Research Article - (2025) Volume 22, Issue 1
Medication Discrepancies Identified During Medication Reconciliation in Patients in a Medium-Sized Hospital
Paula Carneiro Ramalho1*,
Waleria de Paula2,
Lucas da Silva Braga2,
Andrea Grabe Guimaraes2 and
Renata Cristina Rezende Macedo do Nascimento2
1Department of Pharmacy, Federal University of Ouro Preto, Minas Gerais, Brazil
2Department of Pharmaceutical Sciences, Federal University of Ouro Preto, Ouro Preto, Minas Gerais, Brazil
*Correspondence:
Paula Carneiro Ramalho, Department of Pharmacy, Federal University of Ouro Preto, Minas Gerais,
Brazil,
Email:
Received: 07-Sep-2023, Manuscript No. IPDEHC-23-17688;
Editor assigned: 11-Sep-2023, Pre QC No. IPDEHC-23-17688 (PQ);
Reviewed: 25-Sep-2023, QC No. IPDEHC-23-17688;
Revised: 16-Jan-2025, Manuscript No. IPDEHC-23-17688 (R);
Published:
23-Jan-2025, DOI: 10.36648/2049-5471.22.1.57
Abstract
Objective: To analyze (evaluate) the Medication Discrepancies (MD) in prescriptions of patients during a Medication Reconciliation (MR) service at admission to the Medical Unit.
Methods: A cross-sectional study was conducted from March 2021 to February 2022, in a medium-sized hospital of Minas Gerais state, Brazil. Patients aged 18 years or older and under continuous use of at least one medication at the moment of hospital admission were included. The first MR service interview was preferably conducted within 24 hours and should take place until 48 hours of admission. Socio-demographic data, health indicators, detailed information about home pharmacotherapy, and information of potential medication discrepancies were collected. The pharmaceutical care data and medical records were analysed using Stata 13.0 software. Pearson's Chi-square test was performed for the statistical analyses (significance 5%). The study was approved by the research ethics committee of the Universidade Federal de Ouro Preto (CEP)/UFOP under number 4.845.642.
Results: The majority of the 215 patients included were female (n=115; 53.5%), mean age of 68 ± 18 years, and patients aged ≥ 65 years (n=131; 61.0%) were prevalent. The mean number of medicines being used at the moment of hospital admission was 6 ± 3, and poly pharmacy was identified in 128 (59.5%) patients. The most prevalent comorbidities were diabetes mellitus and hypertension and the presence of at least one of these two comorbidities was observed in 80.0% of the patients (n=172). The variables age group (p=0.005), polypharmacy (p<0.001), having hypertension and/or diabetes mellitus (p=0.001), hospitalization for infectious and parasitic diseases (p<0.001) and circulatory system diseases (p=0.040) have a significant relation to the occurrence of at least one MD in prescriptions. Drugs used in diabetes mellitus (p<0.001), agents acting on the renin-angiotensin system (p=0.028), lipid-modifying agents (p=0.026), medications for obstructive airway diseases (p=0.001), general nutrients (p=0.005) and thyroid hormone medications (p=0.002) were associated with unintentional MD.
Conclusion: It was possible to identify a significant percentage of MD in the prescription evaluated. Poly pharmacy and age group were related to the occurrence of MD.
Keywords
Medication; Discrepancies; Hospital; Patients; Diabetes mellitus
Introduction
Patient safety is characterized by reducing the risk of unnecessary harm associated with health care [1]. Considering that the appropriate use of essential medicines is one of the most cost-effective components of health care, the World Health Organization (WHO) launched its third global challenge in 2017 entitled "Medication without Harm". Its statement included the goal of reducing potential harms related to medication use [2]. This challenge addresses priority actions with emphasis on high-risk situations, polypharmacy, and communication failures in management of health care [3,4].
Many medication errors are due to the patient omission of a medication at the moment of hospital admission and communication failure among health professionals by the care transition, compromising patient safety and treatment effectiveness [5]. Taken together, these factors can trigger permanent damage to the health and well-being of the patient, from hospital admission to the other stages of the care transition, corresponding to the most frequent cause of compromised patient safety and the emergence of problems related to the use of medications (DRP) [6,7]. The main role of the pharmacist is to evaluate the necessity, effectiveness and safety of medicines, identifying, preventing and solving the DRP [8]. The professional performance relies on using research tools and the best as possible information of the patient medication history, in order to provide care to the patient, their family and community, reducing adverse drug events and promoting patient safety [9].
