Research - (2022) Volume 6, Issue 4
Non-Invasive Predictors of Large Esophageal Varices in Patients with Cirrhosis in Cameroon
Nsenga Djapa Guy Roger1,2*,
Kowo Pierre Mathurin3,
Mohamadou Galdima4,
Ndjitoyap Ndam Antonin Wilson3,
Talla Paul3,
Ankouane Andoulo Firmin3 and
Njoya Oudou3
1Department of Internal Medicine and Specialties, University of Dschang, Cameroon
2Gastroenterology Unit, Internal Medicine Service, Ebolowa Regional Hospital, Cameroon
3Department of Internal Medicine and Specialties, University of Yaoundel, Cameroon
4Department of Internal Medicine and Specialties, University of Ngaoundere, Cameroon
*Correspondence:
Nsenga Djapa Guy Roger, Department of Internal Medicine and Specialties, University of Dschang,
Cameroon,
Email:
Received: 30-Mar-2022, Manuscript No. IPJCGH-22-13411;
Editor assigned: 01-Apr-2022, Pre QC No. IPJCGH-22-13411 (PQ);
Reviewed: 15-Apr-2022, QC No. IPJCGH-22-13411;
Revised: 20-Apr-2022, Manuscript No. IPJCGH-22-13411 (R);
Published:
27-Apr-2022, DOI: 10.36648/2575-7733.6.4.20
Abstract
Background: Esophageal varices (EVs) are a consequence of portal hypertension in patients with chronic liver
diseases. Current guidelines recommend that all patients with cirrhosis should undergo screening endoscopy at
diagnosis to identify varices at high risk of bleeding which will benefit from primary prophylaxis. This study was
conducted to evaluate known noninvasive predictors of large esophageal varices in Cameroon.
Patients and methods: Patients with liver cirrhosis seen from November 2013 to October 2014, meeting our
selection criteria were consecutively enrolled. Demographic data (age and sex), relevant clinical (ascites, encephalopathy),
biological (platelet count, bilirubinemia, albuminemia and prothrombin level), ultrasonographic (spleen
diameter, portal vein diameter, right liver span and ascites) and endoscopic (EV, gastric varives, portal hypertensive
gastropathy and ulcers) parameters were assessed. Univariate and multivariate analysis was done on the data for
predictors of large EVs. Statistical significance was reached with a p ≤ 0.05.
Results: A total of 64 patients were enrolled in our study. The mean age was 51 ± 18.09 years, with a male predominance
(1.78). Viral hepatitis accounted for the majority of causes of cirrhosis (51.6% were related to hepatitis B
while 46.9% were related to hepatitis C). Nine patients (14.1%) had alcohol related cirrhosis. Thirty three (51.56%)
presented with ascites. Child Pugh score, spleen diameter, albumin level, platelet on spleen diameter and right liver
span on albumin ratios were significantly associated with the presence of esophageal varices. Spleen diameter,
Child Pugh score and right liver span on albumin ratio had the best positive predictive values (PPV) of the presence
of large esophageal varices with cut offs of 148.34 mm (PPV=74.4%), 9 (PPV=72.4%), and 4.4574 (PPV=66.7%)
respectively. Child Pugh score, spleen diameter, platelet count on spleen diameter and right liver span on albumin
ratios were independent predictors of esophageal varices. There was no correlation between bilirubin level, portal
vein diameter and EV.
Conclusion: Child Pugh score, spleen diameter, albumin level, platelet on spleen diameter and right liver span on
albumin ratios are good predictors of EV. Though the predictive values were generally low, spleen diameter, Child
Pugh score and right liver span on albumin ratio were best at predicting large EV. There was no correlation between
bilirubin level, portal vein diameter and EV.
Keywords
Esophageal varices; Cirrhosis; Cameroon
Introduction
One of the most relevant complications of cirrhosis is the occurrence
of portal hypertension which leads to varices within the
splanchnic circulation. In this regard, esophageal varices (EV)
are a major concern in cirrhotic patients because of the risk of
bleeding and related high mortality [1]. The prevalence of EV in
newly diagnosed cirrhotic patients is approximately 60%-80%
and the 1 year rate of first variceal bleeding is approximately
5% for small EV and 15% for large EV [1,2]. The determination
of the presence of EV by upper digestive endoscopy is therefore
mandatory in patients with cirrhosis at diagnosis [3]. For long
term follow up, guidelines recommend monitoring of cirrhotic
patients by routine endoscopy for the detection of the development
of EV and to initiate prophylactic measures to prevent
the bleeding of EV when they become large [3,4]. Endoscopy is
however a costly, invasive, and time consuming procedure [5].
