Perspective - (2025) Volume 26, Issue 1
Received: 11-Jun-2024, Manuscript No. IPP-24-20422; Editor assigned: 13-Jun-2024, Pre QC No. IPP-24-20422 (PQ); Reviewed: 17-Jun-2024, QC No. IPP-24-20422; Revised: 12-Feb-2025, Manuscript No. IPP-24-20422 (R); Published: 19-Feb-2025, DOI: 10.35841/1590-8577-26.1.905
Infections of pancreatic fluid collections, pseudocysts or necrosis with subsequent abscess formation are common complications of acute and chronic pancreatitis. Hence, regular follow-up examinations involving ultrasound to detect (abscessed) pancreatic collections at early stages are recommended. Here, we present clinical images of a patient with chronic pancreatitis and anamnestic ’’endoscopic treatment’’ where unnoticed growth of an infected pancreatic pseudocyst led to the generation of a remarkably large pancreatic "supercyst" filling the entire abdominal cavity. The possibility of pancreatic "supercyst" formation highlights the necessity for regular follow-up examinations, especially in patients with chronic pancreatitis or with previous interventional treatment.
A 44-year-old man with a four-year-history of alcohol-induced chronic pancreatitis presented to the emergency room with diffuse abdominal pain, dyspnea and fatigue. Physical examination revealed a distended and pressure sensitive abdomen. Bloodwork showed elevated CRP levels (129 mg/l), leukocytosis (9.29/nl), anemia (hemoglobin 3.7g/dl), thrombocytosis (608/nl), and a slight increase of lipase levels (62 U/L). Due to dyspnea and massively distended abdomen the patient was admitted to the intensive care unit. CT-imaging displayed a large (28 × 26 cm) intraabdominal mass with air pockets (Panel A)likely emanating from the pancreas.
Moreover, a previously transgastral-endoscopic placed double-pigtail drainage was visible on CT-imaging (Panel B, arrow). Anamnestic this drainage was placed in a referral hospital one year ago, and due to the patient’s noncompliance to medical advice, the drainage has not been removed so far (Panel C). Taken together, a suspected diagnosis of a remarkably large abscessed pancreatic pseudocyst in the context of chronic pancreatitis was made. Due to respiratory instability and to avoid endotracheal intubation we decided to promptly place bedside percutaneous pigtail drainages (2 × 14 Ch) (Panel D, arrow). The entire mass could be successfully removed within one day rendering an enlarged and calcified pancreas (Figure 1) visible on CT-imaging. The drainage fluid was purulent (Panel F) and microbiological examination yielded growth of Klebsiella pneumonia and Streptococcus anginosus corroborating the diagnosis of abscessed pancreatic pseudocyst. Ensuing 19 days of antibiotic treatment and correction of anemia via blood transfusions and iron substitution, the patient was discharged. Infections of pancreatic pseudocyst with subsequent abscess formation are common complications of acute and chronic pancreatitis. Hence, regular follow-up involving ultrasound to detect (abscessed) pancreatic pseudocysts at early stages are recommended, especially to patients suffering from chronic pancreatitis or after interventional therapy to avoid the development of abscessed pancreatic pseudocysts into huge pancreatic "supercysts". Furthermore, patients should be well informed of the negative consequences in case they do not present for regular follow-up [1,2]. 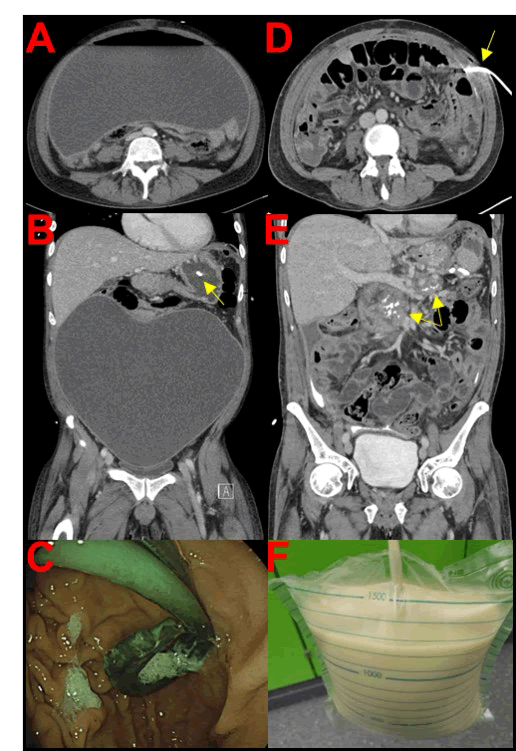
Figure 1: Multimedia.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Webb T, Pancreatic Enzyme Disorders: Diagnosis, Treatment and Management Strategies. JOP. J Pancreas. (2025) 26:905.
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.