Patient-centred care involves respecting the beliefs, expectations, experiences, attitudes, and concerns of the patient or caregivers regarding their health conditions and the use of medicines. Thus, the pharmacist and patient share decision-making and responsibility for health outcomes. In the hospital setting, pharmacists work into multidisciplinary teams, aiming to adequate pharmaco-therapeutic follow-up and resolution of DRP that may arise during treatment, in order to provide safer care to the patient [10]. Medication Reconciliation (MR) is a pharmaceutical service to prevent medication errors resulting from medication discrepancies, such as duplication or medications omissions, especially when the patient goes through different levels of care or different health services. The main objective is to promote rational use of medicines, establish efficient communication and ensure the correct given information to other health professionals. The clinical pharmacist intervenes to prevent and solve problems in drug therapy, in order to guarantee pharmacotherapeutic treatment success, as well as the promotion, protection and recovery of health and other problems in order to provide a better quality of life. These services generate better and more accurate results in medication reconciliation, being part of the integral assistance to inpatients. Thus, this study aimed to analyze the medication discrepancies identified in prescriptions of patients admitted at the medical unit of a medium-sized hospital, during the medication reconciliation service.
Materials and Methods
The procedures adopted in this study are in accordance with the ethical principles in research (ref). Data collection and analysis were approved by the Research Ethics Committee of the Universidade Federal de Ouro Preto (CEP)/UFOP under opinion number 4.845.642. This was a cross-sectional study, carried out from March 2021 to February 2022, conducted in a medium-sized hospital in the unconfident’s region, Minas Gerais state, Brazil. The study population consisted of patients attended by the MR pharmaceutical service, aged 18 years or older and who were in continuous use of at least one medication at the time of hospitalization in the Medical Unit. This was a hospital sector for adult patients with clinical diagnoses and treatment of diseases without surgical procedures demand. Patients unable to respond about their home pharmacotherapy due to some disability or whose relative or caregiver did not have information about pharmacotherapy, were excluded [11].