The detection of EV in African patients with cirrhosis is a matter
of concern because of the frequent malfunction or unavailability
of endoscopy units [6]. This study was conducted to evaluate
known noninvasive predictors of esophageal varices in patients
with cirrhosis in Cameroon.
Patients and Methods
It was a prospective, cross-sectional study conducted in three
university teaching hospitals in Yaounde for a period of 12
months from November 1st 2013 to October 31st 2014. All patients
underwent a detailed clinical evaluation at inclusion. Patients
with evidence of hepatocellular carcinoma and/or portal
vein thrombosis on ultrasonography or computer tomography,
previous or current treatment with beta blockers, nitrates and
diuretics were excluded from the study including those who
had received endoscopic treatment for portal hypertension.
Clinical Assessment
Relevant history and physical characteristics including symptoms
and signs of liver failure (spider angioma, palmar erythema,
jaundice, fetor hepaticus etc.), hepatomegaly, splenomegaly,
and abdominal vein collaterals were recorded. Ascites was
graded as none, mild (detectable only on ultrasound), moderate
(visible moderate symmetrical abdominal distension) or severe
(marked abdominal distension) [7]. Hepatic encephalopathy
was graded from grade 0 to 4, as per the Conn's grading
as [8]:
• Grade 0: Normal neuropsychological functioning
• Grade 1: changes in behavior with minimal change in level
of consciousness
• Grade 2: gross disorientation, drowsiness, possibly asterixis,
inappropriate behavior
• Grade 3: marked confusion, incoherent speech, sleeping
most of the time but arousable to vocal stimuli
• Grade 4: comatose, unresponsive to pain; decorticate or
decerebrate posturing.
Biological Assessment
Hematological and biochemical workup included measurement
of hemoglobin, total leukocyte count, platelet count, prothrombin time, and serum concentrations of bilirubin (total
and conjugated), protein, albumin, alanine aminotransferase
and aspartate aminotransferase. For each patient, a modified
Child Pugh score was calculated [9].All patients were screened
for viral hepatitis. They were considered to be infected with:
• Hepatitis C virus when they tested positive for anti HCV
antibodies using a third generation ELISA commercial kit.
• Hepatitis B virus when they tested positive for HBsAg and/
or positive HBcAb with a detectable viral load using a real
time polymerase chain reaction assay. Hepatitis B surface
antigen was tested using a third generation ELISA test. The
test was considered positive when the optical density of
the test sample was greater than the threshold. It was
considered negative when the optical density of the test
sample was lower than the threshold.
• Hepatitis D virus Screening was only requested when there
was evidence of hepatitis B infection. Patients were considered
infected when they had a positive serology. Commercial
total anti-HDV antibody ELISA kits were used to
screen for hepatitis D viral infection.
Tests for other causes of cirrhosis (serum ceruloplasmin and slit
lamp examination for Wilson’s disease, tests for autoantibodies
for autoimmune liver disease, iron studies for hemochromatosis)
were practically not carried out in our study.Cirrhosis was
said to be related to alcohol when consumption was at least 40
g per day for men and 30 g per day for women.
Ultrasound Doppler
All patients underwent ultrasonography after overnight fast
and the following details were recorded: Maximum vertical
span of the liver; nodularity of liver surface; spleen size (length
of its longest axis); diameter of the portal and splenic veins;
and presence of ascites [10].
Endoscopic Evaluation
All patients underwent upper gastrointestinal endoscopy for
assessment of esophageal and gastric varices. If esophageal
varices were present, they were graded using the North Italian
Endoscopic Club as
• Grade 1: small straight varices that can be depressed;
• Grade 2: enlarged tortuous varices occupying less than
one third of the lumen; and
• Grade 3: large coil shaped varices occupying more than
one third of the lumen [11].
Varices are considered large varices whenever they are either
grade 2 or 3.When present, gastric varices were graded following
Sarin’s classification [12]. The presence or absence of portal
hypertensive gastropathy, gastric and duodenal ulcers were
recorded.
