- (2008) Volume 9, Issue 3
Rahul Gupta1, Deepak Chettri1, Arun Sharma1, Ajay Duseja1, Radha Krishan Dhiman1, Yogesh Kumar Chawla1, Naveen Kalra2, Amod Gupta3, Arunanshu Behera4
Departments of 1Hepatology, 2Radiodiagnosis and Imaging, 3Ophthalmology, and 4General Surgery, Postgraduate Institute of Medical Education and Research. Chandigarh, India
Received January 2nd, 2008 - Accepted February 7th, 2008
Context Extrahepatic biliary obstruction secondary to pancreatic cysts is rare in patients with von Hippel Lindau syndrome. We describe a patient with von Hippel Lindau syndrome who had biliary obstruction due to pancreatic cysts who was initially managed endoscopically and then surgically. Case report A female patient with von Hippel Lindau syndrome which had been diagnosed ten years earlier based on the presence of pancreatic and renal cysts with retinal hemangiomas, presented with cholestatic jaundice of two months duration. On investigation, she was found to have lower end biliary obstruction caused by pancreatic cysts. The patient was initially managed with endoscopic retrograde cholangiography and a 7 French/10F/12F biliary plastic stent placement. Her cholestatic symptoms improved but required frequent stent exchange due to stent block; she finally underwent a hepaticojejunostomy and is doing well on follow-up. Conclusion This case highlights the fact that pancreatic involvement leading to biliary obstruction, although uncommon, can occur in patients with von Hippel Lindau syndrome. Endoscopic biliary stent placement and surgery are helpful in these patients.
Bile Ducts; Cholangiopancreatography, Endoscopic Retrograde Stents; Hemangioblastoma; Kidney Diseases, Cystic; Pancreatic Cyst; von Hippel-Lindau Disease
vHL: von Hippel Lindau
Von Hippel Lindau (vHL) syndrome is an autosomal dominant inherited condition associated with hemangioblastomas of the central nervous system and retina, renal cysts, renal cancer, pheochromocytoma, pancreatic cysts, ear involvement in the form of endolymphatic sac tumors and epididymal cystadenomas. Pancreatic involvement, especially as isolated organ involvement, is not common in patients with vHL [1, 2]. Simple benign cysts and cystadenomas are the most common pancreatic lesions [3]. Most affected individuals remain asymptomatic despite having pancreatic involvement. Extrahepatic biliary obstruction secondary to pancreatic cysts is a rare occurrence in vHL syndrome [3, 4, 5, 6, 7, 8]. We describe a patient with VHL who had biliary obstruction due to pancreatic cysts and was initially managed endoscopically and then surgically.
CASE REPORT
A 37-year-old female presented with a history of generalized pruritus of two months duration and was admitted for biliary drainage. She had been diagnosed with vHL syndrome 10 years earlier on the basis of retinal hemangiomas, and pancreatic and renal cysts. Surgical removal of one of the pancreatic cysts 10 years earlier due to abdominal pain showed a histopathology consistent with a simple pancreatic cyst. There was a family history of retinal angiomas in two of her siblings.
On physical examination, she was blind in the right eye but had normal vision in the left eye. Her abdominal examination revealed a firm irregular mass in the epigastrium extending up to the right hypochondrium with a few cystic areas. The liver, spleen and kidneys were not palpable. Investigation revealed a hemoglobin count of 13.4 g/dL (reference range: 12-18 g/dL), a total leukocyte count of 10.9 x109/L (reference range: 4-11 x109/L) and platelets of 200 x103/mm3 (reference range: 150-400 x103/mm3). Her liver function tests revealed a bilirubin count of 0.7 mg/dL (reference range: 0-1.0 mg/dL), aspartate aminotransferase (AST) 32 IU/L (reference range: 10-21 IU/L), alanine aminotransferase (ALT) 60 IU/L (reference range: 2-15 IU/L) and serum alkaline phosphatase 27 KAU (reference range: 0-13 KAU). Serum amylase and lipase values were normal. Ultrasonography showed dilated intrahepatic biliary radicals and a dilated common bile duct extending to the lower end. Almost the entire pancreas was replaced by multiple cysts in the parenchyma. The liver, gallbladder, hepatic vein and portal vein were normal. A few cysts were seen in either kidney. Contrast-enhanced computed tomography showed dilated biliary system extending to the lower end and a massively enlarged pancreas with multiple cysts causing compression at the lower end of the common bile duct (Figure 1). In addition, bilateral renal cysts were also seen. She refused surgical intervention and subsequently underwent endoscopic retrograde cholangiopancreatography (ERCP) which showed narrowing at the lower end of the common bile duct due to compression by pancreatic cysts and dilatation of the biliary system above the narrowing (Figure 2). Initially, a 7 French, 12 cm biliary plastic stent was placed in the right hepatic duct well above the narrowing which was later replaced by a 10 French stent. After the procedure, her liver function tests normalized and she became asymptomatic after one month but returned two months later with a blocked stent with increasing pruritus and jaundice. Repeat endoscopic retrograde cholangiography was done and a 12 French stent was placed, which also became blocked later, and she underwent a Roux-en-Y hepaticojejunostomy (Figure 3). Intraoperatively, the pancreas was bulky, and the pancreatic head and the rest of the pancreas had cysts of various sizes, some having a solid component. The procedure was carried out under intraoperative ultrasound guidance. The common bile duct in its midportion was obscured by the cysts; hence, a hepaticojejunostomy was carried out near the porta hepatis. She is being followed up monthly and has been doing well for the past two months.