The first interview of the MR services was carried out preferably within 24 hours after hospital admission and may take place within 48 hours of admission. During the interview, sociodemographic data, health indicators and detailed information about home pharmacotherapy were collected. At the bedside pharmaceutical care, the patient medication history information was collected and the reconciliation of the continuous medicines used with the medicines prescribed during the hospital stay was performed. The differences between the list of the patient continuous use medications identified at the hospital admission and the hospital prescription were called discrepancy, classified as intentional (suspended use based on the clinical situation, suspended use due to therapeutic duplicity, change of posology or administration frequency, dose change and change of administration route) or unintentional (omission of medication use).
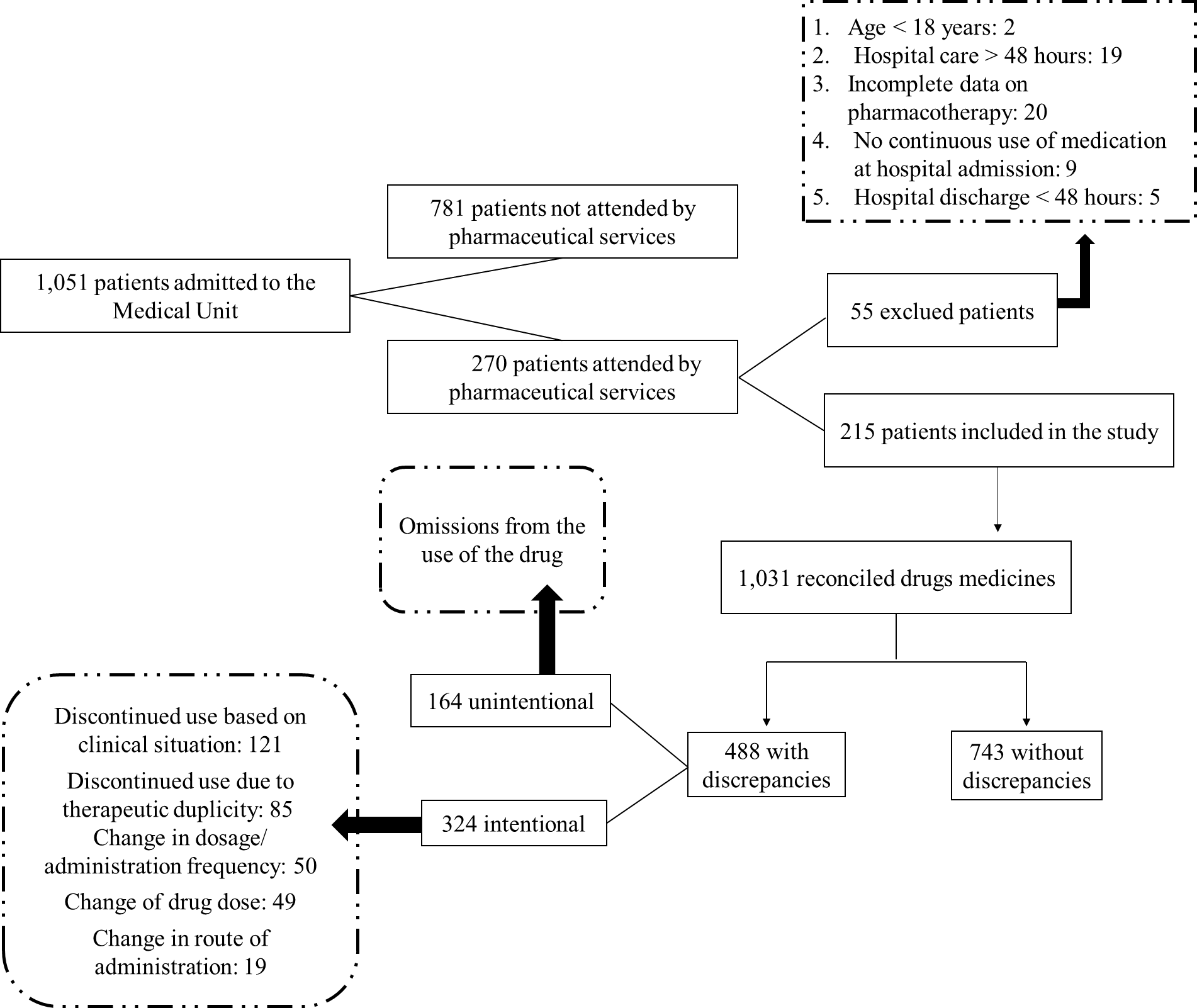
During the study period, 1,051 patients were admitted for hospitalization in the medical unit sector. From those 270 (25.7%) were attended by the clinical pharmaceutical service of MR. However, 55 patients met the exclusion criteria of the study, resulting in 215 patients (20.5%) included in this study (Figure 1).
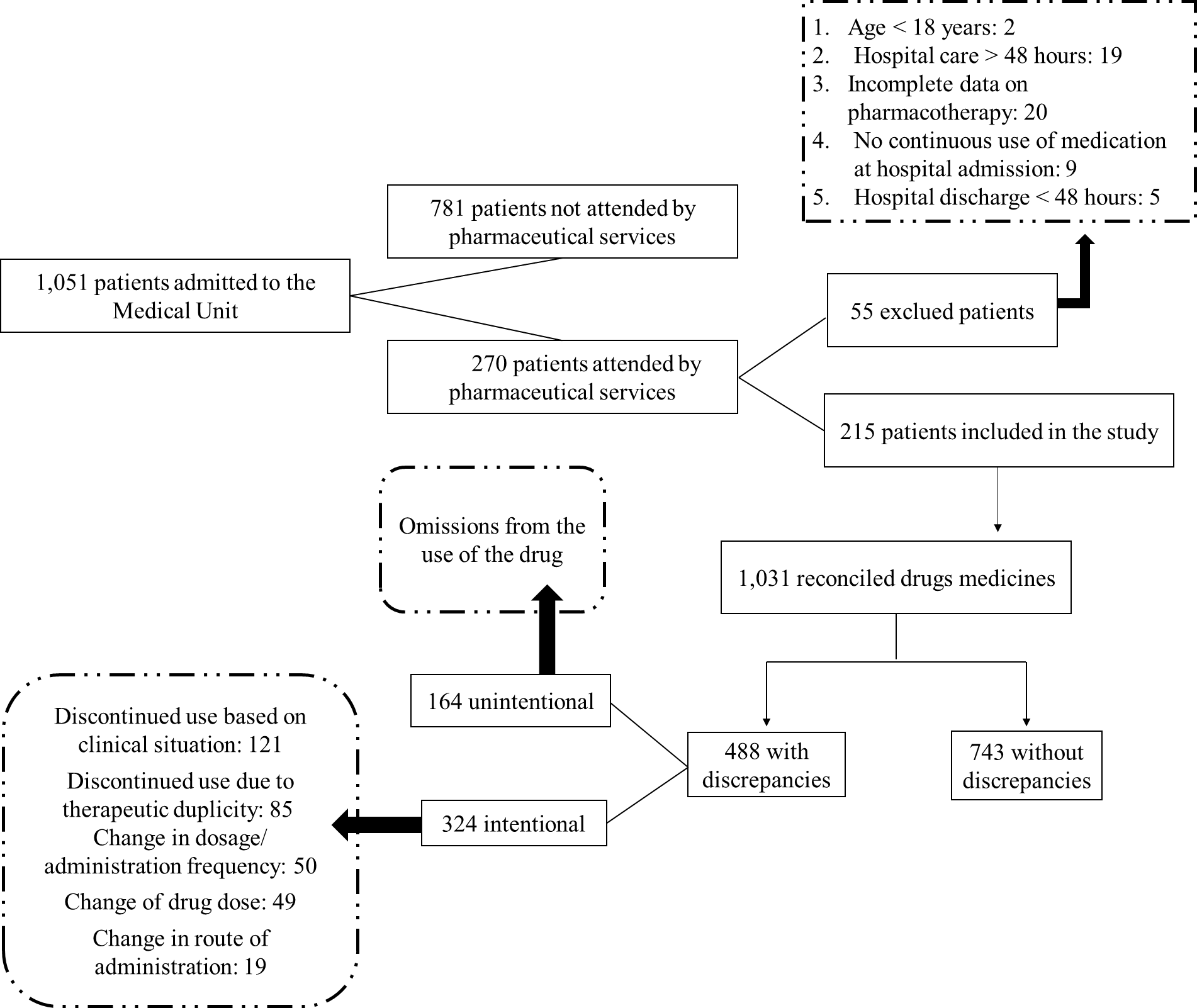
Figure 1: Patients were admitted for hospitalization in the medical unit sector.
The outcome variable was the occurrence of MD identified by pharmacists during MR. The population was characterized by socio-demographic variables (gender/sex, age group, time and type of hospitalization), health indicators (history of drug allergy, comorbidities, hospitalization dyagnosis) and profile of medicines used at hospital admission. Polypharmacy was defined as the concomitant use of five or more medicines, by the same patient [12]. The medicines were described according to the Brazilian Common Denomination (DCB) and classified according to the second and fifth level of the Anatomic Therapeutic Chemical (ATC).