Variables
Qualitative variables were gender, cause of cirrhosis, grade of
esophageal varices, type of gastric varices, gastric and duodenal
ulcers.Quantitative variables were age, Child Pugh score,
spleen diameter, portal vein diameter, right liver span, platelet count, serum albumin, serum bilirubin, prothrombin time.
Statistical Analysis
Data was analyzed using the SPSS (version 11 for windows)
and Microsoft Excel 2007 softwares. For quantitative variables,
means and standard deviations were calculated. For qualitative
variables, proportions were calculated with their confidence
intervals (CI). Univariate analysis for determining the association
of various clinical, laboratory and ultra-sonographic variables
with presence of esophageal varices was performed using
Pearson’s χ2 test. P<0.05 were considered significant, and
all variables found significantly associated with the presence
of esophageal varices were studied on multivariate analysis to
identify independent predictors of the presence of esophageal
varices, and the threshold of predictively of large esophageal
varices.
Results
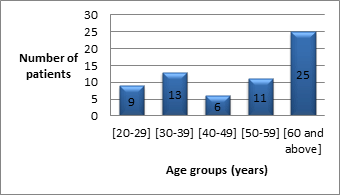
A total of 64 patients were enrolled in our study, most of whom
were men (with a male to female ratio of 1.78) and a media
nage of 54 years old (Figure 1).
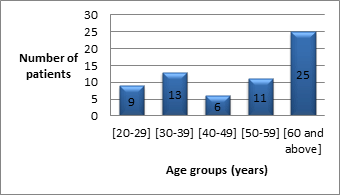
Figure 1: Distribution of patients with respect to age.
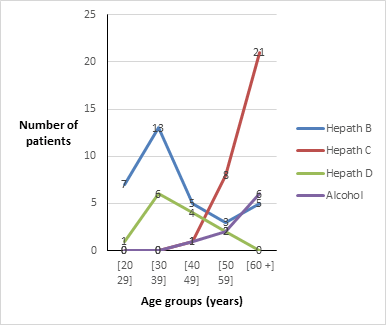
While hepatitis C-related cirrhosis predominantly affected elderly
patients, hepatitis B infected patients were relatively
younger (Figure 2). Similarly, while delta hepatitis was mostly
with cirrhosis among young patients, risky alcohol consumption
predominantly affected the elderly.
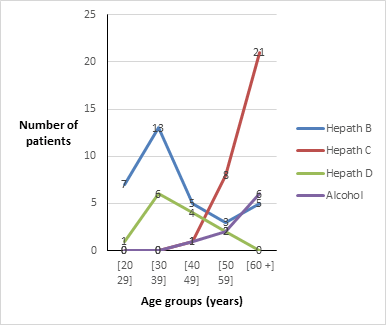
Figure 2: Distribution of patients according to the etiology of cirrhosis within the various age groups.
Ascitis was the most relevant clinical finding at inclusion, followed
by jaundice. No patient in our study presented with
encephlopathy, spinar angiomata or leukonychia. Only 18 patients
(28.13%) had compensated cirrhosis at inclusion.
Esophageal varices were present in 48 patients (75%). Nine had
gastroesophageal varices, with 77.78 being type I (Table 1).
Table 1: Non-invasive markers and their correlation to esophageal varices.
