- (2000) Volume 1, Issue 3
Generoso Uomo*
Internal Medicine Department, 3rd Division, Cardarelli Hospital. Napoli, Italy
Drug Therapy; Endoscopy (treatment); Investigative Techniques; Pancreatitis, Acute Necrotizing; Therapeutics
AP: acute pancreatitis; ARDS: adult respiratory distress syndrome; CECT: contrast-enhanced-tomography; ERCP: endoscopic retrograde cholangiopancreatography; ES: endoscopic sphincterotomy; SIRS: systemic inflammatory response syndrome; TPN: total parenteral nutrition; US: ultrasonography
Acute pancreatitis (AP) is an inflammatory disease of the pancreas that often carries a complicated and severely life-threatening course and still remains a demanding and dreadful disease for both patients and clinicians. Over the last few years, changes in the understanding of the patho-physiologic factors, combined with recent technologic advances, have fortunately led to improvements in the management of these patients. From the practical standpoint, some important indications should be pursued to optimize the treatment:
a) an early objective severity assessment by simple means is mandatory, and all patients should be considered as suffering from severe AP until proven otherwise; in this respect, the recent clinically based classification system for AP - the Atlanta classification [1] - seems to be a valid method of discriminating between the mild and severe forms;
b) the treatment should be started as early as possible and should be primarily addressed to the removal of etiological factor(s) and to support the hydroelectrolytic, caloric and circulatory balance; specific treatment (antiproteases, antibiotics) should be added in severe cases; the main goals of medical therapy also include the need of limiting systemic complications and prevention of pancreatic infection once necrosis takes place;
c) referral to a specialized Center should be carefully considered for those patients with severe disease at major risk of lifethreatening complications; as suggested by the UK guidelines [2], a specialized Center for the management of severe AP should be characterised by the presence of the following:
· a large general hospital with a full range of principal medical and surgical specialities;
· a multidisciplinary team of specialists in internal medicine, surgery, endoscopy, intensive care, pathology with a full staff of support;
· a contrast-enhanced-tomography-scan (CECT-scan) and ultrasonography (US) with full-time availability together with physicians expert in percutaneous procedures; the addition of magnetic resonance imaging and angiographic facilities would be helpful but not essential;
· experencied endoscopists with endoscopic retrograde cholangiopancreatography (ERCP) and related interventional procedures available daily;
d) the approach to managing AP should be interdisciplinary to get the best treatment results for these patients.
The majority of patients with AP suffer from mild pancreatitis, which is a self-limiting disease with a benign course and a rapid recovery. On the other hand, 15-30% of patients suffer from the severe disease which usually requires a lengthy hospital stay and still accounts for a high morbidity and mortality rate [1, 3-7].
Treatment of the mild forms of AP is largely supportive including effective pain control, and fluid and nutritional support. It is traditional to “rest” the pancreas (to minimize pancreas secretion) by discontinuing oral intake until there is near-complete resolution of abdominal pain and tenderness. Although this has never been rigorously evaluated, the practice makes sense since premature feeding may cause an exacerbation [8]. A naso-gastric tube is not helpful in the treatment of mild AP but might play a role in treating either gastric or intestinal ileus and preventing aspiration of gastric contents in severe AP [4]. Naso-gastric suction is also reasonable in patients with mild AP presenting persistent nausea and vomiting. Naso-gastric aspiration should be removed as soon as flatus discharge and bowel peristalsis are re-established. H2- blocking agents or proton pump inhibitors may counterbalance the tendency to metabolic alkalosis induced by vomiting or naso-gastric suction and may prevent stress-induced acute peptic lesions [5]. As a rule, nutritional support is administered for a few (four-six) days as follows: a) fluids: 30-35 mL/kg body weight/day plus integration of fluid loss; b) calories: 25-30 kcal/day (glucides 70%, lipids 30%); c) proteins: 1 g/150kcal; d) supplementation of microelements and ions if required. Narcotic analgesics are given for pain relief; meperidine and pentazocine have proved effective without negative effects on the Oddi sphincter [9].
Re-establishment of oral refeeding can be considered as soon as abdominal pain and tenderness have subsided and bowel sounds have returned. The risk of pain recurrence during refeeding is very low in patients with mild, non-necrotic pancreatitis [10]. It goes without saying that removal of such factors, such as alcohol or drugs, which may have precipitated the attack would be appropriate. ERCP with endoscopic sphincterotomy (ES) is indicated in the case of gallstone pancreatitis with associated cholangitis and common bile duct obstruction, whereas current available data do not indicate any advantage following ERCP + ES in comparison with conventional treatment in mild biliary AP (Figure 1) [11-15]. The use of ERCP after an attack of gallstone AP has decreased but, prior to a cholecystectomy, depends on the evidence for retained stones and on the attitude and experience of the surgeon concerning laparoscopic removal of choledochal stones [16].
