Routine collection of more detailed data is key to improving knowledge. What is not recorded cannot be proven, and what cannot be proven cannot be addressed.
Introduction
A prerequisite for effective action in all social policy development is the availability of evidence. The introduction of any system of quality assurance or output management itself generates change. That which is measured can be aimed at; that which is left unobserved can be ignored. We live in an era of ‘evidencebased practice’, and collection of accurate and appropriate information has become more important than ever for the development of improved policies and practices in the health system. When dealing with the health and well-being of socially excluded and relatively powerless groups, access to such data assumes even greater importance.
In the USA, a crucial legacy of the Civil Rights Movement of the 1960s and 1970s was the introduction of ethnic record keeping and monitoring in all federally supported activities, in order to ensure contract compliance and the specifications of the 1964 Civil Rights Act. More recently, the US Department of Health and Human Services, under the authority of the Patient Protection and Affordable Care Act (the healthcare reforms signed into law by President Obama in March 2010), has published revised standards for data collection on race, ethnicity, gender, primary language and disability status (US Department of Health and Human Services, 2011). However, across most of Europe, and indeed the rest of the world, detailed, comprehensive and accurate information on the health of migrants, ethnic minorities or other ‘vulnerable’ groups is lacking (Rafnsson and Bhopal, 2009; Rechel et al, 2011; Kraler and Reichel, 2010; World Health Organization, 2011).
Equality and diversity monitoring can help to:
• build reputation
• improve productivity
• recruit and retain the best employees
• create awareness
• provide specific adjustments, training or interventions
• identify and address any inequalities
•avoid risk, including damaging and costly legal cases or negative publicity.
What needs to be measured?
The key dimensions of inequality, whatever they are deemed to be in a local or national setting, will need to be monitored. The precise factors will depend on local legislation and aspiration, but should include the protected characteristics laid out in the EU Treaties, Human Rights Acts or the local equivalent. Examples of categories or factors might include the seven strands ofUK policy defined in theUK Equality Act (see below). In states where there are indigenous disadvantaged populations (e.g. Canada, Australia, the USA), groups should include ‘First Nation’ or Aboriginal status.
Effective monitoring is a legal requirement of the UK Equality Act 2010 (Section 149), which sets out a public-sector equality duty in relation to the following protected characteristics:
• age
• disability
• gender reassignment
• marriage/civil partnership status
• pregnancy and maternity
• race, including ethnic or national origins, colour or nationality
• religion or belief, including lack of belief
• gender
• sexual orientation.
Civil status and carer responsibilities are other possible themes to be considered.
What are the arguments against monitoring?
One of the most common arguments against monitoring is that the recording of data may breach human rights to privacy, or risk exposing minorities to the adverse effects of discrimination. It is also suggested that it may be illegal in some jurisdictions.
The European Data Protection Directive (Directive 95/46/EC 24.10.1995) regulations state (with good reason, in view of the experiences of the 1939–1945 Holocaust and more recent ethnic cleansing events) that ‘personal data must (only) be collected for specified, explicit and legitimate purposes.’ Furthermore, Article 8 makes it clear that:
Member states shall prohibit the processing of personal data revealing racial or ethnic origin, political opinions, religious or philosophical beliefs, trade union membership and ... data concerning health or sex life.
(Directive 95/46/EC 24.10.1995)
Further sub-sections of the Directive go on to explain that data may be collected when the subject gives ‘explicit consent’, or where such data are necessary to ensure compliance with employment law, or when public interest (e.g. public health concerns) dictates that such data are necessary and assurance is available that the rights and safety of the individual will be safeguarded (see Johnson, 2008).
Other objections include the belief that it is discriminatory to ask such personal questions, or that people will refuse to participate and thus the monitoring may create barriers to service uptake. The cost and time involved in asking for additional information have also been suggested as reasons for not introducing equality monitoring (www.civitas.org. uk/press/prequalityimpact.htm), but there are no detailed analyses of the cost of introducing monitoring, which is usually added when other systems are revised. Consequently, the cost of gathering data for monitoring is likely to be minimal. There is indeed a business case for diversity and equality initiatives. Some major enterprises have reported a link between good diversity practice and overall business performance, including improved productivity (Procter andGamble), cost savings (British Telecom), and better marketing through a more diverse team (Cadbury Schweppes) (Rutherford and Ollerearnshaw, 2002).
