Original Article - (2017) Volume 18, Issue 3
Istanbul University, Istanbul Faculty of Medicine, Department of General Surgery, Istanbul, Turkey
Received February 09th, 2017-Accepted May 04th, 2017
Introduction The main objective of this study is to find out whether laparoscopic cholecystectomy alone is enough to prevent acute biliary pancreatitis attacks. Material and Method We performed a retrospective study with acute biliary pancreatitis patients who previously undergone cholecystectomy at the Istanbul Faculty of Medicine, Department of General Surgery, between January 2012 and December 2015. Acute biliary pancreatitis was diagnosed with elevated serum and urinary amylase levels with biliary pain. All the diagnoses were made with a combination of cholecystectomy history, physical examination, laboratory tests and imaging techniques [ultrasonography, magnetic resonance cholangiopancreaticography, computed tomography]. Ranson and Balthazar scores are assessed for each case. According to revised Atlanta grading system, the cases are classified as mild, moderate and severe pancreatitis. After a careful evaluation non-biliary pancreatitis patients are excluded from the study. Patients’ demographic datas, comorbidities, history of cholecystectomy and pancreatitis, laboratory tests, invasive procedures, rates of morbidity and mortality and period of hospital stay were analyzed. Results The mean age was 51.5 (21–73) years. Thirty-one patients were enrolled in the study, 23 of them (74.1%) were female and eight (25.9%) were male. The average Ranson score was calculated as According to revised Atlanta scoring system; 28 cases were assessed as mild, one case was moderate and two cases were in the severe category. Necrosis was seen in both severe cases, and there was no necrosis in the moderate category. Balthazar score for the mild cases were counted as 0, moderate cases were 1, and the severe cases as 7. There was no correlation between C-reactive protein level and necrosis with clinical severity. In 19 (61%) of the cases, biliary stone was spotted in the common bile duct on the radiology. Then, endoscopic retrograde pancreaticography was applied for these 19 patients. Two of the cases had infected-necrotizing pancreatitis. Disease lasted fatal in these two cases due to sepsis and multiple organ failure. Percutaneous drainage was applied under USG by the radiologist for one patient whom had an image of collection in the gall bladder bed. Three patients were excluded from the study as non-biliary pancreatitis. The average length of hospital stay was measured as 4-5 days. Conclusion Early cholecystectomy after first pancreatitis attack together with endoscopic retrograde pancreaticography procedure (for the cases that have indication) decreases rates of complication and recurrence greatly. Laparoscopic cholecystectomy alone does not always prevent acute biliary pancreatitis attacks, in patients with prior endoscopic retrograde pancreaticography traumas and patients with high cholestasis enzymes during pancreatitis. Prospective randomized large studies are needed to reach certain etiologic reasons.
Cholecystectomy; Pancreatitis; Recurrence
CT computed tomography; ERCP endoscopic retrograde cholangiopancreatography; MRCP magnetic resonance cholangiopancreaticography
The etiology and common pathogenesis of acute pancreatitis were investigated for centuries. The potential pathogenetic theories are controversial; mostly due to biliary or non-biliary factors, and also can be idiopathic which occur due to unknown reasons. Biliary pathologies are 80-90% reason of acute pancreatitis. Among these; the most common cause is the gallstone impacting the confluence at the distal common bile duct and pancreatic duct [1, 2]. In the studies done about biliary pancreatitis; it has been noticed that biliary stones are seen with a percentage of 88% in radiologic and fecaloid tests of the patients. Modern life style and dietary habits increase the incidence of cholelithiasis [3]. Patient history, physical examination, laboratory tests and radiologic studies are used to make the diagnosis of acute biliary pancreatitis. Conservative approach, surgery, endoscopy and interventional radiology are the main choices used in the treatment. Acute biliary pancreatitis has a clinical course varying from a mild attack, which usually subsets in a few days to a severe clinic with local (pseudocyst, phlegmon, abscess, necrosis) and systemic (Multiple organ failure, disseminated intravascular coagulation, acute respiratory distress syndrome, etc.) complications, and even sometimes leading to death, which require long periods of hospital stay [4].
Laparoscopic cholecystectomy is the gold standard approach to prevent acute biliary pancreatitis attacks. The authors usually suggest surgery when the clinic of acute biliary pancreatitis subsets and liver enzymes start to decrease [5].
In this study; we evaluated the patients with the clinic of acute biliary pancreatitis whom have a history of cholecystectomy because of cholelithiasis. Patients having history of cholecystectomy should be examined more carefully compared to the ones without cholecystectomy.
