Research Article - (2016) Volume 24, Issue 5
Ornelas MD*
Medical Specialist in General Practice and Family Medicine at SESARAM, E.P.E.; PhD Student at NOVA Medical School of Lisbon / FCM – UNL, Portugal
Pais D
Professor at NOVA Medical School of Lisbon / FCM – UNL; MD, Portugal
Sousa P
Professor at National School of Public Health– UNL; Centro de Investigação em Saúde Pública da Universidade Nova de Lisboa (UNL), Portugal
Corresponding Author:
Ornelas Marta Dora
Medical Specialist in General Practice and Family Medicine
PhD Student at NOVA Medical School of Lisbon - FCM – UNL, Portugal
Tel: +351 291782220
Travessa do Tanque 11 Monte, 9050-427 Funchal/Portugal
E-mail: phdmarta@gmail.com
Submitted date: August 25, 2016; Accepted date: September 15, 2016; Published date: September 22, 2016
Introduction: According to the European Commission more than 37 million Primary Healthcare (PHC) users suffer Adverse Events (AE). When we talk about these unintentional and undesirable events, most of the time we are dealing with acts committed by competent and dedicated professionals, who often work in disorganized systems, and who are not very oriented towards patient safety and health care professional safety. The adoption of a safety culture is a proven useful tool to make AE less likely to occur and to minimize its consequences when these inevitably take place.
Methods: The authors describe some pertinent issues that have made the evaluation of AE and Patient Safety Culture (PSC) in Portuguese PHC particularly challenging and describe the preliminary results of a project for the assessment of PSC using the Medical Office Survey on Patient Safety Culture (MOSOPSC). This instrument has been translated, adapted and validated by the authors for the study population.
Results: Studies about AE in PHC are scarce, but admittedly necessary. Despite the socio-economic instability experienced in Portugal, the preliminary results obtained by the authors promise a proactive PSC with dedicated health professionals, working as a team and recognizing the problem of adverse events in PHC of the Madeira Island.
Discussion: The concepts and methodologies used in other studies cannot simply be applied to specific populations. On the Madeira Island (one autonomous region of Portugal), the issue of patient safety (PS) is difficult to approach but, nevertheless, with information and discussion it was possible to measure the PSC in PHC.
Conclusion: After some adjustments, the MOSOPSC questionnaire, in addition to assessing safety culture, has helped to initiate the dialogue and discussion on the issue of PS among the various professionals. This approach has allowed these professionals to anticipate and prevent the occurrence of AE and, whenever such is not possible, notify, discuss, share and learn from those same events.
Keywords
Adverse events; Patient safety; Patient safety culture; Primary health care; Safety management
Introduction
With the publication of "To Err is Human: Building a Safer Health System" [1] and several other studies, such as the Harvard Medical Practice Study, the issues of patient safety (PS) and Adverse Events (AE) (which attracts more media attention) were brought into the limelight and subjected to public opinion.
In spite of being the basis of the evolution and progression of medical innovation, the modern healthcare system also involves (and thankfully in a much smaller scale) the occurrence of AE – a major source of morbidity, mortality and resource consumption (one AE can represent economic costs exceeding USD 3,633.64). [2]
Numerous efforts have been made in order to understand the nature and magnitude of AE and to propose appropriate solutions. Most of this activity has been focused on hospital settings where the activities are more standardized, complex and with higher risk.
Based on a retrospective review of hospital records, we already know that 31% of the AE identified during hospitalization have occurred in earlier levels of care, probably in the PHC. [3] This fact can be justified by the increasing technical and scientific capacity of these professionals and their ability to perform medical acts that were once performed only in hospitals.
The incidence of AE in hospitals reach values between 3.7% and 16.6% and 40% to 70% of these are considered preventable. In Portugal, a pilot study in hospitals [4] show us an incidence rate of AE of 11.1%. Such studies are scarce in Primary Health Care (PHC) but we can estimate an incidence of AE ranging between 0.0004% and 24% and, similarly to what happens in hospital, 45% to 76% are considered to be preventable.
The results found in PHC may give the impression of lowrisk. However, if we take into account the fact that this incidence is still undervalued (it only represents the reported, remembered, recognized and/or analysed incidents) and the volume of visits to primary care centers (over 25 million consultations were performed in Portuguese PHC in 2012, representing 69% of all consultations performed in the National Health System (NHS) during that year), [5] this problem becomes an issue that requires the immediate intervention of national and international policy-makers.