| Non-invasive markers |
Cases (N=64),% |
EV (N=48),% |
RR |
p-value |
| Child-Pugh class |
| A |
18 (28.13) |
8 (44.4) |
1 |
|
| B |
31 (48.44) |
26 (83.87) |
1.87 [0.54-3.21] |
0.006 |
| C |
15 (23.44) |
14 (93.33) |
2.86 [0.63-5.09] |
0.012 |
| Platelet count |
| >150000/mm3 |
12 (18.75) |
6 (50) |
1 |
|
| 100000-150000/mm3 |
20 (31.25) |
14 (70) |
0.85 [-0.63-2.33] |
0.262 |
| <100000/mm3 |
32 (50) |
28 (87.5) |
1.95 [0.40-3.49] |
0.013 |
| Prothrombin time |
| >70% |
21 (32.81) |
13 (61.9) |
1 |
|
| 50-70% |
32 (50) |
26 (81.25) |
0.98 [-0.27-2.23] |
0.124 |
| <50% |
11 (17.19) |
9 (81.81) |
1.02 [-0.75-2.79] |
0.259 |
| Albumin |
| >35 g/l |
24(37.5) |
13 (54.17) |
1 |
|
| 28-35 g/l |
17 (26.56) |
16 (94.12) |
2.61 [0.43-4.78] |
0.019 |
| <28 g/l |
23 (35.94) |
19 (82.61) |
1.39 [0.047-2.74] |
0.043 |
| Bilirubin |
| <34 µmol/L |
50 (78.13) |
13 (27.08) |
1 |
|
| 34-50 µmol/L |
9 (14.06) |
16 (33.33) |
2.12 [-0.94-5.17] |
0.18 |
| >50 µmol/L |
5 (7.81) |
19 (39.58) |
0.27 [-1.84-2.38] |
0.8 |
| Spleen diameter |
| ≤ 140 mm |
33 (51.56) |
19 (39.58) |
1 |
|
| >140 mm |
31 (48.44) |
29 (60.42) |
2.37 [0.78-3.96] |
0.004 |
| PV Diameter |
| ≤ 12 mm |
40 (62.5) |
29 (60.42) |
1 |
|
| >12 mm |
24 (37.5) |
19 (39.58) |
0.37 [-0.84-1.57] |
0.55 |
| PV=Portal vein, N=total number of cases, EV=esophageal varices, RR=relative risk |
Bilirubin, portal vein diameter and prothrombin time were not
significantly associated with the presence of esophageal varices.
All other markers were significantly associated with the
presence off esophageafl varfices (Table 1).
A statistically significant correlation was found between the
presence of esophageal varices and the platelet count on
spleen diameter ratio on one hand (p=0.01) and the right liver
span on albumin ration on the other hand (p=0.02).
The predictive values of the various markers were generally
low. Spleen diameter, Child Pugh score and right liver span on
albumin ratio had the highest sensitivity, specificity, positive
and negative predictive values. The area under the receiver
operation curve (AUROC) was significant only for the spleen
diameter, Child Pugh score and the right liver span on albumin
ration (Table 2).
Table 2: Predictivity of large esophageal varices.
|
Threshold |
SE |
SPE |
PPV |
NPV |
p-value (AUROC) |
| Child-Pugh score |
8 |
0,62 |
0,73 |
0,72 |
0,63 |
0,0001 (0.738) |
| Spleen diameter (mm) |
148,34 |
0,63 |
0,77 |
0,75 |
0,65 |
0,001 (0.715) |
| Platelet count (ml) |
104117 |
0,37 |
0,47 |
0,44 |
0,39 |
0,055 (<0.5) |
| PC/SD |
736 |
0,38 |
0,40 |
0,42 |
0,36 |
0,004 (<0.5) |
| Albumin (g/l) |
32,24 |
0,38 |
0,43 |
0,43 |
0,38 |
0,009 (<0.5) |
| Right liver span/albumin |
4,8 |
0,56 |
0,8 |
0,76 |
0,62 |
0,006 (0.668) |
| PC/SD=platelet count to spleen diameter ratio. SE=sensitivity; SPE=specificity; PPV=positive predictive value; NPV=negative predictive value; AUROC=area under the receiver operating curve. |
Discussion
A total of 64 patients were enrolled in the study. The sex ratio
was 1.78 (41 men against 23 women). This male preponderance
correlates with most findings both in African and Western
studies. It was reported to be 1.88 by Mouliom in 2006 [13].
The median age was 54 years old.
Viral hepatitis accounted for the majority of cases of cirrhosis
in our study, as is the case with most African series [13,14-16],
contrary to findings in western countries were alcoholic liver
diseases and metabolic diseases are more rampant [17]. As a
matter of facts, 51.6% (33 patients) had HBV related liver cirrhosis,
46.9% (30 patients) had HCV related cirrhosis and only
14.1% had alcohol related cirrhosis. The mean age at presentation
of HBV related cirrhosis was 36.41 years, with a peak within
the group of patients aged between 30-39 years. Ankouane
et al in a recent study found the mean age of patients with HBV
related hepatocellular carcinoma to be 38.5 ± 12.3 years [18].
On the otherhand, the mean age at presentation of HCV related
cirrhosis was 66.17%. Likewise, Ankouane et al reported
that most patients with hepatitis C virus related hepatocellular
carcinoma were beyond age 50 (mean 61.5 years old) [19].