Our patient has vHL syndrome on the basis of the presence of bilateral retinal angiomas, pancreatic and renal cysts and a family history of retinal angiomas. The diagnosis of vHL is usually based on the presence of various criteria as described by Melmon and Rosen [9] which include either a family history of retinal or CNS hemangioblasts, or CNS hemangioblastomas plus a hemangioblastoma, or visceral lesions (renal cysts, pancreatic cysts, tumor, pheochromocytoma), or two or more hemangioblastomas, or one hemangioblastoma and a visceral manifestation in patients with no clear family history.
Pancreatic involvement occurs in 17 to 56% of patients with vHL [1, 2]. Although CNS and retinal hemangioblastomas are the most common presenting features, pancreatic lesions as an isolated manifestation in vHL disease is seen in up to 12% of patients [3]. Though simple pancreatic cysts and cystadenomas represent the most common pancreatic lesions in vHL, various other pancreatic lesions reported in the literature include common ones such as neuroendocrine tumors as well as the rarer ones such as adenocarcinomas, hemangioblastomas and metastases from renal cell cancer [3]. Most patients with pancreatic involvement remain asymptomatic, although patients can present with abdominal pain, with or without evidence of pancreatitis [10, 11].
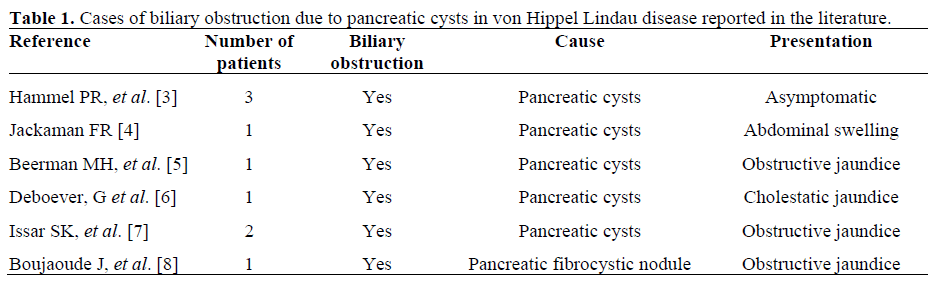
To the best of our knowledge, in vHL, bile duct obstruction due to pancreatic cysts has been previously described in only 9 cases of vHL (Table 1). These patients may remain asymptomatic or can present with obstructive jaundice and other features of cholestasis [3, 4, 5, 6, 7, 8]. Our patient has had a relatively long asymptomatic follow-up, except for the abdominal pain 10 years earlier and the present symptomatic cholestasis.
Treatment strategies for symptomatic pancreatic involvement in vHL should be individualized depending upon the patient profile and the presence or absence of renal cell carcinoma. Radiologically guided percutaneous aspiration and/or hypertonic saline sclerosis are options but diffuse pancreatic involvement hinders these procedures. In patients with symptomatic biliary obstruction due to pancreatic cysts, endoscopic biliary stent placement [6] is effective and can be a modality of choice where surgical and radiological intervention are difficult for technical and anatomical reasons or when the patient refuses surgery. Stent clogging, a known complication of biliary stenting may be tackled with repeated stent exchange and by using a stent having a bigger diameter. Surgical management such as cystectomy/enucleation or a Whipple procedure [8] in patients with only a few cysts seems feasible. Because of the non-malignant potential of these cysts, a surgical bypass procedure such as a Roux-en-y hepatico/ choledochojejunostomy seems reasonable as a part of pancreatic saving procedure.
In conclusion, our case points out that pancreatic cysts leading to biliary obstruction, although uncommon, can occur in patients with vHL. Endoscopic biliary stent placement/surgical intervention are helpful in these patients.
The authors have no potential conflicts of interest