The descriptive and statistical analyses were performed in Stata 13.0 software. To assess the correlation between MD and explanatory variables, Pearson's Chi-square test was performed. The statistical significance threshold was 5%.
Results and Discussion
From the 215 patients attended by the clinical pharmaceutical service of MR, the majority were female (n=115; 53.5%), mean age of 68 ± 18 years, with patients aged ≥ 65 years (n=131; 61.0%) being the most prevalent. The majority of hospitalizations occurred in Brazilian unified health system (SUS) beds (90.7%; n=195). The mean length of hospital stay was 8 ± 7 days and 61.9% of patients (n=133) had a maximum of 7 days of hospitalization. Previous drug allergy was reported by 15.3% of patients (n=33). The mean number of medicines used at the hospital admission was 6 ± 3 and poly pharmacy was identified in 59.5% (n=128) of patients. The most prevalent comorbidities were diabetes mellitus and hypertension and the presence of at least one of these two comorbidities was observed in 80.0% (n=172) of patients. The most prevalent hospitalization diagnoses, according to ICD-10 chapters, were certain infectious and parasitic diseases (n=66; 30.7%), circulatory system diseases (n=45; 20.9%) and genitourinary system diseases (n=22; 10.2%). Among these, the most prevalent ICD-10 was B34.2: Coronavirus infection of unspecified location (27.4%; n=59), under Chapter (Table 1).
|
Chapters
|
Codes
|
Description
|
n
|
%
|
|
I
|
A00-B99
|
Certain infectious and parasitic diseases
|
66
|
30,7
|
|
IX
|
I00-I99
|
Diseases of the circulatory system
|
45
|
20,9
|
|
XIV
|
N00-N99
|
Diseases of the genitourinary system
|
22
|
10,2
|
|
X
|
J00-J99
|
Diseases of the respiratory system
|
31
|
14,4
|
|
IV
|
E00-E90
|
Endocrine, nutritional and metabolic disorder
|
10
|
4,7
|
|
XI
|
K00-K93
|
Other diseases of the digestive system
|
8
|
3,7
|
|
V
|
F00-F99
|
Mental and behavioural disorders
|
8
|
3,7
|
|
|
|
Other hospitalization diagnoses
|
25
|
11,6
|
|
|
|
Total
|
215
|
100
|
Table 1: Hospitalization diagnoses of patients attended by the medication reconciliation service of a medium-sized hospital in Minas Gerais, Brazil, according to ICD-10 chapters, from March 2021 to February 2022.