Of the 64 cirrhotic patients enrolled, 46 (71.87%) presented
with decompensation. In most studies, cirrhosis is diagnosed
at decompensation with ascites being its commonest unveiling
mode [13,20-22]. This portrays the long asymptomatic characteristic
of this chronic disease. While 20.31% had their cirrhosis revealed by upper gastrointestinal bleeding, 7.81% had it
revealed by jaundice. Jaundice was not as frequent a mode of
decompensation of cirrhosis in our study compared to findings
in similar studies in other parts of Africa [20,23]. Furthermore,
none of our patients presented with hepatic encephalopathy.
In our study, esophageal varices were present in 48 patients
(75%) with 53.15% having large esophageal varices (34 patients).
Even higher rates have been reported in other African
studies [20,23]. Mouliom reported that 86% of cirrhotic patients
had esophageal varices [13]. Gastric varices were present
in 9 of our patients (14.01%) and were all gastroesophageal
varices, predominantly type 1 (77.78% of all GOV). Mouliom
reported a rate of gastric varices of 19.40% [13].
Data on the relationship between Child Pugh score and the risk
of EV is somewhat conflicting. One study showed that Child
Pugh score was an acceptable predictor of the presence of EV
[24], whereas another well designed study suggested that it
was not a useful predictor [25-27]. In our study however, 18 patients
(28.13%) were Child Pugh A, 31 patients (48.44%) Child
Pugh B and 15 patients (23.44%) Child Pugh C. Ascites was the
predominant mode of decompensation as earlier mentioned.
The relative risk increased from 1.87 to 2.86 as we moved
from patients with Child Pugh A to classes B and C respectively
(p-values of 0.006 and 0.012). This association has been described
by several authors [24,28-31]. Using the linear logistic
regression model, patients with a score greater or equal to 8
were significantly at risk of presenting high grade esophageal varfices (Table 2). Furfthermore, Chfifld Pugh score appears fto be
an independent predictor of esophageal varices on multivariate
analysis.
The mean spleen diameter in patients in our study was 142.86
mm (range: 68 mm to 240 mm). Similar high spleen diameters
have been reported by Mouliom in Cameroon and other
studies conducted in Sub-Saharan countries [13,29,31]. Spleen
diameter greater than 140 mm were 2.37 times more at risk
of having esophageal varices (p=0.004). Using the linear logistic
regression model, patients with a spleen diameter greater
148.339 mm were significantly at risk of having high grade
esophageal varices (p<0.001), with a positive predictive value
of 0.75. Splenomegaly in cirrhosis is equally an independent
predictor of esophageal varices.
The mean platelet count in our population was 109266 cells/
mm3 (range: 59000 mm3-432000 mm3). There was an inverse
correlation between platelet count and the grade of esophageal
varices which was found to be statistically significant. Patients
with platelet count less than 100000/mm3 were twice
at risk of developing esophageal varices (p value=0.013). Patients
with platelet count less than or equal to 104117 cells/
mm3 were at risk of presenting with large esophageal varices.
However, contrary to findings of other studies, this correlation
was not statistically significant (p=0.055).
Though not a marker of portal hypertension, prothrombin
level decreases with advanced liver disease (which results in
increase portal hypertension). Similarly to what has been reported
by Lahmidani in 2015 [32], there was no correlation between
prothrombin level and the grade of esophageal varices
in our study. The relative risk did not change with a drop in
prothrombin level. The mean prothrombin level in our study
was 61.21% (range 15%-99%). However a positive correlation
has been reported by some authors [33-35].
The mean serum albumin level in our population was 33.20 g/l
(range: 20.17 g/l-54 g/l). It appeared to decrease with increasing
grade of esophageal varices. As a matter of facts, the relative
risk was 2.61 for patients with an albumin level between
28 g/l and 35 g/l, while it was 1.39 for patients with an albumin
level less than 28 g/l. This finding has been equally reported by
Sarwar et al [36]. A level less or equal to 32.24 g/l in our study
had a statistically significant correlation with the presence of
large esophageal varices following the linear logistic regression
model (p=0.009). However its sensitivity and positive predictive
value were low (0.38 and 0.43) with an AUROC less than
0.5.
