Case Report - (2017) Volume 18, Issue 6
Koji Kubota, Ataru Nakayama, Hitoshi Masuo, Kaori Takasu, Fumitoshi Karasawa, Nobumichi Takeuch
Department of Surgery, Ina Central Hospital, 1313-1 Koshirokubo, Ina, Nagano 396-8555, Japan
Received Date: October 10th, 2017; Accepted Date: November 1st, 2017
Xanthogranulomatous pancreatitis is an extremely rare histological subset of pancreatitis characterized by chronic destructive granulomatous inflammation. Here, we report a 23-year-old man who was found to have xanthogranulomatous pancreatitis complicated by pancreas pseudocysts that infiltrated into spleen, stomach, transverse colon and omentum. The lesion persisted through medical treatments such as dietary modification, pharmacotherapy, and endoscopic intervention. Though this is benign entity, only radical resection as a last resort cut off a chain reaction of inflammation of xanthogranulomatous pancreatitis.
Pancreatectomy; Pancreatitis
IPMT intraductal papillary mucinous tumor; XGI xanthogranulomatous inflammation; XGP xanthogranulomatous pancreatitis
Xanthogranulomatous inflammation (XGI) is a rare pathologic entity with characteristic macroscopic and microscopic features [1]. XGI is destructive inflammatory disease affected multiple organs. Most XGIs occur in the kidney [2] and gallbladder [1, 3, 4], but the other sites such as the breast [5], intracranium [6], gastrointestinal tract [7, 8], genital organs [9], bone [10], and skin [11] were reported. XGI to the pancreas, the xanthogranulomatous pancreatitis (XGP) is an extremely rare disease. Over the past decades, only 19 cases of xanthogranulomatous pancreatitis were reported in the English literature [12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27]. We herein report a case of progressive XGP, where the inflammation infiltrated into the stomach, transverse colon and spleen.
A Twenty-three-year-old Japanese man was admitted to our hospital for episodes of acute upper abdominal pain. He was diagnosed with acute pancreatitis caused by main pancreatic duct stones. The abdominal computed tomography (CT) scan on admission showed pancreatic stones in main pancreatic duct as well as duct dilation and enlarged pancreas head (Figure 1a). There was no past medical history nor family history of the pancreatic disease. He denied alcohol use. He was referred to University hospital for extracorporeal shock wave lithotripsy (ESWL) for stone removal followed by Endoscopic Retrograde Cholangio- Pancreatography (ERCP) with pancreatic duct stenting. He underwent total eight times of ESWL and pancreatic stones in main pancreatic duct were removed (Figure 1b). Within next two years from initial treatment, he came back total three times with pancreatitis by radiological evident pancreatics stones. ERCPs were performed same manner and stones were removed (Figures 2a, 2b). However four months after the last episode of stone pancreatitis, he developed another pancreatitis without evidence of stone in the main pancreatic duct. The pancreatic pseudocysts were evident at that time, and dilation of pancreatic duct vanished (Figure 3). The serum amylase and pancreatic-amylase level were high as 615IU/ℓ (standard value:43-116 IU/ℓ) and 587 IU/ℓ (18-53 IU/ℓ) respectively. And amylase level in the urine was also elevated as 8,604 IU/ℓ (<500 IU/ℓ). Complete blood count (CBC) and Comprehensive metabolic panel with fasting glucose (CMP) were within normal limits. The mutations of all pancreatitis-associated gene CPA1 [28] was negative, and the IgG 4 level was within normal limit. We initiated medical treatment (pancreatin, camostat mesylate, trimethadione, bromhexine hydrochloride, esomeprazole magnesium hydrate) and dietary restrictions (only Elental 480g/day or fast cure). The follow up abdominal CT scan after four months, however, showed multiple pseudocysts at the tail of the pancreas that infiltrated into stomach, colon, and spleen without stone at main pancreatic duct (Figure 4). Meantime his symptom had been on and off. Six months later, follow up CT scan showed ill-defined low-density area developed adjacent to pseudocysts that involved the stomach, transverse colon, and spleen. The border between pancreas and stomach became unclear (Figure 4). Esophagogastroduodenoscopy (EGD) showed hypertrophic mucosa with poor distensibility of the posterior gastric wall suggested inflammation from pancreatitis, and pancreatic pseudocysts involved stomach (Figure 5). Further restricted dietary treatment with total parental nutrition and pain management with NSAIDs and pentazocine hydrochloride were initiated but failed shortly after. At that point, we finally decided to perform a surgical intervention. Initially, our plan was to perform distal pancreatectomy with possible splenectomy, since we recognized the lesion was benign and attempted to preserve as many adjacent organs as possible. However, the whole lesion that include part of the transverse colon, spleen and the large portion of stomach was palpate like a solid mass and only en bloc resection appeared to be an option. The entire posterior walls of the stomach and transverse colon as well as spleen were severely adhered to the pancreas. We ended up to perform distal pancreatectomy up to superior mesenteric vein with splenectomy, partial resection of transverse colon with primary anastomosis and total gastrectomy with Rouxen Y reconstruction (Figure 6). Gross examination of the specimen revealed the rupture of main pancreatic duct led to 5.0 cm pancreas pseudocysts with the thick wall made of dense fibrosis. The pancreas itself and pancreatic pseudocyst infiltrated to the stomach, spleen and transverse colon (Figure 7). Histopathologic examination of the pancreatic tail specimen showed extensive fibrosis and infiltration of numerous foamy histocytes with scattered eosinophil, neutrophils, lymphocytes, plasma cells, indicating XGI (Figure 8). The XGI lesion infiltrated into not only the pancreas parenchyma but also adjacent organs such as the stomach, transverse colon, and spleen. His postoperative course was uneventful, and he was discharged on the 22nd post-operative day. After 3 years of follow up, he is in good health without any symptom.