The variables age group (p=0.005), polypharmacy (p<0.001), having at least one of the two most prevalent comorbidities, hypertension or diabetes mellitus (p=0.001), hospitalizations for infectious and parasitic diseases (p<0.001), and circulatory system disease (p=0.040) were significantly related to the occurrence of at least one MD in prescriptions (Table 2).
|
Variables
|
Patients seen by the medication reconciliation service
|
|
n
|
%
|
MD** n (%)
|
p
|
|
Gender
|
0.505
|
|
Male
|
100
|
46,5
|
77 (77,0)
|
|
|
Female
|
115
|
53,5
|
84 (73,0)
|
|
|
Age group
|
0.005
|
|
18 to 44 years
|
26
|
12
|
15 (57,7)
|
|
|
45 to 64 years
|
58
|
27
|
38 (65,5)
|
|
|
≥ 65 anos
|
131
|
61
|
108 (82,4)
|
|
|
Type of hospitalization
|
0.273
|
|
SUS
|
195
|
90,7
|
144 (73,9)
|
|
|
Health plan
|
20
|
9,3
|
17 (85,0)
|
|
|
Length of stay
|
0.649
|
|
1 a 7 dias
|
133
|
61,9
|
101 (75,9)
|
|
|
≥ 8 dias
|
82
|
38,1
|
60 (73,2)
|
|
|
History of drug allergy
|
0.237
|
|
No/Does not know
|
182
|
84,7
|
139 (76,4)
|
|
|
Yes
|
33
|
15,3
|
22 (66,7)
|
|
|
Polypharmacy
|
<0.001
|
|
No
|
87
|
40,5
|
50 (57,5)
|
|
|
Yes
|
128
|
59,5
|
111 (86,7)
|
|
|
People with systemic hypertension and/or diabetes mellitus
|
0.001
|
|
No
|
43
|
20
|
24 (55,8)
|
|
|
Yes
|
172
|
80
|
137 (79,7)
|
|
|
Presence of a companion
|
0.258
|
|
No
|
74
|
34,4
|
52 (70,3)
|
|
|
Yes
|
141
|
65,6
|
109 (77,3)
|
|
|
Certain infectious and parasitic diseases (Chapter I)*
|
<0.001
|
|
No
|
163
|
75,8
|
133 (81,6)
|
|
|
Yes
|
52
|
24,2
|
28 (53,9)
|
|
|
Diseases of the circulatory system (Chapter IX)*
|
0.04
|
|
No
|
170
|
79,1
|
122 (71,8)
|
|
|
Yes
|
45
|
20,9
|
39 (86,7)
|
|
|
Diseases of the genitourinary system (Chapter XIV)*
|
0.429
|
|
No
|
193
|
89,7
|
143 (74,1)
|
|
|
Yes
|
22
|
10,2
|
18 (81,8)
|
|
|
Diseases of the respiratory system (Chapters X)*
|
0.924
|
|
No
|
184
|
85,6
|
138 (75,0)
|
|
|
Yes
|
31
|
14,4
|
23 (74,2)
|
|
|
CID: Other chapters*
|
0.139
|
|
No
|
150
|
69,8
|
108 (72,0)
|
|
|
Yes
|
65
|
30,2
|
53 (81,5)
|
|
|
Note: Absolute, relative values and threshold for statistical significance was p values ≤ 0.05. *Chapters according to ICD-10; **MD: Medication Discrepancy
|
Table 2: Bivariate analysis of the occurrence of medication discrepancies in prescriptions evaluated by the MR services (n=215) in the Medical Unit sector of a medium-sized hospital in relation to socio-demographic characteristics and health indicators, March 2021 to February 2022.
