s plasma subsequent to its removal via filtration, which results in inflammation reduction by decreasing triglyceride levels and supplementation of protease and lipase with the intact fresh frozen plasma (FFP) [11, 13].
There are several case reports and case series in the literature reporting the beneficiary of plasmapheresis in treatment of severe acute pancreatitis and recurrent pancreatitis due to hypertriglyceridemia, however, there is lack of known trials and reviews evaluating its advantages and disadvantages on AP regardless of etiology [14, 15, 16]. Therefore, in current phase I clinical trial, we aimed to determine feasibility of plasmapheresis in treatment of patients with severe acute pancreatitis.
An experimental phase I controlled trial carried out between March 2014 and December 2014 in general surgery ward, Imam Reza hospital, Tabriz University of Medical Sciences. The study was approved by ethics committee of the Vice Chancellor of Research and Development, Tabriz University of Medical Sciences (Approval No: 5/4/10443), and registered in Iranian Registry of Clinical Trials (primary registry in the WHO registry network) (www.irct.ir, ID No: IRCT201411084456N1). Considering indeterminate population and based on previous studies, using Morgan table, study population calculated to include 20 patients with severe acute pancreatitis.
Patients with AP diagnosis who had Ranson scores ≥ 7, enrolled in this study (scores computed using online Ranson Criteria in Acute Pancreatitis, www.globalrph.com/ranson.htm) (Figure 1). Patients who had undergone any kind of surgeries and patients with cardiovascular diseases were excluded, as well as patients suffering coagulopathies. Written informed consent was obtained from all patients participating in the study.
Demographic data (including patients’ age and gender) were recorded. Subsequent to admission to intensive care unit (ICU), bowel rest started for all patients and nasogastric tube inserted. Fluid resuscitation, pain control by intravenous analgesics and empiric broad spectrum antibiotics administered. Furthermore, dialysis catheter was placed through internal jugular vein in order to acquire central venous access, and patients underwent plasmapheresis (exchanged with 2 units of ISO-group FFP) every other day, up to three sessions consecutively, based on attending physician decision. Plasmapheresis stopped right after pancreatitis clinical manifestations recovered.
Probable plasmapheresis side effects, clinical findings, pancreatitis complications, presence of end organ failure (including ARDS), inpatient death, ICU length of stay and hospital length of stay were recorded.
Statistical Analysis
The Chi-square Test used for comparing two qualitative variables. The level of significance was set at 0.05 and all results were expressed by frequency (percent) for qualitative variables and Mean±SE for quantitative variables.
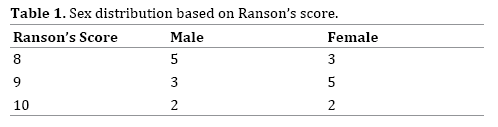
In current study, 20 patients enrolled suffering severe pancreatitis (Ranson score ≥ 7). Of twenty patients, 10 (50%) were female and 10 (50%) were male. Patients mean age was 64.75±19.10, whereas the youngest and the oldest patients were 23 and 87 years old (Table 1). The underlying etiology for pancreatitis was recognized to be cholelithiasis in 17 patients (85%) and hypertriglyceridemia in 3 patients (15%). In addition, one of the patients with underlying hypertriglyceridemia was pregnant.
In terms of presenting symptoms, 18 (90%) had severe abdominal pain that resolved in all patients subsequent to plasmapheresis, showing a statistically significant recovery with plasmapheresis (P<0.0001).
Fever detected in 9 patients (45%) initially. After plasmapheresis, fever resolved in all suffering patients (P=0.001). Acute respiratory distress syndrome (ARDS) detected in 7 patients (35%). However, after plasmapheresis, ARDS resolved in all patients (P=0.004).
Three patients (15%) presented with urticaria prior to plasmapheresis. Although urticaria recovered in two patients (10%) following plasmapheresis, there was no significant correlation between plasmapheresis and urticaria healing in these patients (P=0.5).
Mean hospital length of stay was 10.62±3.03 (ranged between 7 to 17 days), and mean ICU admission duration was 5.75±3.75. None of the patients died during this study. No adverse events subsequent to plasmapheresis, such as hemodynamic abnormalities, were reported in patients. No catheter related complications such as pneumothorax were noticed.
Acute pancreatitis may develop due to disturbances in factors affecting cellular hemostasis, according to recent studies [5, 6, 17]. Although, several factors such as alcohol consumption and gallstones, have been recognized to play role in onset of acute pancreatitis, exact pathophysiology of the disease is still unclear [7, 10]. Considering importance of early treatment in AP management, several treatment strategies such as peritoneal lavage and plasmapheresis have been introduced to improve outcomes [18, 19]. Since inflammatory mediators have been suggested to be associated with acute pancreatitis severity, elimination of these factors via plasmapheresis may lead to increased recovery rate and decreased morbidity and mortality [14, 20].