There was no correlation between bilirubin level and the grade
of esophageal varices. Though patients with bilirubin level between
34 and 50 μmol/L were 2.12 times more at risk of presenting
esophageal varices, this correlation was not significant
(p=0.18). A local study equally found that there was no correlation
[13].There was equally no correlation between the portal
vein diameter and the presence of esophageal varices in our
study (p-value of 0.55 for a cut off of 12 mm). Our mean portal
vein diameter was found to be 12.63 mm (range: 8 mm-21
mm). Similar findings have been reported by Wan-dong H et
al [37].
The mean platelet count on spleen diameter (PC/SD) ratio in our study was 840.82. This ratio decreased with an increase in the
size of esophageal varices using the logistic regression model,
and the correlation was statistically significant (p=0.004). This
correlation has consistently been reported by several authors
[33,38,39-41]. Patients with a ratio less or equal to 736 were
significantly at risk of having large esophageal varices, though
the sensitivity and positive predictive value were low (0.38 and
0.42). This ratio was also found to be an independent predictor
of esophageal varices on multivariate analysis (p=0.001).
The right liver span on albumin ratio has equally been reported
as a promising predictive marker of the presence of esophageal
varices [38,41]. The mean ratio in our study was 4.4574
and it significantly correlated with the presence and grade of
esophageal varices (p=0.017). A ratio greater or equal to 4.8
was significantly predictive of high grade esophageal varices
(p=0.006), with a sensitivity of 0.56 and a positive predictive
value of 0.76 (AUROC=0.67). This is equally found to be an
independent predictor of esophageal varices on multivariate
analysis (p=0.02).
Conclusion
Cirrhosis predominantly affects adult male patients, and is
mostly associated to chronic viral hepatitis. Child Pugh score,
spleen diameter, platelet count on spleen diameter and right
liver span on albumin ratios were independent predictors of
esophageal varices. Portal vein diameter and bilirubin level
were not significantly associated with the presence of esophageal
varices. Voluntary screening programs will help diagnose
liver disease an early stage and prevent the occurrence
REFERENCES
- Bosch J, Abrades GJ, Berzigotti A, Garcia-Pagan JC (2008) Portal hypertension and gastrointestinal bleeding. Semin Liver Dis. 28(1):3-25
[Crossref] [Google Scholar] [PubMed]
- Bosch J, Garcia-Tsao G (2010) Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 362(9):823-32
[Crossref] [Google Scholar] [PubMed]
- R De Franchis (2005) Evolving consensus in portal hypertension: Report of the Bevano IV workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 43(1):167-76
[Crossref] [Google Scholar] [PubMed]
- Cales P, Desmorat H, Vinel JP, Caucanas JP, Ravaud A, et al. (1990) Incidence of large esophageal varices in patients with cirrhosis: Application of prophylaxis of first bleeding. Gut.31(11):1298-1302
[Crossref] [Google Scholar] [PubMed]
- Crott R, Makris N, Barkun A, Fallone C (2022) The cost of an upper gastroduodenal endoscopy: An activity-based approach. Can J Gastroenterol. 16(7):473-482
[Crossref] [Google Scholar] [PubMed]
- Mandeville KL, Krabshuis J, Ladep NG, Mulder CJJ, Quigley EMM, et al. (2009) Gastroenterology in developing countries: Issues and advances. World J Gastroenterol. 15(23):2839-2854
[Crossref] [Google Scholar] [PubMed]
- Arroyo V, Ginès P, Gerbes AL, Dudley FJ, GentiliniP, et al. (1996) Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome. International ascites club. Hepatology.23:164-176
[Crossref] [Google Scholar] [PubMed]
- Conn H, Bircher J (1994) Hepatic encephalopathy syndrome and therapies. Medi-Edi Press. Bloomington 1-12
[Crossref] [Google Scholar] [Research Gate]
- Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, William R (1973) Transection of the esophagus for bleeding esophageal varices. Br J Surg. 60(8):646-9
[Crossref] [Google Scholar] [PubMed]
- Lamb PM, Lund A, Karagasabay RR, Martin A, Webb JA, et al. (2002) Spleen size: How well do lineal ultrasound measurement correlate with three-dimensional CT volume assessment? Br J Radiol. 75:573-7
[Crossref] [Google Scholar] [PubMed]
- Garcia-Tsao G, Sanyal AJ, Norman DG, William C (2007) Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 46(3):922-938
[Crossref] [Google Scholar] [PubMed]
- Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK (1992) Prevalence, classification and natural history of gastric varices: A long-term follow-up study in 568 portal hypertension patients. Hepatology. 16:1343-1349
[Crossref] [Google Scholar] [PubMed]
- Mouliom Tapouh JR, Njoya O, Monabang Zoé C, Moifo B, Kowo M, et al. (2015) Approche non endoscopique du diagnostic des varices oesophagiennes d’origine cirrhotique dans une population d’Afrique noire subsaharienne. Health Sci Dis. 16(3); 1-5.
