Rajshree Dayanand Katke*
Obstertrics and Gynaecology Department, Cama Albless Hospital, Mumbai, India
- *Corresponding Author:
- Rajshree Dayanand Katke
Associate Professor, Obstertrics and Gynaecology Department, Cama Albless Hospital, Mumbai, India
Tel: 91-022-22620390
E-mail: drrajshrikatke@gmail.com
Received date: June 15, 2016; Accepted date: July 29, 2016; Published date: August, 01, 2016
Citation: Katke RD. Large (7.2 kg) Subserosal Fibroid with Monkenberg’s Calcification in a Postmenopausal Woman: Extremely Rare Case with Review of Literature, Gynecol Obstet Case Rep. 2016, 2:2.
Keywords
Computed tomography; Ovarian mass;
Uterine subserosal leiomyoma; Ultrasonography; Subserosal
fibroid; Salpingoophrectomy; Hysterectomy
Introduction
Leiomyomas or fibroids arise from overgrowth of the
smooth muscle and connective tissue of the uterus, and most
commonly involve the uterine corpus, although they may also
occur in the cervix in a minority of instances. Typical fibroids
are easily recognized on imaging. However, an atypical
presentation caused by degenerative changes can cause
diagnostic confusion as in our case mimicking ovarian tumour
[1,2]. The use of color Doppler ultrasonography (CDUS) to
visualize interface vessels between the uterus and a juxtauterine mass is useful in the differential diagnosis. Also,
magnetic resonance imaging (MRI) yielding multiplanar views
can reveal the peduncle, or confirm the presence of a normal
uninvolved ovary [3]. In this case report, we present
multimodal abdominopelvic radiologic imaging findings of a
patient with a huge giant subserosal uterine leiomyoma, in
conjunction with histopathological findings.
Case Report
A 70 Year old postmenopausal woman presented to our
hospital with a complaints of gradual distension of abdomen
since 2 months and diffuse pain in abdomen since 3-4 months.
All routine laboratory test values were within normal limits. On
general examination patient was vitally stable. Per abdominal
examination revealed large abdominal mass corresponding to
28 to 30 weeks Gestational size of uterus arising from pelvis,
smooth surface, firm to hard in consistency, mobility slightly
restricted. Its lower border could not be felt. Per speculum
examination revealed cervical os was taken up. On per vaginal
examination a mass of 28-30 weeks gestational size was
palpable which was firm to hard in consistency, uterus could
not be felt separately from the mass, bilateral fornices were
free and there was no tenderness. Abdominal ultrasound
examination showed a large heterogenous hypoechoic mass of
size 20 cm × 15 cm × 18 cm in the pelvico abdominal region
displacing the uterus anteriorly and is not separately visualised
from either ovary query neoplastic origin likely ovary. Contrastenhanced
computed tomography of the abdomen and pelvis
demonstrated a large well defined lobulated soft tissue
attenuating minimally and heterogeneously enhancing solid
mass lesion of 21 cm × 16 cm × 19 cm with multiple foci of
calcification seen within the pelvis. Computed tomography
findings suggestive of benign etiology query subserosal fibroid.
Laboratory tests including tumour markers CA-125 and CEA
were within normal limits. Patient underwent exploratory
laparotomy with Total Abdominal Hysterectomy with bilateral
Salpingoophrectomy with removal of huge subserosal Fibroid.
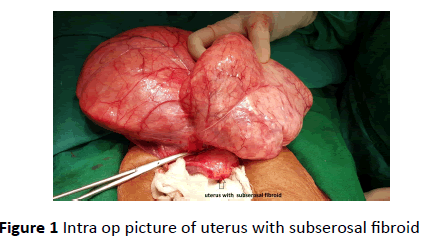
Laparotomy revealed a Huge mass of 28 cm × 18 cm × 20 cm
arising from anterior serosal part of uterus and the part of
peritoneum near the urinary bladder, the mass was highly
vascular and adherent to bladder and large bowel (Figure 1).
Figure 1: Intra op picture of uterus with subserosal fibroid
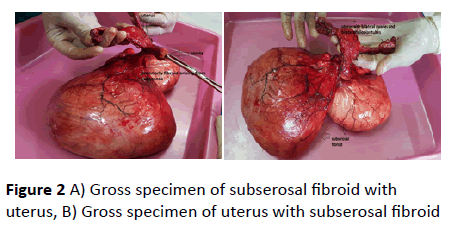
A succenturiate mass of 15 cm × 10 cm × 10 cm was seen
arising from the previous mass. Both mass were soft to firm in
consistency. Bilateral ovaries were atrophic and the uterus and
cervix was of normal size. Mass was firmly adherent to bowel
and urinary bladder and had to be separated by sharp
dissection. Abdominal hysterectomy with bilateral
salpingoopherectomy was performed. On gross inspection the
removed bilobed subserosal mass weighs 7.2 kg with atrophic
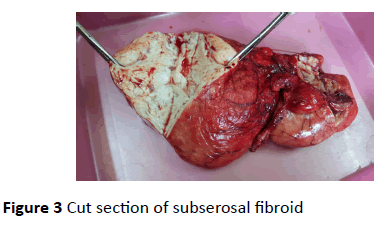
uterus was seen (Figure 2). On histopathological examination
revealed uterus was atrophic and myometrim showed thick
walled blood vessel with Monckeberg’s calcification with
subserosal leiomyomas. Sections through the mass revealved a
tumor arranged in interlacing fascicles and bundles with ient
areas of calcifications and degeneration. No significant atypia
was evident (Figure 3). Final impression suggestive of
subserosal fibroid. The Patient’s post-operative course was
uneventful.