As the first point of contact for individuals, family and the general community, the PHC brings healthcare as close as possible to where people live and work, offering a more personal and longer-term care, being the key point for the design of effective preventive strategies. Its high rate of users associated with a set of circumstances that involves an increased risk of AE (multiple chronic pathologies, users over 65 years of age, polymedicated and living in problematic psychosocial contexts) places AE in PHC as a real public health problem.
In Portugal, Family Practitioners (FP) act as gatekeepers to hospital care and are responsible for family planning, follow-up on child development, surveillance of low-risk pregnancies, chronic disease management and care of the elderly. Most general practices have 5-10 FP working in a group and most doctors care for a list of 1,500–1,900 patients. [6]
The Madeira Island is an autonomous region of Portugal with about 270,000 inhabitants. It has a regional health care service - SESARAM, E.P.E (two hospitals with all specialties and about 45 Personalised Health Care Units) that is an integral part of the NHS.
The PHC Activity Monitor for Europe (PHAMEU) project has evaluated the Portuguese PHC at a relatively strong level of care (similar to what happens in other countries like the UK, Denmark, the Netherlands and Spain). [7] However, WHO’s Safer Primary Care Expert Working Group [8] considers that despite the fact that the national health system has progressed significantly over the years (this progress reflects on better health care indicators, like life expectancy and child mortality), evidence concerning the quality and safety of services is lacking, and information about AE is currently very limited and difficult to access.
In fact, the National Reporting System of Incident and Adverse Events (NOTIFIQ@) covers all levels of care; but even with the efforts made by the Directorate-General of Health (DGS) and readjustments to the notification platform, the total number of notifications is far from reflecting the national reality (1,675 notifications from health professionals and 159 notifications from citizens since the beginning of the system (2013) until the end of 2015. [9]
According to Milligan [10], there is no use in trying to implement measures that encourage good practice (and hence reduce the occurrence of AE) if the professionals who make up the organizations are not particularly aware of PS and the education of patients, families, healthcare professionals, administrators, managers and policy makers is not a priority and point of approach, reflection and standardization of concepts.
We know that even the perception of occurrence of these events by health professionals varies according to the safety culture present in their workplaces and, therefore, both WHO and the Council of the European Union recommend the evaluation of this culture - "product of values, attitudes, skills and individual behavior patterns and group, which determine the commitment, style and proficiency administering a safe and healthy care”, [11] as an essential condition for the introduction of changes in the behavior of professionals and health care organizations.
For the assessment of PS culture (both in hospital and PHC) there are essentially two types of approaches: a qualitative approach (through multidisciplinary meetings, interviews, observation methods, audits or document analysis) and a quantitative approach (through self-completed questionnaires).
Our objectives are to (i) assess PSC in the PHC of the Madeira Island through the translation, adaptation, application and validation of the "Medical Office Survey on Patient Safety Culture" (MOSOPSC) [12] questionnaire; (ii) identify strengths and areas for improvement; (iii) create PS awareness among PHC professionals; and (iv) contribute to the first strategic objective of the Portuguese Plan for Patient Safety ("increase the safety culture of the internal environment"), and to PS in general and in PHC in particular.
Methods
The authors describe one quantitative, descriptive, cross-sectional, observational study with an analytical component through the translation, adaptation and application of MOSOPSC questionnaire to assess PSC in PHC of the Madeira Island. In order to obtain more reliable and accurate results, the process was performed in five steps: original version translation, conceptual equivalence evaluation, acceptability and viability assessment, content validity and questionnaire test and response analysis and psychometric properties assessment. The internal consistencies of the subscales were examined using Cronbach’s alpha (an alpha larger than 0.6 was considered acceptable), indicating that different items measure the same concept.
The MOSOPSC is a self-administration and multidimensional questionnaire (12 dimensions) with 51 questions; it is presented in the form of Likert scale, graduated in 5 levels for the 51 items, ranging from "strongly disagree" or "never"=1, to "strongly agree" or "always"=5; there is also the option "not applicable or do not know". The dimensions discussed are the following: (i) opening to communicate; (ii) communication on the error; (iii) transmission of information to other services; (iv) organizational learning; (v) general perceptions on PS and quality; (vi) support by the managers; (vii) provision and continuity of care; (viii) safety and quality; (ix) team training; and (x) teamwork and pressure/amount of work. In addition, the medical office survey includes three items about respondent background characteristics and two overall rating questions.