Treatment of Severe AP
Roughly 15-30% of patients with AP will have an attack classified as severe and 95 % of the deaths will occur in this subset [1, 2]. Management and monitoring of these patients must therefore be more aggressive, with a prolonged stay in an intensive-care Unit for several of them. The mainstay of the management of severe AP includes: a) elimination of the cause of the primary insult if possible, i.e, relief of obstruction in biliary forms by endoscopic treatment within the first 24-48 hours of admission (Figure 1) [17]; b) identification and treatment of secondary causes of organ failure, such as hypovolemia and tissue hypoperfusion, hypoxemia, pancreatic infections, and nosocomial infections [18].
The most important precipitating factors for the development of multi-organ failure are probably unrecognized and untreated hypoxemia and hypovolemia and an insufficient initial supplementation. Rapid restoration of intravascular fluid volume is one of the few therapeutic measures that are generally accepted as effective in severe AP [5, 8]. For this purpose, invasive monitoring (central venous pressure measurement) is frequently necessary; in fact, vital signs and urinary output may cause one to underestimate daily fluid requirements that often exceed 5-6 litres/day [19]. Monitoring of central venous pressure leads to correct fluid replacement in relationship to hemodynamic parameters and cardiac reserve. The use of a pulmonary artery wedged catheter should be indicated in patients with cardiovascular instability or increasing respiratory failure. During the early phase of AP. many patients present normal or nearnormal blood pressure, despite quite severe hypovolemia, with preservation of the central nervous system and coronary blood flow, and decrease of the perfusion of the intraabdominal organs perfusion. Thus, global oxygen transport and delivery is to be established as soon as possible; on the other hand, pancreatic ischemia plays an active role in the development of the necrotic process [20]. Regular arterial blood gas analysis is essential as the onset of hypoxia and acidosis may be detected too late by clinical means alone [2]. Hypoxemia should be prevented by securing free airways and by administration of extra oxygen via a nasal mask. Endotracheal intubation and controlled ventilation with a low level of positive end-expiratory pressure often become necessary to gain satisfactory oxygenation in the case of adult respiratory distress syndrome (ARDS). The use of cardioinotropic agents follows traditional schemes; in particular, dobutamine may be necessary in patients who experience systemic inflammatory response syndrome (SIRS) or sepsis and who present low systemic vascular resistance and low cardiac output.
For routine plasma replacement/expansion, synthetic colloids (dextran, gelatin solutions) can be used instead of human albumin with advantages from the economic and safety standpoints. However, when the serum albumin level is below 20 g/L or total plasma protein are very low (<40 g/L), albumin should be administered [19]. Packed red blood cells are generally requested if the hematocrit value falls to 25%; a hematocrit value of 30-32% is associated with the best viscosity and hemorheologic findings within pancreatic microcirculation [21].
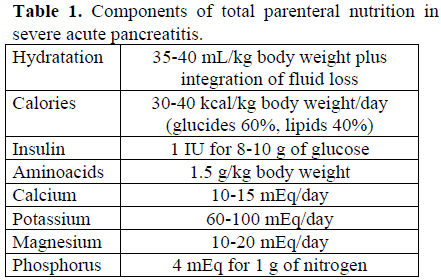
Deterioration of renal function, which might be caused by hypotension or by direct toxicity of pancreatic enzymes, is treated by conventional strategy (hemodialysis) [2]. Hydration and total parenteral nutrition (TPN) should start very early. Sufficient amounts of fluids, calories, nitrogen and other components are indicated in Table 1. Lipids should be included in TPN unless serum triglycerides are elevated to a level >500 mg/dL. Fluid balance should be reassessed at least every 12 hours during the first few days in order to ensure adequacy of fluid replacement. Periodic measurements of serum ions should be utilized to gauge the adequacy of replacement. In clinical practice, a major concern is the decrease of serum potassium; replacement is quite easy, except for patients with associated cardiac arrhythmias.
As for mild attacks, oral refeeding should be considered when abdominal pain and tenderness have subsided and bowel sounds have returned.