Figure 2: A) Gross specimen of subserosal fibroid with
uterus, B) Gross specimen of uterus with subserosal fibroid
Figure 3: Cut section of subserosal fibroid
Discussion
Leiomyomas arise from overgrowth of the smooth muscle
and connective tissue of the uterus. Around the menopause,
leiomyomas decrease in size because their growth is thought
to be estrogen dependent, but leiomyomas may still be newly
diagnosed in postmenopausal women. A calcified
pedunculated leiomyoma in a postmenopausal woman is
extremely rare; in such cases it is more difficult to predict the
clinical symptoms and physical findings. In our case there was
discrepancy between ultrasonography and computed
tomography findings. Typical fibroids are easily recognized on
imaging, but atypical presentation caused by degenerative
changes can cause diagnostic confusion in postmenopausal
women [2]. As leiomyomas enlarge, they may outgrow their
blood supply, resulting in various types of degeneration:
hyaline, myxomatous, calcific, cystic or red degeneration. As in
our case it showed huge fibroid with calcific degeneration. In
general, hyaline degeneration is the most common (63%) form
of degeneration, while the others occur less frequently, such
as myxomatous changes (13%), calcification (8%), mucoid
changes (6%), cystic degeneration (4%), red degeneration
(3%), and fatty changes (3%) [3]. The finding of a calcified
leiomyoma is more common in postmenopausal woman. Over
time, the blood supply within the myoma might decrease, and
the tissue becomes ischemic. Calcium is deposited in the
peripheral portion of the leiomyoma. As the degenerative
changes progress, the leiomyoma may become calcified.
Pedunculated leiomyomas can have obscure origins and may
be mistaken for a lesion of ovarian origin. A sonographic
diagnosis of a pedunculated, subserosal leiomyoma can be
made if a vascular pedicle is demonstrated. On
Ultrasonography fibroids appear as well-defined, solid masses
with a whorled appearance. These are usually of similar
echogenicity to the myometrium, but sometimes may be
hypoechoic However, these features may not always be
detected sonographically [4-6]. Computed tomography is not
the primary modality for diagnosing leiomyomas. CT scan is
not the investigation of choice for the characterization of
pelvic masses. Uterine fibroids are often seen incidentally on
CT scans performed for other reasons. The typical finding is a
bulky, irregular uterus or a mass in continuity with the uterus.
Degenerate fibroids may appear complex and contain areas of
fluid attenuation [7,8]. MRI is the most accurate diagnostic test
to assess the precise sizes of the fibroids and the position of
each fibroid within the uterine wall (submucous, intramural,
subserous).
Conclusion
In the literature, calcified pedunculated subserous
leiomyoma in a postmenopausal woman is rare. Pedunculated
leiomyomas with calcified degeneration should be considered
in the differential diagnosis of a solid and calcified adnexal
mass. Our case is one of the rarest presentation of huge
subserosal fibroid with calcific degeneration which was
mimicking an ovarian mass in postmenopausal female.
Acknowledgement
Dr Nishtha Tripathi (Resident Doctor).
References
- Katke RD (2014) Torsion of huge cystic teratoma of ovary with multiple fibroids uterus: a case report and review of literature. Int J ReprodContracept Obstet Gynecol3(3):793-795.
- Ciarmela P, Ciavattini A, Giannubilo SR, Lamanna P, Fiorini R, et al. (2014) Management of leiomyomas in perimenopausal women. Maturitas 78: 168- 173.
- Hwang JH, Modi GV, Jeong Oh M, Lee NW, Hur JY, et al. (2010) An unusual presentation of a severely calcified parasitic leiomyoma in a postmenopausal woman. JSLS 14: 299-302.
- Samal SK, Rathod S, Rani R, Anandraj R (2014) An unusual presentation of a severely calcified subserous leiomyoma in a postmenopausal woman: a case report. Int J ReprodContracept Obstet Gynecol 3: 463-465.
- Singh K, Prasad D, Pankaj S, SumanS, Kumar A, et al. (2014) Postmenopausal massive subserous calcified fibroid: a case report. J of Evolution of Med and Dent Sci 3: 2255-2257.
- Caoili EM, Hertzberg BS, Kliewer MA, DeLong D, Bowie JD (2000) Refractory shadowing from pelvic masses on sonography: a useful diagnostic sign for uterine leiomyomas. AJR Am J Roentgenol 174: 97-101.
- Rajanna DK, Pandey V, Janardhan S, Datti SN (2013) Broad ligament fibroid mimicking as ovarian tumor on ultrasonography and computed tomography scan. J Clin Imaging Sci.
- Owen C, Armstrong AY (2015) Clinical management of leiomyoma. Obstet Gynecol Clin North Am 42: 67-85.