In present study, twenty patients presenting with severe AP with Ranson’s score of greater than or equal to 7, were enrolled in and underwent plasmapheresis. Abdominal pain and fever were the most prevalent symptoms that resolved in all patients subsequent to plasmapheresis. All patients suffering ARDS recovered from symptoms following plasmapheresis sessions. Our results showed significant correlation between plasmapheresis and recovery of acute pancreatitis common symptoms and associated syndromes. However, there were no correlation between plasmapheresis and urticaria healing in suffered patients. No mortality and adverse events reported in these patients.
According to the literature, our study is one of the first phase I studies dedicated to plasmapheresis in treatment of acute pancreatitis, regardless of underlying etiology. Previous reports mostly include case presentations limited to hypertriglyceridemia as the underlying reason, which may be due to proven efficiency of plasmapheresis in treatment of hypertriglyceridemia. Similar to other studies, we suggest plasmapheresis to be helpful in patients with severe acute pancreatitis immediately after admission to intensive care unit and routine medical management.
In a report by Kohli et al. they reported a case with acute pancreatitis caused by hypertriglyceridemia presented by mild fever and epigastric tenderness with a mild leukocytosis and severe hypertriglyceridemia in laboratory tests [1]. Despite routine care, patient’s overall condition turned out to worsen during admission, followed by developing multi-organ failure including anuric acute renal failure and ARDS. Subsequently, patient underwent three sessions of plasmapheresis in three consecutive days that completely improved patient’s symptoms, organ failure and hemodynamic instability. In our report, patients underwent plasmapheresis right after patients kept NPO and fluid resuscitation started, however, organ failure developed in some patients due to rapid progression of the inflammation and severity of AP. Similar to Kohli’s report, patients’ symptoms including abdominal pain and fever resolved followed by plasmapheresis administration in our study. In addition, ARDS developed in 7 patients that completely recovered after plasmapheresis sessions.
In a case series by Kyriakidis et al. five male patients suffering hyperlipidemia induced acute pancreatitis (Ranson score between 4 and 7) were enrolled and treated by plasmapheresis, in addition to standard treatment [21]. They reported significant improvement in patients’ abdominal pain and other signs and symptoms. The authors did not report any organ failure, complications or mortality. Despite Kyriakidis study, we evaluated patients with severe acute pancreatitis (Ranson’s score ≥7). Similarly, approximately all sign and symptoms improved after plasmapheresis in our patients, and no plasmapheresis induced complication and mortality reported and none of the patients needed surgical intervention.
We performed plasmapheresis whenever the acute pancreatitis diagnosis has been made, as a supplement to standard pancreatitis treatment and detected significant improvement in clinical status, signs and symptoms of the patients. However, Bhavsar suggested plasmapheresis to be effective only in patients with hyperlipidemic acute pancreatitis [22]. It seems our study is the very first report in to evaluate plasmapheresis in patients who suffered AP due to gallstones.
In a study by Syed et al. of four patients with severe hyperlipidemic acute pancreatitis, two patients received early plasmapheresis [16]. Serum triglyceride levels improved significantly in patients who received plasmapheresis, in comparison to standard treatment patients. In addition, they reported no significant difference in terms of ICU and hospital stay, as well as incidence of secondary complications. Similarly, our results showed no serious complication or mortality in SAP patients, who received plasmapheresis treatment. Although, it was impossible to evaluate plasmapheresis efficacy in absence of standard SAP management group, we believe plasmapheresis may lead to rapid improvement in SAP victims, while preventing secondary complications. It can be estimated that secondary complications are in correlation with severity of pancreatic inflammation. Thus, with due attention to study by Kohli et al. standard treatment followed by wait and watch treatment can develop life-threatening complications including multiorgan failure and severe unstable clinical status. Therefore, we hypothesize that early plasmapheresis can prevent progression of inflammation and decrease incidence of life-threatening conditions [1].
Our study had some limitations. As a phase one clinical trial, there was no control group so the efficacy of plasmapheresis versus standard treatment cannot be determined. In addition, due to small patient population size, there were no catheter and plasmapheresis complications. Obviously these complications occur when population size increases. Furthermore, number and frequency of plasmapheresis in these patients was chosen arbitrarily and refined protocols need to be established.
There was another limitation in this study. In our population in Iran alcohol consumption is relatively scarce, thus alcohol induced AP is not encountered so often. So we had no severe AP patient due to alcohol consumption in this patient population.
We suggest that plasmapheresis can be done in severe acute pancreatitis patients regardless of its etiology with acceptable complication rate. However further randomized clinical trials must be done to determine its efficacy and complications.
The authors declare that they have no conflict of interest.