Some staff may be embarrassed to ask questions which they describe as ‘sensitive.’ All health services require very sensitive data on age, private behaviours and relationships, and the confidentiality and necessity of such data are seldom questioned. Once they are embedded in records, these data need not be requested again, except for occasional audit. Questions about ‘ethnicity origin’ can uncover the risk of certain inherited conditions, such as sickle-cell anaemia, which provides a clinical justification for them (Aspinall et al, 2003; Dyson et al, 2007).
How common and how effective is ‘ethnic’ or other diversity monitoring?
Despite a long tradition and legal mandate for such data in the USA, the levels of monitoring remain surprisingly variable. The Centers for Disease Control National Electronic Telecommunications System for Surveillance (NETSS) found that 59% of cases were missing race data and 40% were missing ethnicity data in Massachusetts. Data on gender and age, on the other hand, were complete in 95–99% of cases (Chen et al, 2003).
At present, in Europe, disease-specific populationbased registers with data on ethnicity or migrant status are available only in Germany, England, Scotland and Sweden (for a limited number of conditions). Germany and Sweden register data only on country of birth, not on ethnicity. However, data on healthcare utilisation allowing for some identification of migrants at national or regional levels were found to be available in 11 of the 27 EU member states (Nielsen et al, 2009). In every case this included some utilisation data on hospital care, but only a few countries collected data on care in outpatient settings.
How and what do you ask?
The best indicator to collect is the one most closely related to the factors believed to drive inequities. Choice is often limited by political or ideological constraints, and one variable may have to be used as a proxy for another. Country of birth is often used as a proxy for ethnicity because it is conflated with nationality, but both may be very unreliable in former colonial powers such as the UK, France, Spain, Portugal, Belgium, the Netherlands or Italy. Members of colonial populations and the children of colonists born aboard may be entitled to citizenship and residence in the mother country even if they do not wish to take up these options. Patterns of migration are in a constant state of change, and the children of migrants may have dual nationality.
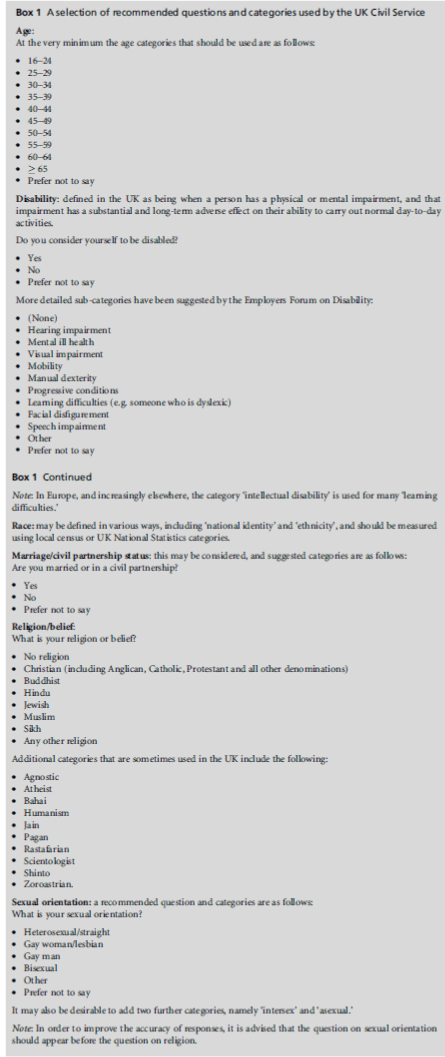
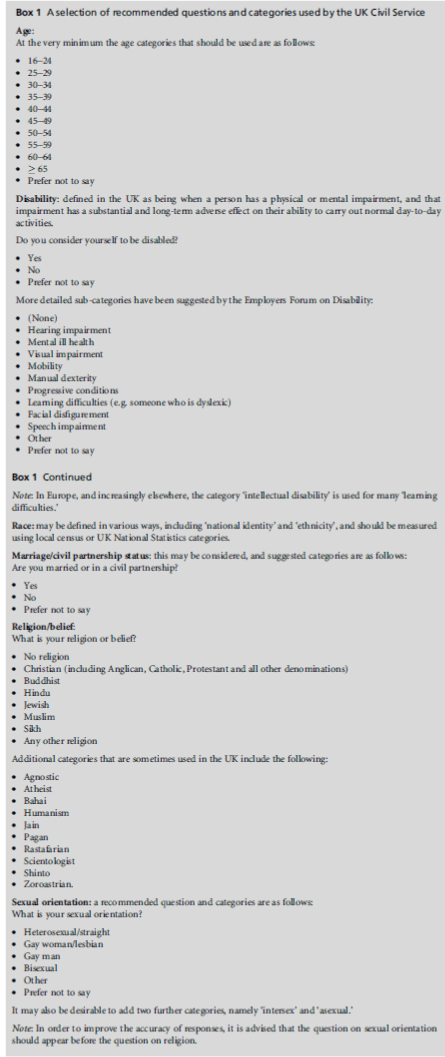
Labels may not be particularly helpful. For example, ‘Indian or British Indian (Asian)’ includes the possibility of membership of at least four major language groups (Punjabi, Hindi, Gujerati or Urdu), or many minor language groups, such as Malayalam, spoken by more recent, ‘high-skilled’ workers, many of whom are also fluent in English, the lingua franca of India. ‘Indian’ people also belong to all of the world’s main faiths (including Christianity, Islam, Sikhism and Buddhism, as well as Judaism), many but not all are vegetarian, and while some groups eschew alcohol, and others avoid tobacco, local cultural groups providemany exceptions to an ‘ethnic stereotype.’ Similarly, although the vast majority of people of ‘Pakistani’ or ‘Bangladeshi’ heritage in theUKare Muslim and speak Urdu (or a Kashmiri dialect thereof), or the Sylheti dialect of Bengali, respectively, there are many exceptions. What is required is some kind of agreed baseline (see Box 1).