According to Pereira et al., in a population-based study, it was observed polypharmacy and sociodemographic characteristics revealed association with female gender and elderly above 80 years, and that regardless of socioeconomic variables a higher prevalence of polypharmacy is related to female gender. This could be related to the fact that women commonly are more careful and concerned about their health than men. A retrospective cohort study conducted with inpatients in the surgical clinic sector in a teaching hospital, between 2014 and 2018, in a city of Alagoas state, Brazil, observed that from 338 patients included in the study, 187 (55.3%) had MD identified at the first prescription after hospital admission. Female patients were the most prevalent and the most frequent type of MD was medication omission (93.0%). Additionally, they observed association of MD with comorbidities (p=0.000) and elderly patients aged 60 years or older (p=0.007), but not associated with hospitalization [13]. These findings corroborate the results of the present study, demonstrating that length of stay is not related to the occurrence of MD, but that group age and comorbidities suggesting that the elderly may be a risk factor for the occurrence of MD on hospital admission. Thus, it was highlighted that the elderly should be prioritized regarding the MR services after hospital admission in order to reduce potential damage by pharmacotherapy. A narrative literature review on MR performed in the elderly pointed out the existence of a positive association between the numbers of medicines used by the patient and the rate of discrepancies, being the omission of medications the predominant type of discrepancy [14]. Our results also corroborate these findings, demonstrating a significant relationship between poly pharmacy and the presence of MD. The type of unintentional discrepancy due to omission of medications can be a worrying factor when collecting a patient medication history at the moment of hospital admission. Taking this difficulty to account, the MR service demonstrates optimization and rationalization of the patient pharmacotherapy aimed at patient safety and reduction of Adverse Drug Events (ADE) in the care transition process ref. Unintentional MD are related to un-intentionality of the prescriber to not prescribe a medicine that is part of home pharmacotherapy or to change prescription on admission by information omission [15]. An observational study in the cardiology unit of a large hospital identified 50.4% of the 117 discrepancies as the unintentional type, with omission of medications being the most prevalent. Chung et al., conducted a study in the cardiology department of a hospital in France and observed 544 MD and also omission as the most frequent (70.1%), arising from different causes during the information transfer process. An uncontrolled study conducted in Spain for one year in a hospital and three basic health units, identified MD in 143 patients, and it was necessary 228 MR for 126 patients [15]. The main type of discrepancy was that patients were not taking medicines listed in their active medical records (n=152; 58.7%) [16]. It was possible to resolve the MD of the 126 patients by reducing the number of medicines in use per patient, reducing hospital admissions and there was association with greater economic and social accessibility [17]. Another cross-sectional study in a clinical unit of a public hospital in southern Brazil identified that 94.0% of the interviewed patients had at least one DM [18]. In the present study, the amount of medication in use at the time of hospital admission can be characterized as poly pharmacy, and the prevalent type of DM as unintentional by omission. These data corroborate the aforementioned study, and demonstrate worrying factors for the health team, given the difficulty in managing drug therapy in light of their comorbidities and clinical situation that led to hospitalization. The MR had a positive impact on health care, showing that patients treated by the service have up to 20% less chances of being readmitted for a hospitalization [19]. In this context, MR services is an effective strategy for identification of MD and that the omission, when identified in the pharmacotherapeutic analysis, allows the occurrence of avoidable clinical consequences, increasing patient safety.
A total of 1,231 medicines were reconciled, of which 488 (39.6%) had MD on prescription at the time of hospital admission. The most frequent pharmacological classes among MD were drugs used in the treatment of diabetes mellitus (n=72; 14.8%), diuretics (n=58; 11.9%), and agents with action on the renin angiotensin system (n=40; 8.2%). Among these, 324 (66.4%) had an intentional discrepancy (Chart 1). Of the 488 reconciled medications that had MD, 33.6% (n=164) had a discrepancy of the unintentional type caused by omission of medicine use. Regarding intentional discrepancies, suspended use based on clinical situation (n=121; 24.8%), suspended use due to therapeutic duplicity (n=85; 17.4%), alteration of dosage/frequency of administration (n=50; 10.2%), alteration of drug dose (n=49; 10.0%), and alteration of route of administration (n=19; 3.9%) were identified.
The most common therapeutic classes in unintentional DM due to omissions were lipid-modifying agents (n=16; 21.9%), followed by antithrombotic agents (n=13; 12.4%) and diuretics (n=13; 9.50%). The most common drugs for unintentional DM were simvastatin (C10AA01–n=6), fenofibrate (C10AB05–n=5), acetylsalicylic acid (B01AC06–n=10) and furosemide (C03CA01 n=8). Medicines used in Diabetes Mellitus (p<0.001), agents acting on the renin-angiotensin system (p=0.028), lipid modifying agents (p=0.026), medicines for obstructive airway diseases (p=0.001), general nutrients (p=0.005) and thyroid hormone medicines (p=0.002) were associated with unintentional MD (Table 2). In the study by Barboza da Silva et al., considering the analysis of medicines in ATC level 1, it was described as most present drugs those acting on the cardiovascular system. The study of Gai observed that the classes of psychoanaleptics (17.5%), followed by diuretics (15.8%) and medicines for acid disorders (12.3%) were the most involved in the omissions and the medicines most involved in the omissions were omeprazole, followed by citalopram. In the present study, it was observed that the drugs losartan, simvastatin and fenofibrate were the most present in the cardiovascular system, second only to levothyroxine.