[Google Scholar] [Research Gate]
- Blankson A, Wiredu EK, Gyasi RK, Adjei A, Tettey Y (2005) Seroprevalence of hepatitis B and C in cirrhosis of the liver in Accra, Ghana. Ghana Med J. 39(4):132-137
[Google Scholar] [PubMed] [Research Gate]
- Baba MM, Ajayi BB, Ekanem IA (2000) Prevalence of hepatitis B surface antigen among patients suspected of liver disease in a Nigerian hospital. Niger Postgrad Med J. 7(3):91-5
[Google Scholar] [PubMed] [Research Gate]
- Hoffmann CJ, Thio CL (2007) Cinical implications of HIV and hepatitis B co-infection in Asia and Africa. Lancet Infect Dis. 7:402-409.
[Crossref] [Google Scholar] [PubMed]
- Nada L, Samira EF, Bahija B, Adil I, Nourdine A (2015) Noninvasive predictors of presence and grade of esophageal varices in viral cirrhotic patients. Pan Afr Med J. 20:145
[Crossref] [Google Scholar] [PubMed]
- Ankouane AF, Kowo M, Talla P, Medjo EH, Djapa R, et al. (2013) Epidemiology of hepatitis B virus-associated hepatocellular carcinoma in Cameroon. Health Sci Dis. 14(1):16-19
[Research Gate]
- Ankouane AF, Noah ND, Djapa R, Kowo M, Talla P, et al. (2014) Epidemiology of hepatitis C: Related hepatocellular carcinoma in Cameroon. Pan Afr Med J. 19:379
[Crossref] [Google Scholar] [PubMed]
- Diarra M, Konaté A, Soukho A, Dicko M, Kallé A, et al. (2010) Aspects évolutifs de la maladie cirrhotique dans un service d’hépatogastroentérologie au Mali. Mali Médical. 25(1):42-46
[Google Scholar]
- Karoui S, Hamzaoui S, Sahli F, Matri S, Boubaker J, et al. (2002) Mortality in cirrhosis: Prevalence, causes and predictive factors. Tunis Med. 80(1):21-5
[Google Scholar] [PubMed]
- Pariente A (2006) Decompensation ascitique. Gastroenterol Clin Biol. 30:870-874
[Crossref] [Google Scholar] [PubMed]
- Maiga MY, Diallo F, Traoré HA, Traoré AK, Guindo A, et al. (2002) Valeur diagnostique de l’endoscopie digestive haute au cours de la cirrhose. Acta Endoscopica. 32(2):211-215
[Crossref] [Google Scholar] [Research Gate]
- Thabut D, Trabut JB, Massard J, Rudler M, Muntenau M, et al. (2006) Non-invasive diagnosis of large esophageal varices with fibrotest in patients with cirrhosis: A preliminary retrospective study. Liver Int. 26(3): 271-278
[Crossref] [Google Scholar] [PubMed]
- Qamar AA, Grace ND, Groszmann RJ, Garcia-Tsao G, Bosch J, et al. (2008) Platelet count is not a good predictor of the presence or development of gastroesophageal varices in cirrhosis. Hepatology. 47(1):153-9
[Crossref] [Google Scholar] [PubMed]
- Rajvanshi P, Kowdley KV (2002) Prediction of varices in patients with cirrhosis. A high stakes number of game? J Clin Gastroenterol. 34(1):4-5
[Crossref] [Google Scholar] [PubMed]
- Attia KA, N’dri-yoamn TH, Talla P, Bathaix YF, Mahassadi A, et al. (2003) Facteurs prédictifs des signes endoscopiques d’hypertension portale sévère chez le cirrhotique en milieu africain: Etude de 131 cas. Médecine d'Afrique. 50(3):109-114
[Google Scholar]
- Sharma SK, Aggarwal R (2007) Prediction of large esophageal varices in patients with cirrhosis of the liver using clinical, laboratory and imaging parameters. J Gastroenterol Hepatol. 22(11):1909-1915
[Crossref] [Google Scholar] [PubMed]
- Thompoulos KC, Labropoulou-Karatza C, Mimidis KP, Katsakoulis EC, Iconomou G, et al. (2003) Non-invasive predictors of the presence of large esophageal varices in patients with cirrhosis. Dig Liver Dis. 35(7):473-478
[Crossref] [Google Scholar] [PubMed]
- Cherian JV, Deepak N, Ponnusamy RP, Somasundanam A, Jayanthi V (2011) Non-invasive predictors of esophageal varices. Saudi J Gastroenterol. 17(1):64-68
[Crossref] [Google Scholar] [PubMed]
- Chang MH, Sohn JH, Kim TY, Son BK, Kim JP, et al. (2007) Non-endoscopic predictors of large esophageal varices in patients with liver cirrhosis. Korean J Gastroenterol. 49(6): 376-83
[Google Scholar] [PubMed] [Research Gate]
- Dib N, Konate A, Oberti F, Calès P (2005) Noninvasive diagnosis of portal hypertension in cirrhosis: Application to primary prevention of varices. Gastroenterol Clin Biol. 29(10):975-87.
