- (2004) Volume 5, Issue 5
Stefano Crippa1, Claudia Bonardi1, Giorgio Bovo2, Chiara Mussi1, Carlo Angelini1, Franco Uggeri1
1Department of Surgery and 2Department of Pathology, University of Milan-Bicocca, San Gerardo Hospital. Monza (MI), Italy
Received May 26th, 2004 - Accepted July 15th, 2004
Context Unlike primary pancreatic carcinoma, metastases to the pancreas are rare events and their resection may be performed as a palliative treatment. The aim of this study was to review our experience with the operative management of pancreatic metastases from breast carcinoma. Case report Three patients underwent pancreaticoduodenectomy for pancreatic metastases from breast carcinoma between 1990 and 2002. The clinical features of and the results after resection were examined. The presenting clinical symptoms were jaundice, pain and weight loss. In all cases, the pancreatic metastases were solitary lesions located in the head of the pancreas and the intervals between the primary breast carcinoma and the pancreatic metastases were 3, 5 and 7 years. The primary tumor was lobular carcinoma. Metastases were initially misdiagnosed as primary cancers. All patients underwent pancreaticoduodenectomy. One patient died from disseminated metastatic disease 26 months after surgery. The other two patients are alive 37 and 21 months after pancreaticoduodenectomy; the second one has had recurrence of the disease. Conclusion In rare cases, the pancreas may be the presenting site for breast metastases, typically years after treating the primary tumor. Pancreaticoduodenectomy can be performed in the absence of extreme metastatic disease; it can provide worthwhile palliation and improve survival..
Breast Neoplasms; Neoplasm Metastasis; Pancreatic Neoplasms
AJCC: American Joint Committee on Cancer; CEA: carcinoembryonic antigen; CT: computed tomography; ER: estrogen receptor; US: ultrasonography
Unlike primary pancreatic carcinoma, metastatic lesions to the pancreas are uncommon and account for approximately 2% of pancreatic malignancies [1]. At autopsy, the pancreas has been found to be a site of metastases in a wide range (3-12%) of patients with malignant tumors; the most common primary neoplasms are carcinomas and melanomas of the kidney, lung, breast and colon [2].
It is known that the favored sites for breast carcinoma dissemination are mainly the lungs, bones, liver, adrenal glands, brain and ovaries. However, breast carcinoma, especially in the advanced stages, can metastasize to virtually every organ of the body [3].
Although many patients with pancreatic metastases have widespread disease, isolated metastases can be found [4]. If an isolated metastasis in the pancreas becomes symptomatic, it is often misdiagnosed as primary pancreatic adenocarcinoma [5].
Recently, an improvement in hospital perioperative morbidity and mortality rates for pancreaticoduodenectomy has been documented [6] and resections of metastatic tumors to the pancreas have also been reported [7, 8]. Although the role of pancreaticoduodenectomy is not clearly defined in the management of metastatic lesions, it seems to be associated with improved survival and useful palliation.
We present 3 cases of pancreatic metastases from breast lobular carcinoma. The clinical features of the treatment and the outcome are discussed.
Case 1
In 1998, at this institution, a 67-year-old woman underwent a total mastectomy and axillary dissection for an invasive lobular carcinoma localized in the upper inner left quadrant, measuring 3 cm in its greatest dimension. Histological examination showed a grade II tumor exhibiting high levels of estrogen receptors; at that time, only nodal metastases were evident (pT2, pN1, M0, Stage IIB according to the American Joint Committee on Cancer, AJCC)).
She was treated by adjuvant chemotherapy and tamoxifen. The postoperative course was uneventful. The follow-up was uneventful for 3 years without breast or axillary recurrence of disease or evidence of distant metastases. In March 2001, she presented with obstructive jaundice, upper abdominal pain irradiating to the back and weight loss; Courvoisier’s sign was positive.
Routine examination showed CEA, CA 19.9, CA 125 and CA 15.3 levels within normal values and, at abdominal ultrasound, a dilatation of the gallbladder and extrahepatic ducts was seen. A CT scan showed a periampullary mass. Pylorus-sparing pancreaticoduodenectomy was performed. The postoperative course was complicated by wound infection. Pathological examination revealed a periampullary mass of 2 cm in its greatest diameter with negative resection margins. It was a pancreatic metastasis of breast lobular carcinoma, estrogen receptor (ER) positive, which was misdiagnosed as a primary pancreatic cancer. After surgery she was treated with hormonal therapy (tamoxifen).
The patient is alive and in good health 37 months after surgery, with no evidence of disease at the moment.
Case 2
In 1997, a 41-year-old woman underwent a quadrantectomy and axillary dissection for a breast carcinoma localized in the upper outer right quadrant at another hospital. Pathological examination revealed the resected specimen to be an invasive grade III lobular carcinoma with high levels of estrogen receptors (pT2, pN2, M0, Stage IIIA according to AJCC).