For positively worded items with 5-point response scales, percent positive response is the combined percentage of respondents within a medical office who answered “Strongly agree” or “Agree,” or “Always” or “Most of the time,” depending on the response categories used for the item. For negatively worded items, percent positive response is the combined percentage of respondents within a medical office who answered “Strongly disagree” or “Disagree,” or “Never” or “Rarely,” as a negative answer on a negatively worded item indicates a positive response. Percent positive scores for the “PS and quality issues items”, and “Information exchange with other settings” items, were calculated by the sum of the three response options that represent the smallest frequency of occurrence (not in the past 12 months, once or twice in the past 12 months, and more than three times in the past 12 months).
Using a non-probability sampling (random/voluntary) the authors requested, via web and personally, the participation of about 1,000 professionals of 45 PHC centers achieved by completion of the questionnaire (accessed through a link). Each professional fills out the questionnaire only once. To reduce the frequency of missing answers the questions in the questionnaire were appearing as the answers were given.
The questionnaire was applied (between February and May 2016) to health care providers (medical specialists, doctors in training, nurses, operating and technical assistants, nutritionists, social workers and psychologists). An exclusion criterion was applied to PHC centers with under three careers or less than five participants, participants with less than a month of experience, and completed questionnaires with more than five missing answers.
The results were analyzed with the use of SPSS 18.0 for Windows.
Results
During the period under study (four months) we obtained 802 questionnaires; 319 of these were incomplete (more than five missing answers) and 483 were valid questionnaires.
The last two dimensions of Madeira Island MOSPSC (“information exchange with other settings”, and “PS and quality issues”) were deleted because of the high response rate of non-applicability (58 and 43% respectively).
The 10 reliability dimensions expressed as Cronbach’s alpha for the Madeira Island MOSOPSC ranged from 0.52 to 0.88 (Table 1). The lowest values of Cronbach alpha were observed in the questions related with leadership support and overall perceptions of PS and quality.
`
| Patient Safety Culture Composites/Dimensions | % Positive Response Madeira/(AHRQ) | Αlpha Cronbach Madeira/(AHRQ) |
|---|---|---|
| Teamworka | 81 (87) | 0.64 (0.83) |
| Organizational Learninga | 67 (80) | 0.58 (0.82) |
| Overall Perceptions of PS and Qualitya | 66 (80) | 0.54 (0.79) |
| Patient Care Tracking/Follow-upa | 62 (86) | 0.75 (0.78) |
| Staff Traininga | 61 (75) | 0.63 (0.80) |
| Office Processes and Standardizationa | 57 (69) | 0.65 (0.77) |
| Communication About Errora | 52 (71) | 0.75 (0.75) |
| Communication Opennessa | 47 (69) | 0.76 (0.81) |
| Owner/Leadership Support for PSa | 45 (69) | 0.52 (0.76) |
| List of PS and Quality Issues | 39 (86) | 0.88 (0.86) |
| Information Exchange With Other Settings | 25 (82) | 0.78 (0.90) |
| Work Pressure and Pacea | 25 (50) | 0.65 (0.76) |
Table 1: Percent positive response of items and dimensions and Cronbach`s alpha values for Madeira Island MOSOPC and 2016 database medical offices (AHRQ).
Madeira MOSOPSC is data obtained from 483 respondents; AHRQ Benchmark is data obtained from 25127 respondents [12]
aSafety Culture Dimension
PS: Patient Safety
The valid questionnaire represents a participation rate of 52%. The top three staff positions of respondents were Nurses (44.7%), Clinical support staff (16%) and Administrative staff (15%). Most healthcare professionals (69%) were aged between 31 and 50 years, worked 33-40 h a week (85%) and had been working for 11 or more years in the same service (42%).
In PHC of the Madeira Island, despite the fact that the majority of the professionals (53%) consider that representatives of organizations "are not investing enough resources to improve the quality of care" in their offices and there is a work overload (72%), the assessed safety culture is good, the health care is equitable (81%), effective (73%), patient-centered (60%), efficient (60%) and timely (55%) (Figure 1). Professionals receive appropriate training (61%) and work in teams (81%).