Conclusion: key factors in equality monitoring
• The existence of ‘Champions’ (i.e. political leadership and ownership) along with support from communities, managers and staff is a key factor. Most important of all, however, is political acceptance of the value and necessity of the data.
• Agreement on the value of any data for clinical or policy purposes and the factors to be measured (whether migration origin, citizenship status, ethnicity, language or faith) is essential, and can be supported by reference to research.
• An understanding of the best place in the ‘patient journey’ to make the initial enquiry, and a way to record it so that data, while kept securely, can also be shared between relevant agencies so as to reduce the necessity for repeated requests.
• Standardised questions that can be utilised in and compared across national systems are desirable, and enable local data to be related to national or regional patterns.
• Data need to be tied to policies such as targets and expectations relating to equity or fairness and incentives, or penalties for non-compliance, and to action plans.
• Examples of good practice, or pilot projects which can be used to demonstrate both the feasibility and utility of the process, are needed
• Finally, it is essential that once the data have been collected (even if they were initially flawed in terms of quality or coverage) they are analysed and used to make changes or justify policy actions, and to allocate resources to demonstrate their value (including the risks of non-collection).
REFERENCES AND FURTHER READING
- Ahdieh L and Hahn RA (1996) Use of the terms ‘raceâ€Âââ€Å¾Â¢, ‘ethnicityâ€Âââ€Å¾Â¢, and ‘national originsâ€Âââ€Å¾Â¢: a review of articles in the American Journal of Public Health, 1980–1989. Ethnicity and Health 1:95–8.
- Aspinall PJ, Dyson SM and Anionwu EN (2003) The feasibility of using ethnicity as a primary tool for antenatal selective screening for sickle cell disorders: pointers from the research evidence. Social Science and Medicine 56:285– 97.
- Baker P and Eversley J (eds) (2000) Multilingual Capital: the languages of London schoolchildren and their relevance to economic, social and educational policies. London: Battlebridge.
- Bardsley M, Hamm J, Lowdell C et al (2000) Developing Health Assessment for Black and Minority Ethnic Groups: analysing routine health information. London: East London &The City Health Authority for Health of Londoners Project, NHS Executive.
- Bhopal RS (2006) Race and ethnicity: responsible use from epidemiological and public health perspectives. Journal of Law, Medicine and Ethics 3:500–7.
- Chen J, Etkind P, Coman G et al (2003) Eliminating missing race/ethnicity data from a sexually transmitted disease case registry. Journal of Community Health 28:257–65.
- Department of Health (2007) A Practical Guide to Ethnic Monitoring in the NHS and Social Care. London: Department of Health. https://bit.ly/yLuILX (accessed 20 October 2012).
- Dyson SM, Chambers K, Gawler S et al (2007) Lessons for intermediate- and low-prevalence areas in England from the Ethnicity Questions and Antenatal Screening for sickle cell/thalassaemia (EQUANS) study. Diversity in Health and Social Care 4:123–35.