Figure 1: (a). Abdominal CT at first visit to our hospital showed pancreatic stone at main pancreatic duct, main pancreatic duct (MPD) dilation, and moderate enlarged pancreas head. Asterisks indicate MPD stone, arrows indicate MPD dilation. (b). He underwent ESWL 8 times; Left panel; MPD stone obstructed MPD. Right panel; after ESWLs 8 times, pancreatic stones at MPD were completely removed.
Figure 2: (a). He has relapsed into pancreatitis after ten months of initial treatment. Left panel; MPD stones were appeared. Right panel; MPD stones were removed again. (b). After 8 months, he had a recurrence of pancreatitis. MPD stones were removed and drainage of MPD was performed. Arrows indicate MPD stone.
Figure 3: Abdominal CT after four months of treatment third pancreatitis revealed that the pancreas pseudocysts at the pancreatic tail, around of stomach and spleen without the pancreatic stone at main pancreatic duct. Dilation of pancreatic duct vanished. Asterisks indicate pseudocyst, arrows indicate.
Figure 4: (a). Follow up abdominal CT after one month showed multiple pseudocysts at the tail of the pancreas that are extended into stomach, colon, and spleen. (b, c). Ill-defined low-density area developed around pancreas and pseudocysts involved the stomach, transverse colon, and spleen. The borders between the lesion and the pancreas, stomach, transverse colon and spleen were unclear. Sharps indicate stomach. Asterisks indicate transverse colon. Arrows indicate pseudocyst.
Figure 6: Surgical figures: Pancreas firmly adhered to spleen, stomach, transverse colon and omentum. Due to extensive infiltration, we had to performed radical resection include distal pancreatectomy up to superior mesenteric vein with splenectomy, total gastrectomy with Roux-en Y reconstruction and partial resection of transverse colon with primary anastomosis.
Figure 8: Microscopic examination revealed extensive fibrosis and infiltration of numerous foamy cells along with scattered lymphocytes and plasma cells are noted. (a). Hematoxylin and Eosin stain (HE) ×20, (b). ×100, (c). ×600. high-power view of foamy histocytes with clear lipid-containing cytoplasm. (d). Schmorl stain; Pale blue cells are foamy cells. Blue immediate iron.
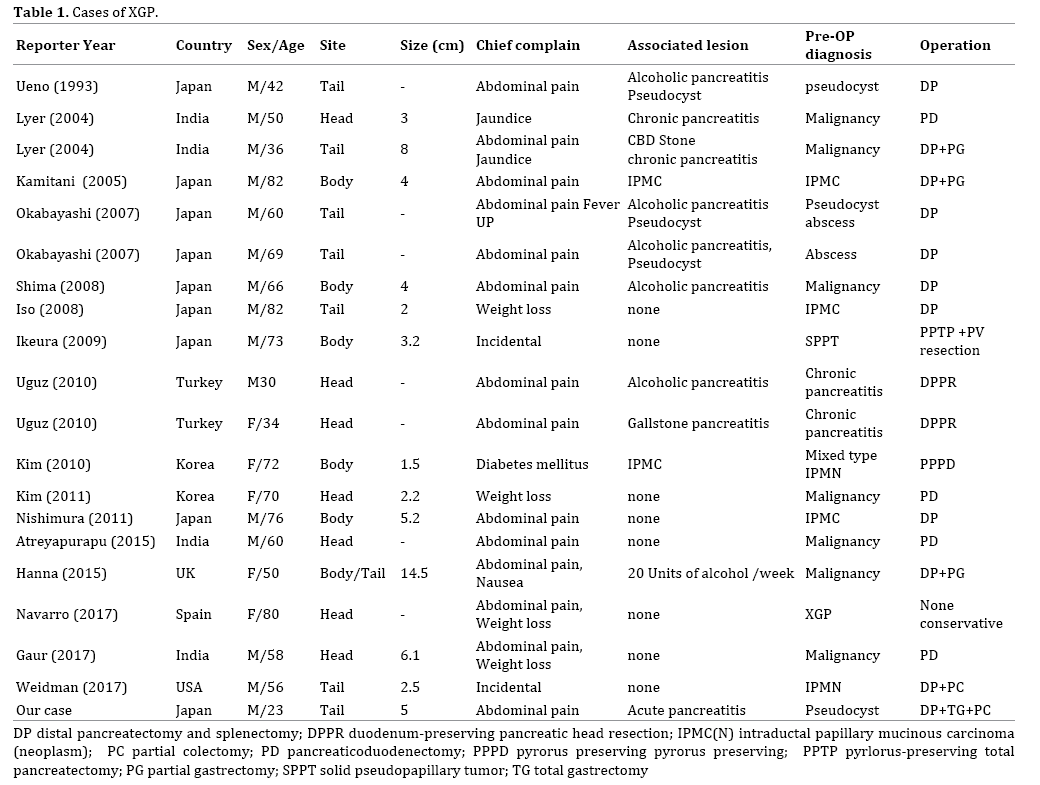
We reported a twenty-three-year-old man who was found to have an extremely rare entity, XGP complicated by pancreas pseudocysts infiltrated into spleen, stomach, transverse colon and omentum. Originally Goodman et al. reported that XGI is characterized by chronic mixed inflammatory process that contains varying amounts of foamy histiocytes, inflammatory cells, fibrous reaction and sometimes accompanied by multinucleated giant cells [1]. The characteristic processes of XGP include destruction and effacement of the normal structures of the affected organ and often mimic the neoplastic process. XGI itself is also a rare condition which has been well documented mainly in the gallbladder [1, 3, 4] and kidney [2]. XGI occurs in the pancreas is so rare that only 19 cases have been reported in the English literature since Ueno et al. reported the first case of XGP in 1993 [12]. According to 20 case reports include our case (Table 1) [12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27], their median age was 60 year (23-82), XGP occurs mainly in male patients (M:F; 15:5), the locations were evenly distributed in the pancreas (head: body: tail; 7: 6: 8). In most cases, patients presented with symptoms such as abdominal pain (14 cases, 68%) and weight loss (4 cases). Only 2 cases were diagnosed by accidental findings. The majority of cases (13/20; 65%) were misdiagnosed as a neoplasm by preoperative imaging (13/20; 65%).