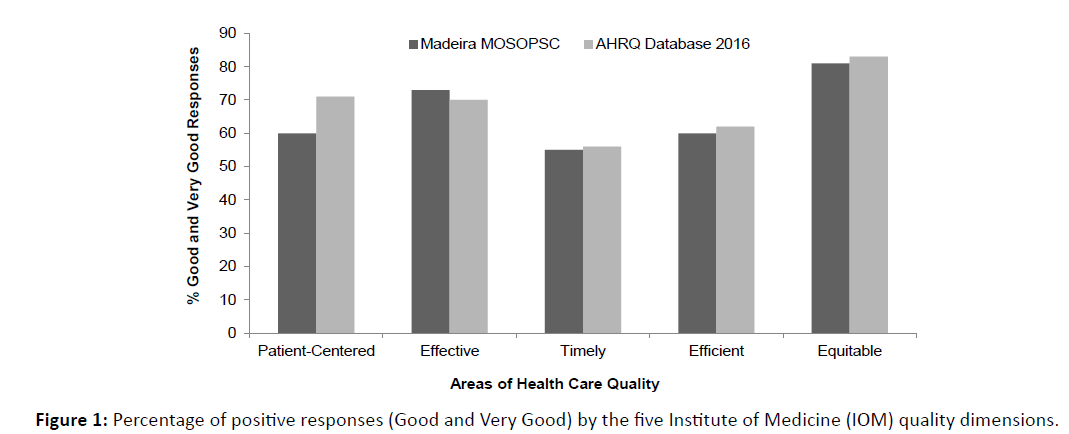
Figure 1: Percentage of positive responses (Good and Very Good) by the five Institute of Medicine (IOM) quality dimensions.
Although 21% of professionals refer that weekly the “medical equipment was not working properly or was in need of repair or replacement”, the majority of professionals disagree/strongly disagree with the expressions that “Mistakes happen more than they should in this office” (63%) and “It is just by chance that we do not make more mistakes that affect our patients” (70%).
Discussion
Studies of AE in PHC are still in early stages and, as far as Portugal is concerned, there have been many threats making this a particularly challenging issue.
As from 2011, DGS has been performing the evaluation of Patient Safety Culture (PSC) in hospital care, and recently (March 2016) has started this approach in PHC (in the context of the National Plan for Patient Safety). [13]
Unlike what happens on mainland Portugal, the Madeira PHC are only composed by classic general practices called Personalized Health Care Units and Family Health Units (FHU) have not yet been implemented, which is a logistic/manner of working a bit differently. FHU are formed by voluntary associations of physicians and the salary on these units is fee-for service and pay-for-performance bonuses,6 which can have an effect on the dynamics of teams and, consequently, on PSC in this type of health care organizations. For this reason, and the fact that this island did not participate in the project of DGS, the authors had to translate, adapt and validate the MOSOPS for PHC of the Autonomous Region of Madeira. In this process the authors faced particularly challenging issues, among them, we highlight:
– When other studies mention “primary care”, “ambulatory care”, “outpatients”, they may be referring to outpatient care delivered, which is part of hospital care programmes. This is completely different in Portugal, where apart from quaternary and tertiary healthcare, there is PHC (Personalized Health Care Units and FHU) and secondary healthcare (acute care);
– Many existing studies conducted in “medical offices” are not produced in what we consider to be public health systems, as the studies are mostly concerned with care delivered in “private” systems or in the framework of insurance schemes. The fact that care is delivered free of charge may impact the rate of use of the former services;
– Many health systems, in addition to "our" basic team providing PHC (family practitioners, nurses and administrative staff), also include paediatricians, dentists and pharmacists, which account for operating logistics different from the those we are used to observe in Portugal;
By the grounds displayed above and because of the heterogeneity in applied questionnaires and the reporting of outcomes, real comparison with other studies on perceived safety culture in primary care was difficult. For example, a comparison with AHRQ database immediately raises important questions, particularly the difference in the number of completed questionnaires (483 in Madeira MOSOPSC vs 25,127 in AHRQ 2016 database) and the time spent on collecting data (4 months on Madeira vs. 2 years in AHRQ). Taking this into consideration, we can state that the average medical office response rate on Madeira Island is lower than that found in U.S. Medical Offices (52 percent vs. 68 in AHRQ), however, the participation rate in this study is higher than that in hospital care on mainland Portugal (18%) and other international studies with similar methodology. [14,15] The 10 reliability dimensions expressed as Cronbach’s alpha for the Madeira Island MOSOPSC ranged from 0.52 to 0.88 (Table 1), which is lower than that reached by the 2016 AHRQ database (ranging from 0.75 to 0.90), leading one to infer that the consistency of the responses on each survey item for the data in this study is low if compared with the AHRQ data. The subscales inter correlated moderately, except for the factor about leadership support for PS and overall perceptions of PS quality.