She was treated with adjuvant chemotherapy and radiotherapy. The follow-up was uneventful for 5 years. In July 2002, she presented at our institution with obstructive jaundice and weight loss. A tumor in the head of the pancreas, 2 cm in diameter, was found by abdominal ultrasonography. The tumor showed contrast enhancement on abdominal CT scan. Routine examinations were all within normal limits. In August 2002, a pylorus-sparing pancreaticoduodenectomy was performed and the postoperative course was complicated by pneumonia.
The pathologic diagnosis was that metastasis of the breast lobular carcinoma had occurred, exhibiting estrogen receptors. The patient was treated with postoperative chemotherapy and tamoxifen therapy. She is alive 21 months after the pancreaticoduodenectomy with evidence of a new pancreatic recurrence of disease.
Case 3
In 1990, at this institution, a 50-year-old woman underwent a quadrantectomy and axillary dissection for a breast cancer localized in the upper outer right quadrant. The resected specimen was an invasive grade II lobular carcinoma with no estrogen receptor exhibition (pT2, pN0, M0, Stage IIA according to AJCC). The postoperative course was uneventful; the patient was treated by adjuvant radiotherapy while no adjuvant chemotherapy was administered.
In 1997, 7 years after the initial excision, she presented with obstructive jaundice and progressive midepigastric pain. Abdominal ultrasonography and CT scan showed a dilatation of the gallbladder and the extrahepatic ducts associated with a mass in the head of the pancreas, measuring 3 cm in diameter.
The patient underwent pylorus-sparing pancreaticoduodenectomy and the postoperative course was uneventful. She was also treated with postoperative chemotherapy. Pathological examination of the surgical specimen revealed a metastasis of breast lobular carcinoma in the head of the pancreas. She was in good health for 10 months after pancreaticoduodenectomy. Then, her clinical condition started to deteriorate rapidly with evidence of generalized metastatic disease and she died 26 months after pancreatic surgery.
Summary data
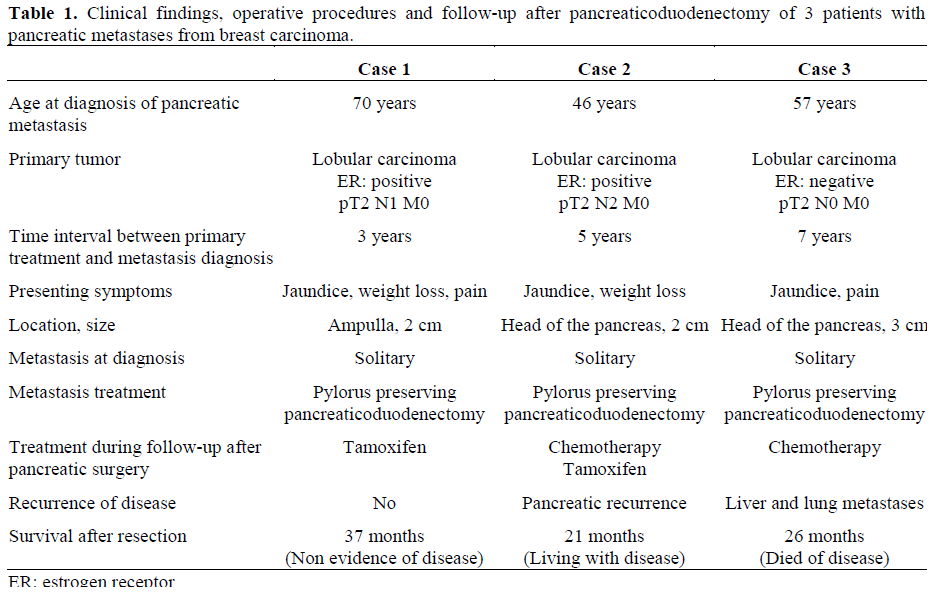
Clinical findings of the patients are summarized in Table 1 together with the operative procedures and follow-up data of the treated patients. Histological features of the surgical specimens are showed in Figures 1 and 2 (Case 2) and Figure 3 (Case 3).
While the prevalence of liver metastases from breast carcinoma can be as high as 40% in autopsy-based reports, involvement of the gastrointestinal tract and pancreas is less frequent [3, 9, 10, 11]. Asch et al. showed a gastrointestinal spread in 16.4% of 337 patients who died from breast carcinoma [9] while Cifuentes and Pickren found the incidence of pancreatic metastases to be 13% among 707 autopsies of breast cancer patients [10]. Most of these patients had widespread metastatic disease. More recently, some cases of isolated pancreatic metastases from breast cancer have also been reported [5, 7, 12, 13, 14].
Lobular breast carcinoma, as was found in the three patients described in this report, seems to metastasize with a particular predilection to the gastrointestinal tract [15]. Furthermore, a subclass of lobular carcinoma, called signetcell carcinoma of the breast, has been associated with unusual patterns of metastatic spread, including gastrointestinal and pancreatic metastases [16].