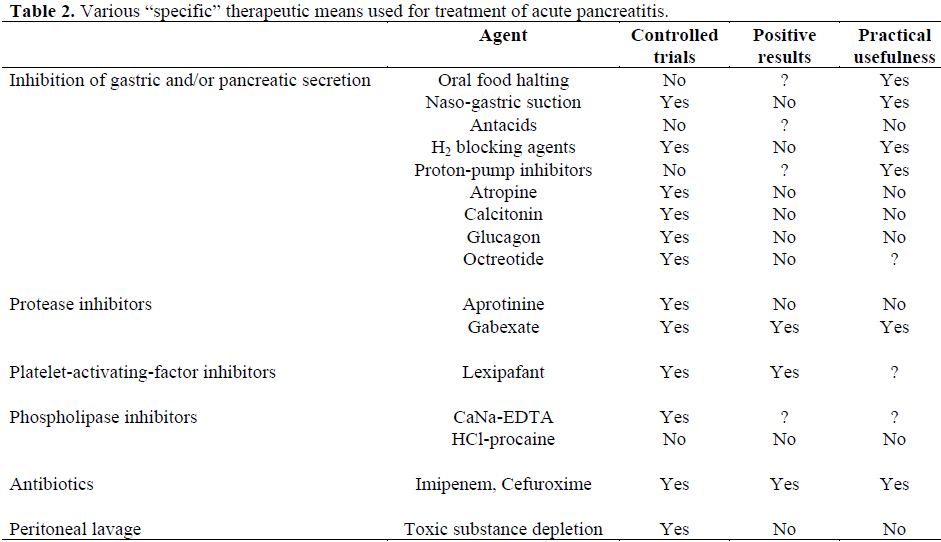
Various “specific” drugs have been utilized over the last number of years for the treatment of severe AP. However, looking at the results of the published controlled trials on this topic [22], only a few drugs give positive results together with a demonstrated usefulness from a practical standpoint (Table 2). Modern antiprotease therapy (gabexate mesilate) can reduce systemic complications and the need of surgery in severe AP [23, 24]. Two recent placebo-controlled trials [25, 26] showed that octreotide is not helpful in reducing the complication and mortality rate in patients with severe AP. Results from recent controlled trials [27-31] and one retrospective review [32] support the use of prophylactic antibiotics in the prevention of local and other septic complications in severe AP. Antibiotic therapy (imipenem, cefuroxime) should be commenced as early as possible after the identification of severe attack and should be continued for at least two weeks [33, 34].
Surgery should be considered specifically for severe necrotizing AP, excluding from this discussion all those cholecystectomies defined as “corrective” and performed after mild AP [35]. The traditional and well-accepted indications for surgery include: a) exploration for those patients with acute abdomen and no definitive diagnosis; b) biliary obstruction not amenable to endoscopic procedures, c) specific complications such as hemorrhage or fistulas; d) infection of necrosis and/or fluid collections; e) pancreatic abscess [35-37]. The clinical picture of peritonitis (“chemical” peritonitis) must be carefully assessed before opting for a surgical solution, since, after the acute phase, the patients often tend to improve or even resolve in the course of the first 24-48 hours of intensive medical therapy. Thus, peritonitis in itself in the course of severe AP is not an absolute indication for laparotomy.
Controversies exist regarding the indication for surgical debridement in the presence of extensive sterile necrosis, associated or not, with multi-organ failures. In the recent past, many surgeons considered the presence of pancreatic necrosis as a sufficient indication for surgical intervention, independent of the presence of infection, particularly in patients who do not respond (fail to improve) after 3 days of maximal care treatment [4, 37, 38]. They advocated that removal of necrotic tissue and pancreatogenic fluid (pancreatic broth) may prevent the systemic spread of the vasoactive mediators and toxins and interrupt the inflammatory process and the damage of the target organs. However, the benefits from surgery in severe AP with sterile necrosis have been difficult to establish because of the lack of comparison to the behaviour of unoperated patients. Also, surgical intervention in sterile necrosis causes pancreatic infection in 20% of patients with a very high mortality rate (50-60%) [39-41]. In addition, conservative treatment proved successful also in the presence of organ failure associated with sterile necrosis involving more than 50% of the gland [41, 42] and it has not yet been demonstrated that surgical procedures can improve a preoperative multi-organ system failure [35, 39]. Lastly, the rupture of the main pancreatic duct may be successfully managed without surgery if the necrotic process remains sterile [43]. So, the available data do not support a definitive management policy toward patients with sterile necrosis, while there is a general consensus that patients with infected necrosis should undergo surgical debridement. The crucial point remains the monitoring of the necrotic process. Percutaneous (US- or computed tomography-guided) fine needle aspiration is the only reliable test to diagnose infected necrosis and it should be performed if the patients experience both classic septic or septic-like symptoms and instability of cardiovascular, pulmonary or renal features. In addition, percutaneous drainage of infected necrosis may prove useful in patients unfit for surgery because of high anaesthesiological risk and/or in frail, very old patients [35].
With regard to the timing of surgery, this essentially depends on the occurrence of infective complications. Most cases (85%) of infected necrosis appear after the first two weeks of the disease. At this time, the debridement is fortunately easier and safer than early necrosectomy, because the demarcation of the necrotic foci is sharper [37, 44].