The professionals have the perception that PHC on Madeira Island is more effective (when compared to the USA), but not as timely, efficient, equitable and patient-centered. Patient-centered health care is the dimension that differ the most from that observed by AHRQ.
Despite the good team work and respect for others, there are heavy workloads and problems with medical equipment. An issue that needs to be attended and quickly resolved.
Although nurses were the professional class with the highest answer rate (45%), when the number is adjusted to the number of health professionals on Madeira, doctors become the professional class with the highest participation rate (54.9%). This high participation rate of doctors is probably justified by the peer work performed by the doctoral student, who is a family practitioner on this island, in order to disseminate awareness of the questionnaire being carried out.
Madeira Island PHC has the following two areas of strength: “Teamwork” (81 percent positive) and “Organizational Learning” (67%).
Areas with potential for improvement for most of Madeira’s medical offices are: “Work Pressure and Pace” (25 percent positive) and “Ownership/Leadership Support for PS” (45%).
Although “list of PS and quality issues”, “information exchange with other settings” and “patient care tracking/follow-up” have a Cronbach’s alpha higher than 0.75, there was a large percentage of answers with “not applicable or do not know”. The exclusion of possible causes related to bad formulation/understanding of these questions may show some discomfort from the part of health professionals when tackling those questions.
Conclusion
For “the prevention of harm to patients” the emphasis must be placed on the system of care delivery that (i) prevents errors; (ii) learns from the errors that do occur; and (iii) is built on a culture of safety that involves health care professionals, organizations, and patients. Patients must be able to read, understand, evaluate and use health information effectively in order to be involved and truly contribute to the improvement of the quality of health care services and therefore, the reduction of medical errors. Their lack of understanding (poor health literacy) can contribute to failures in healthcare and, in turn, may represent a risk to PS. [16,17]
On the Madeira Island, the PS issue is difficult to approach but with information and discussion it was possible to measure the PSC in PHC. Despite the economic crisis experienced in Portugal, the preliminary results obtained by the researchers of this article promise a proactive safety culture with dedicated health professionals, working as a team and recognizing the problem of AE and the need for more human and material support in this level of care.
Nevertheless, the PS and quality rating, information exchange and work pressure were fairly low. Implementation of a safety and quality management system on Madeira island primary care setting is paramount. Further research is needed to improve the Madeira MOSPSC questionnaire for regional PHC. This project was the first step in approaching PS issue on Madeira Island; With knowledge of this PSC, the authors began the quantification and analysis of AE in Portuguese PHC with the application of APEAS formulary [18] (which was translated, adapted and validated for the Portuguese population) and it is our intention to publish the results briefly. Our goals also involve examining the changing trends of PSC over time, assessing the cultural impact of PS initiatives and interventions and defining internal and external benchmarking.
In Medicine, it is certain that the vulnerability of those who are sick is associated with the inevitability of the occurrence of AE caused by those who have to act and provide care in environments and systems that are susceptible to those events. However, it is no less true that the adoption of a PSC is a proven useful tool to promote the safety of patients and clients, a place that sooner or later we will all occupy.
Acknowledgement
The authors are grateful to healthcare professionals from Primary Healthcare of Madeira Island that collaborated with us in accomplishing this project. Researchers also thank the Administration Institute of Health and Social Affairs, IP-RAM (IASAUDE, IP-RAM) for their support and contribution in spreading the questionnaire.
Ethical Approval
The study was approved by the Research Ethics Committee of the Madeira Island Regional Service of Healthcare (SESARAM, E.P.E.), NOVA Medical School and Portuguese National Data Protection Commission.