In the study by Oñatibia-Astibia et al. the drug groups with the greatest discrepancy were drugs for obstructive airway diseases (R03; 8.3%, n=19), psychoanaleptics (N05; 8.3%, n=18) and anti-inflammatory products and nonsteroidal antirheumatics (M01A; 7.5%, n=17). Through this, it is possible to observe that it was suggested that patients on drug therapies at the cardiovascular level are a population at risk for DM and therefore should be prioritized for the MR services. The variety of drugs cited among the studies that showed a correlation between the therapeutic classes with the onset of DM can be explained by the location where the study was carried out, reinforcing the need to characterize the population and the profile of the drugs used, so that the health team can fully assist in the management of pharmacotherapies in order to reduce adverse effects to medications and therapeutic ineffectiveness due to the absence of medication use. The predominant classes of medicines that presented unintentional MD indicate the correlation with the comorbidities hypertension and diabetes mellitus, demonstrating the need for special attention to these patients, who are more susceptible to the occurrence of MD in prescription. Hospitalizations for infectious and parasitic diseases were the most frequent type of hospitalization due to the period of the study occurring in times of pandemics by the new Coronavirus infection. Thus, the MR services and the patient care process, by proposing measures to reduce risks and mitigate adverse events, collaborate to strengthen the Brazilian Patient Safety Program and the WHO´s global challenge to assure medication without harm. That’s why knowledge of the profile of medicines used by patients is an essential strategy to reduce medication errors during transitions of health care (Table 3).
| Second level of ATC |
Description |
Reconciled medications |
Unintentional MD |
| Omission |
| N |
% |
n (%) |
P |
| C03 |
Diuretics |
137 |
11,1 |
13 (9,50) |
0,161 |
| A10 |
Drugs used in diabetes |
124 |
10,1 |
4 (3,2) |
<0,001 |
| C09 |
Agents acting on the renin–angiotensin system |
118 |
9,6 |
8 (6,8) |
0,028 |
| B01 |
Antithrombotic agentes |
105 |
8,5 |
13 (12,4) |
0,767 |
| C07 |
Beta blocking agentes |
80 |
6,5 |
8 (10,0) |
0,366 |
| N03 |
Antiepileptics |
77 |
6,3 |
10 (13,0) |
0,929 |
| C10 |
Lipide modifying agente |
73 |
5,9 |
16 (21,9) |
0,026 |
| N06 |
Psychoanaleptics |
65 |
5,3 |
5 (7,69) |
0,170 |
| N05 |
Psycholeptics |
63 |
5,1 |
8 (12,7) |
0,881 |
| C08 |
Calcium channel blockers |
53 |
4,3 |
6 (11,3) |
0,661 |
| A02 |
Drugs for acid related disorders |
38 |
3,1 |
8 (21,1) |
0,154 |
| R03 |
Drugs for obstructive airway diseases |
38 |
3,1 |
12 (31,6) |
0,001 |
| V06 |
General nutrientes |
34 |
2,8 |
10 (29,4) |
0,005 |
| H03 |
General nutrientes |
32 |
2,6 |
10 (31,3) |
0,002 |
| OTC |
Other classes on the second level of ATC |
194 |
15,8 |
33 (17,0) |
0,100 |
| |
Total |
1031 |
|
164 |
|
| Note: Threshold for statistical significance was p values ≤ 0.05 |
Table 3: Bivariate analysis of the frequencies of medications reconciled (n=1231) by the MR service according to unintentional discrepancies caused by medication omissions, in the Internal Medicine sector of a medium-sized hospital, Brazil, March 2021 to February 2022.
Conclusion
It was possible to identify a significant percentage of MD in the prescription evaluated. Poly pharmacy and age group were related to the occurrence of MD.
References
- World Health Organization (2019) Medication safety in transitions of care: Technical report. Biblioteca responsável.
[Google Scholar]
- Sheikh A, Dhingra-Kumar N, Kelley E, Kieny MP, Donaldson LJ (2017) The third global patient safety challenge: Tackling medication-related harm. Bull World Health Organ. 95(8):546.
[Google Scholar] [PubMed]
- Galvin M, Jago-Byrne MC, Fitzsimons M, Grimes T (2013) Clinical pharmacist’s contribution to medication reconciliation on admission to hospital in Ireland. Int J Clin Pharm. 35:14-21.