- European Commission (2008) Regulation (EC) No. 763/ 2008 of the European Parliament and of the Council of 9 July 2008 on Population and Housing Censuses. Brussels: European Commission. https://eur-lex.europa.eu/LexUri Serv/LexUriServ.do?uri=CELEX:32008R0763:EN:HTML (accessed 20 October 2012).
- Fischbacher C (2005) Ethnic Monitoring Tool. Edinburgh: NHS Health Scotland. www.isdscotland.org/isd/files/ ETHNIC%20MONITORING%20TOOL.pdf (accessed 20 October 2012).
- Ingleby D (2009) European Research on Migration and Health. Background Paper for IOM project ‘Assisting Migrants and Communities (AMAC): Analysis of Social Determinants of Health and Health Inequalities.â€Âââ€Å¾Â¢ Geneva: International Organization for Migration. https://bit.ly/ Al2mld (accessed 20 October 2012).
- Iqbal G, Gumber A, Szczepura A et al (2008) Improving Ethnic Data Collection for Statistics of Cancer Incidence, Management, Mortality and Survival in the UK. Warwick Medical School Report to Cancer Research UK. Coventry: Warwick Medical School Clinical Trials Unit. https:// bit.ly/xBIGNf (accessed 20 October 2012).
- Jayaweera H (2010) Health and Access to Health Care of Migrants in the UK. London: Race Equality Foundation. Johnson MRD (1998) Ethnic monitoring: bureaucratic construction of a minority entity or identity. In: Williams C, Soydan H and Johnson M (eds) Social Work and Minorities. London: Routledge. pp. 79–90.
- Johnson MRD (2001) Ethnic monitoring and nursing. In: Culley L and Dyson S (eds) Ethnicity and Nursing Practice. London: Palgrave Macmillan. pp. 91–106.
- Johnson MRD (2008) Making difference count: ethnic monitoring in health (and social care). Radical Statistics 96:38–45.
- Johnson MRD and Gill P (1995) Ethnic monitoring and equity: collecting data is just the beginning (editorial). British Medical Journal 310:890.
- Jones M and Kai J (2007) Capturing ethnicity data in primary care: challenges and feasibility in a diverse metropolitan population. Diversity in Health and Social Care 4:211–20.
- Knight M, Kurinczuk JJ, Spark P et al (2009) Inequalities in maternal health: national cohort study of ethnic variation in severe maternal morbidities. British Medical Journal 338:1–7.
- Kraler A and Reichel D (2010) Statistics on Migration, Integration and Discrimination in Europe. PROMINSTAT Final Report. Brussels: European Commission.
- Lin SS and Kelsey JL (2000) Use of race and ethnicity in epidemiologic research: concepts, methodological issues, and suggestions for research. Epidemiologic Reviews 22: 187–202.
- McKenzie K and Crowcroft N (1996) Describing race, ethnicity, and culture in medical research. British Medical Journal 312:1054.
- Makkonen T (2007) European Handbook on Equality Data. Brussels: European Commission, Directorate-General for Employment, Social Affairs and Equal Opportunities. https://ec.europa.eu/employment_social/ fundamental_rights/pdf/pubst/stud/hb07_en.pdf (accessed 20 October 2012). NHS Information Centre (2008) National Diabetes Audit (2006–2007). Leeds: NHS Information Centre. www.ic. nhs.uk/nda (accessed 20 October 2012).
- Nielsen SS, Krasnik A and Rosano A (2009) Registry data for cross-country comparisons of migrantsâ€Âââ€Å¾Â¢ healthcare utilization in the EU: a survey study of availability and content. BMC Health Services Research 9:210.
- Public Health Sector Group (2000) Ethnicity Profiling in Primary Care: the Princes Park Health Centre model. Liverpool: Public Health Sector Group, School of Health and Human Sciences, Liverpool John Moores University.
- Rafnsson S and Bhopal RS (2009) Large-scale epidemiological data on cardiovascular diseases and diabetes in migrant and ethnic minority groups in Europe. European Journal of Public Health 19:484–91.
- Rechel B, Mladovsky P, DevilleWet al (2011) Migration and Health in the European Union. European Observatory on Health Systems and Policies Series. Maidenhead: Open University Press.
- Rutherford S and Ollerearnshaw S (2002) The Business of Diversity: how organisations in the public and private sectors are integrating equality and diversity to enhance business performance. London: Schneider-Ross www. schneider-ross.com/wp-content/uploads/2012/07/The- Business-of-Diversity-with-cover.pdf (accessed 20 October 2012).