[Crossref] [Google Scholar] [PubMed]
- Schepis F, Cammà C, Niceforo D, Magnano A, Pallio S, et al. (2001) Which patients with cirrhosis should undergo endoscopic screening for esophageal varices detection? Hepatology. 33:333-338.
[Crossref] [Google Scholar] [PubMed]
- Giannini E, Botta F, Bomo P, Risso D, Romagnoli P, et al. (2003) Platelet count/spleen diameter ratio : Proposal and validation of a noninvasive parameter to predict the presence of oesophageal varices in patients with liver cirrhosis. Gut. 53:1200-1205.
[Crossref] [Google Scholar] [PubMed]
- Sarwar S, Khan AA, Alam A, Butt AK, Shafqat F, et al. (2005) Non-endoscopic predictors of the presence of esophageal varices in cirrhosis. J Coll Physicians Surg Pak, 15:528-531.
[Crossref] [Google Scholar] [PubMed]
- Wan-don H, Qi-huai Z, Zhi-ming H Xiang-Rong C, Zen-Cai J, et al. (2009) Predictors of esophageal varices in patients with hepatitisB virus-related cirrhosis: A retrospective study. BMC Gastroenterol. 9:11
[Crossref] [Google Scholar] [PubMed]
- Esmat S, Omam D, Rashid L (2012) Can we consider the right hepatic lobe/albumin ratio a noninvasive predictor of esophageal varices in hepatitis C virus-related liver cirrhotic Egyptian patients? Eur J Intern Med. 23(3):267-72.
[Crossref] [Google Scholar] [PubMed]
- Schwarzenberger E, Meyer T, Golla V, Sahdala NP, Min AD (2010) Utilisation of platelet count spleen diameter ratio in predicting the presence of esophageal varices in patients with cirrhosis. J Clin Gastroenterol. 44(2):146-150.
[Crossref] [Google Scholar] [PubMed]
- Barikbin R, Hekmatnia A, Omidifar N, M Farghadani, P Adibi (2010) Prediction severity of esophageal varices: A new cut-off point for platelet count/spleen diameter ratio. Minerva Gastroenterol Dietol. 56(1):1-6.
[Google Scholar] [PubMed] [Research Gate]
- Ying L, Lin X, Xie ZL, Hu YP, Shi KQ (2012) Performance of platelet count/spleen diameter ratio for the diagnosis of esophageal varices in cirrhosis: A meta-analysis. Dig Dis Sci. 57(6):1672-1681.
[Crossref] [Google Scholar] [PubMed]
- Alempijeric T, Bulat V, Djuranovic S, Kovacevic N, Jesic R, et al. (2007) Right liver lobe/albumin ratio: A contribution to non-invasive assessment of portal hypertension. World J Gastroenterol. 13(40):5331-5335.
[Crossref] [Google Scholar] [PubMed]
Citation: Roger NDG, Mathurin KP, Galdima M, Wilson NNA, Paul T, et al. (2022) Non-Invasive Predictors of Large Esophageal Varices in Patients with Cirrhosis in Cameroon. J Clin Gastroenterol Hepatol. 6:20.
Copyright: © Roger NDG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.