[Crossref] [Google Scholar] [PubMed]
- Lombardi NF, Mendes AE, Lucchetta RC, Reis WC, Favero ML, et al. (2016) Analysis of the discrepancies identified during medication reconciliation on patient admission in cardiology units: A descriptive study. Rev Lat Am Enfermagem. 24:e2760.
[Crossref] [Google Scholar] [PubMed]
- Schuch AZ, Zuckermann J, Santos MEF, Martinbiancho JK (2013) Medication reconciliation upon admission to a pediatric oncology unit. Rev Bras Farm Hosp Serv. 4:35–39.
- Silva DA, Mendonca SD, Oliveira DR, Chemello C (2018) Clinical practice of pharmacists in family health Support team. Work Educ Health. 16(2):659-682.
[Google Scholar]
- DE Lima Ed, DA Silva RG, Ricieri MC, Blatt CR (2017) Clinical pharmacy in a hospital environment: focus on recording activities. Rev Bras Farm Hosp Serv Saúde. 8(4).
[Google Scholar]
- dos Santos SL, da Silva Alves HH, Pessoa CV, Saraiva HS (2018) Evidence of pharmaceutical care in oncology clinical practice. Magazine of the Faculty of Medical Sciences of Sorocaba. 20(2):77-81.
[Google Scholar]
- Brazilian Society of Clinical Pharmacy, “Origin of Clinical Pharmacy in Brazil, its development, related concepts and perspectives Brasília,” Sbfc, p. 17, 2019
- Rezende R, Alvares J, Guerra AA, Gomes IC, Silveira MS (2017) Polypharmacy: A reality in primary care of the Unified Health System. J. Public Health. 51(suppl.2):19.
- Pereira KG, Peres MA, Iop D, Boing AC, Boing AF, et al. (2017) Polypharmacy in the elderly: A population-based study. Braz J Epidemiol. 20(02):335-344.
[Google Scholar]
- Al-Khashan HI, Almulla NA, Galil SA, Rabbulnabi AA, Mishriky AM (2012) Gender differences in health education needs and preferences of Saudis attending Riyadh Military Hospital in the Kingdom of Saudi Arabia. J Family Community Med. 19(3):172-177.
[Crossref] [Google Scholar] [PubMed]
- Menezes KB, Silva AS, Cunha-Mattos CE, Nutels T, Oliveira AD, et al. (2021) Association between medication discrepancies and length of hospital stay in the surgical clinic of a university hospital. Rev Bras Farm Hosp Serv Saude. 12(2):547.
[Google Scholar]
- Campos PL, Reis AM, Martins MA (2013) Medication reconciliation in the elderly: a literature review. Geriatr Gerontol Aging. 7(2):146-151.
- Santos CO, Lazaretto FZ, Lima LH, Azambuja MS, Millao LF (2019) Medication reconciliation: Implementation process in a hospital complex using an electronic system. Health in Debate. 43:368-377.
[Google Scholar]
- Chung C, Gauthier V, Marques-Tavares F, Hindlet P, Cohen A, et al. (2019) Medication reconciliation: predictors of risk of unintentional medication discrepancies in the cardiology department. Arch Cardiovasc Dis. 112(2):104-112.
[Crossref] [Google Scholar] [PubMed]
- Onatibia-Astibia A, Malet-Larrea A, Mendizabal A, Valverde E, Larranaga B, et al. (2021) The medication discrepancy detection service: A cost-effective multidisciplinary clinical approach. Aten Primaria. 53(1):43-50.
[Crossref] [Google Scholar] [PubMed]
- Da Silva TB, Alves-Zarpelon SP, Laureano JV (2021) Medication reconciliation in an inpatient unit of a public hospital in southern Brazil. Infarma-Pharm Sci. 33(2):158-166.
[Google Scholar]
- Redmond P, Grimes TC, McDonnell R, Boland F, Hughes C, et al. (2018) Impact of medication reconciliation for improving transitions of care. Cochrane Database Syst Rev. (8).
[Crossref] [Google Scholar] [PubMed]
Citation: Ramalho PC, de Paula W, da Silva Braga L, Guimaraes AG, do Nascimento RCRM (2025)
Medication Discrepancies Identified During Medication Reconciliation in Patients in a Medium-Sized Hospital. Divers Equal
Health Care. 22:57.
Copyright: © 2025 Ramalho PC, et al. This is an open-access article distributed under the terms of the Creative
Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided
the original author and source are credited.