Jaundice in patients with breast carcinoma is most likely to be the result of diffuse metastases of the liver and the onset of jaundice is a sign associated with a mean survival of only 1 month [17, 18]. In a small subset of patients, jaundice is caused by extrahepatic bile duct obstruction due to lymph node or pancreatic metastases [5, 12, 17]. It is important to identify patients with solitary pancreatic metastases since they are good candidates for combined treatment including surgery, chemotherapy, radiation and hormonal therapy.
In our series, the presenting symptoms were jaundice (cases 1, 2 and 3) associated with weight loss (cases 1 and 2) and pain (cases 1 and 3); these symptoms are also commonly found in patients with primary pancreatic cancer. Pancreatic metastatic tumor may be also completely asymptomatic as in the series reported by Le Borgne et al. [7] and by Hiotis et al. [8]. In another report of 18 patients with pancreatic metastases, 15 were asymptomatic and they were detected on routine follow-up examination [19]. We would like to stress that the preoperative diagnosis of a secondary pancreatic tumor begins with suspicion based on the history of a previously known nonpancreatic cancer [4].
Moreover, the radiological evidence of multiple lesions in the pancreas may support the suspicion of pancreatic metastases [20]. Imaging studies included CT scan and magnetic resonance imaging. Highly vascular tumors are more likely to be secondary than primary cancer, which is often hypovascular.
However, not all pancreatic metastases are hypervascular and these lesions must still be distinguished from primary neuroendocrine carcinoma [5, 21].
The time interval between primary nonpancreatic cancer and the detection of pancreatic metastases varies widely and the diagnosis of recurrent tumor to the pancreas usually occurs within 3 years [21]. It is known that a long disease-free interval is very frequent for renal cell carcinoma [4, 8] but it is also possible for other metastatic cancers: two cases of solitary metastasis to the pancreas from breast carcinoma occurring 8 years after mastectomy have been reported [5, 18]. In our series, the intervals between primary breast carcinoma and pancreatic metastases were 3, 5, and 7 years, respectively. In the literature, synchronous pancreatic metastases from non pancreatic tumors have been reported in about 15% of cases [4, 21, 22]. To the best of our knowledge, only one case of a solitary synchronous pancreatic metastasis from breast carcinoma has been reported [7].
Indications for pancreatic resection of metastases have not been clearly defined. Some authors consider isolated metastases to the pancreas in the absence of a widely metastatic disease as the best indication for performing surgery [4, 7, 8]. Moreover, resection is most likely to be warranted in patients presenting after a long disease-free interval following primary cancer treatment, suggesting a biological pattern of slow growth [5, 23]. Regarding patients who underwent pancreatic resection for breast carcinoma metastases, the survival rate ranged from 12 to 132 months [4, 12]. In our experience, one patient is alive and free of disease 37 months after pancreaticoduodenectomy, while a second patient is alive but with a pancreatic recurrence of disease 21 months after surgery. The third patient died of disease 26 months after a pancreaticoduodenectomy.
In patients presenting with jaundice, if a curative resection can not be performed because of invasion of the mesenteric vessels or the presence of disseminated metastases, surgical or endoscopic palliation should be chosen [4, 17]. Relief of cholestasis due to extrahepatic bile duct obstruction using a surgical bypass or biliary stent can significantly improve patient survival and the quality of life [24]. Z’graggen et al. reported that a patient who underwent hepaticojejunostomy and gastrojejunostomy associated with chemotherapy for a pancreatic metastasis from breast cancer survived for 54 months [5].
Besides surgery, patients with metastases from breast carcinoma can be treated by chemotherapy and hormonal therapy with similar results if the tumor is positive for estrogen receptors [25]. Long-term palliation can be achieved in patients with breast cancer metastatic to the gastrointestinal tract if they are responsive to tamoxifen [26]. Considering the low toxicity of hormonal therapy and its capability of improving survival and the quality of life in the setting of metastatic disease, tamoxifen should also be administered to patients with pancreatic metastases from breast carcinoma exhibiting estrogen receptors, as we did.
It is well-known that patients with metastatic breast cancer may live for months or even years. For this reason, we believe that aggressive treatment for patients with isolated metastases from breast cancer is justified. In the case of a solitary metastasis to the pancreas in the absence of multiple metastatic disease, a pancreatic resection should be performed, if technically possible, in order to obtain palliation, to relieve biliary or duodenal obstruction and to improve survival. Liver and peritoneal metastasis from breast cancer should be ruled out.
In conclusion, even if we have limited experience with only three cases treated in an 8-year period, this report suggests that, in selected patients with isolated metastases from breast carcinoma, a pancreaticoduodenectomy can be performed safely.
Surgical resection combined with systemic therapy can provide worthwhile palliation, thus improving survival.