The exact etiology of XGP is unknown; duct obstruction, infection and hemorrhage trigger such as XGI of gallbladder and kidney. Kim et al. reported mucin produced by intraductal papillary mucinous tumor (IPMT) increased the intraductal and intracystic pressure and that a leakage of mucin into the pancreatic parenchyma produced the xanthogranulomatous changes [20]. Iyer et al. suggested that obstruction to pancreatic ducts by stones followed by secondary bacterial infection initiated the xanthogranulomatous pancreatitis without cystic lesion [13]. Ueno et al. reported that a pseudocyst formed by acute alcoholic pancreatitis and, after relapse attacks, infection and hemorrhage occurred in the pseudocyst. That elevated intracystic pressure and caused secondary xanthogranulomatous change to the pancreatic cyst wall [12]. In our case, extensive pancreatic stones caused pancreatic duct obstruction and the subsequent development of longstanding pancreatitis, which might cause xanthogranulomatous change in the pancreas.
Weidman et al. reported that the peculiarity of the imaging of XGP is very helpful for proper preoperative diagnosis [27]. Of note, all cases except one underwent surgery due to either preoperative diagnosis as malignant or failure of medical treatment. Although the ill-defined lesions appeared around pseudocysts by the follow up CT scan, we kept treating the lesion as the benign due to the fact the patient presented as pancreatic stone induced pancreatitis. Thus, we did not pursue further diagnostic imaging nor biopsy but we might have done endoscopic ultrasound guided biopsy for confirmation that the lesion was benign. Six cases included our case (6/20; 30%) underwent surgery despite the fact that preoperative diagnosis was benign [12, 15, 19]. In these cases of XGP, they had had intractable abdominal pain for a long period of time (Average 17.8 M; 1-36 M) and persisted through medical management such as low-fat diet and pharmaceutical management. Navarro et al. avoided surgery by making the diagnosis through biopsy and reported the effectiveness of medical therapy and pharmaceutical intervention [25]. In our case, it is demonstrated that his disease overall resisted for all various treatments such as dietary treatment (low-fat diet), pharmacotherapy (antibiotic, proteinase inhibitor, NSAIDs and pentazocine hydrochloride) and endoscopic therapy (remove pancreatic calculus exploited ESWL and drainage of the MPD) for total two years four months period. Only surgical intervention can cut off a chain reaction of inflammation of XGP for pancreas and its adjacent organs. However, due to the fact that both XGI and XGP are not neoplastic entities, there is always room for debate regarding surgical intervention. In our case, the intention to avoid pancreatectomy for two years four months allows XGP to progress and end up with radical resection include total gastrectomy. Fortunately, our case has been making good progress after the surgery, and his lifestyle has been improved. He drinks alcohol occasionally post operation but no recurrence of pancreatitis for almost three years.
In summary, we report a 23-year-old man who was found to have XGP complicated by pancreas pseudocysts infiltrated into spleen, stomach, transverse colon and omentum. Although we applied multidisciplinary approach, only radical resection of the involved area reached remission of the disease. Further knowledge is warranted to establish the treatment strategy for this rare, complicated pancreatitis.
The authors declare that they have no competing interests.