- US Department of Health and Human Services (2011) Final Data Collection Standards for Race, Ethnicity, Primary Language, Sex, and Disability Status Required by Section 4302 of the Affordable Care Act. Washington, DC: US Department of Health and Human Services. https:// minorityhealth.hhs.gov/templates/browse.aspx?lvl= 2&lvlid=208 (accessed 20 October 2012).
- World Health Organization (2011) Interim Second Report on Social Determinants of Health and the Health Divide in the WHO European Region. Copenhagen: WHO Regional Office for Europe. https://bit.ly/yT0gFo (accessed 20 October 2012).
ADDITIONAL USEFUL WEBSITES
- Balarajan M, Gray M and Mitchell M (2011) Monitoring Equality: developing a gender identity question. Equality and Human Rights Commission Research Report 75. London: Equality and Human Rights Commission. www.equalityhumanrights.com/uploaded_files/research/ rr75_final.pdf (accessed 18 October 2012).
- Equality and Human Rights Commission (undated) Equality Policies, Equality Training and Monitoring. www.equalityhumanrights.com/advice-and-guidance/ guidance-for-employers/equality-policies-equalitytraining- and-monitoring (accessed 18 October 2012).
- Equality Challenge Unit (2008) Monitoring Disability Equality. www.ecu.ac.uk/inclusive-practice/monitoringdisability- equality (accessed 18 October 2012).
- Fulton R (2010) Ethnic Monitoring: is health equality possible without it? Better Health Briefing Paper 21. London: Race Equality Foundation. www.better-health.org.uk/briefings/ ethnic-monitoring-health-equality-possible-without-it (accessed 18 October 2012).
- NHS Employers (2009) Monitoring for Equality and Diversity: what healthcare employers need to know and do. www.nhsemployers.org/Aboutus/Publications/Pages/ moitoring-briefing.aspx (accessed 18 October 2012).
- NHS Equality Delivery System (2011) Various documents. www.eastmidlands.nhs.uk/about-us/inclusion/eds (accessed 18 October 2012). NHS Information Centre (2012) Equality and Diversity. www.ic.nhs.uk/equality (accessed 18 October 2012).
- NHSNorth West Health Equality Library Portal (2009) Why Monitor? https://help.northwest.nhs.uk/somworkbook/ why_monitor.php (accessed 18 October 2012).
- UK Civil Service (2012) Best Practice Guidance on Monitoring Equality and Diversity in Employment. www.civil service.gov.uk/wp-content/uploads/2012/03/Equalities- Monitoring-Guidance-final.doc (accessed 18 October 2012).
- UK Government (2012) Employers: preventing discrimination. www.gov.uk/employer-preventing-discrimination (accessed 18 October 2012)
ADDITIONAL REFERENCES PUBLISHED IN THIS JOURNAL
- Cant B (2006) Out for the counting. Diversity in Health and Social Care 3:161–2.
- Hussein S and Manthorpe J (2011) ‘Third-ageâ€Âââ€Å¾Â¢ workers caring for adults and older people in England: findings from secondary analysis of the National Minimum Data Set for Social Care. Diversity in Health and Care 8:103–12.
- Iqbal G, Gumber A, Johnson MRD et al (2009) Improving ethnicity data collection for health statistics in the UK. Diversity in Health and Care 6:267–85.
- Johnson MRD and McGee P (2011) Canâ€Âââ€Å¾Â¢t count, wonâ€Âââ€Å¾Â¢t count. Diversity in Health and Care 8:63–6.
- Jones M and Kai J (2007) Capturing ethnicity data in primary care: challenges and feasibility in a diverse metropolitan population. Diversity in Health and Social Care 4:211–20.
- Meads C, Carmona C and Kelly MP (2012) Lesbian, gay and bisexual peopleâ€Âââ€Å¾Â¢s health in the UK: a theoretical critique and systematic review. Diversity and Equality in Health and Care 9:19–32.
- Salway S, Barley R, Allmark P et al (2011) Enhancing the quality of published research on ethnicity and health: is journal guidance feasible and useful? Diversity in Health and Care 8:155–65.
- Sundararajan V, Reidpath DD and Allotey P (2007) Ethnicity, discrimination and health outcomes: a secondary analysis of hospital data from Victoria, Australia. Diversity in Health and Social Care 4:21–32.