We performed a retrospective analysis of acute biliary pancreatitis (ABP) patients at the Istanbul Faculty of Medicine, Department of General Surgery from January 2012 to December 2015. During this period, 246 patients with acute biliary pancreatitis were identified. Thirtyone patients who had previously had cholecystectomy from these patients were included in the study. All clinical records were retrospectively reviewed. Acute biliary pancreatitis was diagnosed with elevated serum and urinary amylase level and biliary pain.
Oral intake was stopped after diagnosis. Analgesic therapy had been ordered. Informed consent was obtained from all participants, and study followed the guidelines of the Declaration of Helsinki. Study protocol was approved by institutional ethics committee.
The patients having calculus in the biliary tract without cholecystectomy history (cholecystocholedocholithiazis) and the ones with known biliary calculus who have a record of pancreatitis attack after cholecystectomy had been included in the study. In the most updated studies; the appropriate time to make cholecystectomy after acute cholecystitis attack has been stated as in the following three days or after six weeks. In our study, we discussed the clinical course of the patients who undergone cholesystectomy at different time intervals (Figure 1).
Malignancy, history of trauma, enfection and alcohol induced pancreatitis, hyperlipoproteinemia, congenital pancreas anomally (pancreatic divisum etc.) and hyperlipidemia are excluded from the study.
All patients were viewed by USG at the admission. Hepatobiliary USG was a helpful tool on determining to prefer MRCP (Magnetic Resonance Cholangiopancreatiography). Patients having high levels of cholestatic enzymes (ALP, GGT, and Billirubins) above the normal range were screened with MRCP to rule out any calculus, or other obstructive lesion in the biliary tract.
Oral contrast enhanced abdominal angiographic computerized tomography (CT) was preferred for the patients having Ranson value above three, or with increasing values of white blood cells (WBC) and C-reactive protein (CRP) (Figure 2).
Ranson and Balthazar scores are determined at the time of admission. Patients are classified according to revised Atlanta classification system as mild, moderate or severe.
Patients aged who were diagnosed with necrotizing pancreatitis, primary sclerosing cholangitis, pseudocysts, non-biliary pancreatitis, intrahepatic lithiasis, primary biliary cirrhosis, gall bladder and biliary duct tumors, or drug-induced pancreatitis; and those who did not accept undergoing an operation were excluded from the study.
Patients were evaluated according to differences in age, gender, cholecystectomy history, blood tests results, morbidity-mortality rates, invasive procedures done and the average length of hospital stays.
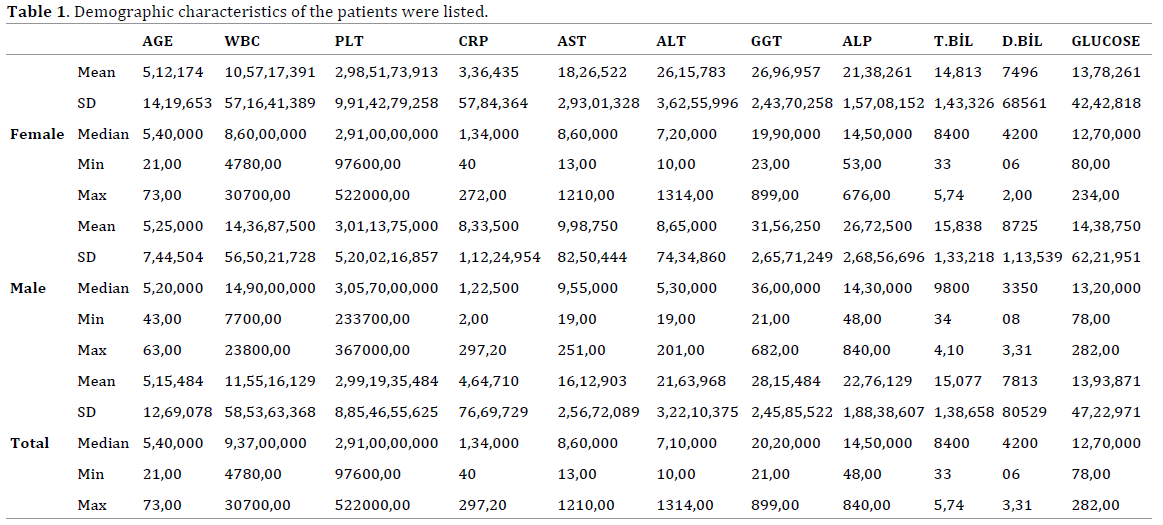
Thirty-one patients were enrolled in the study. Median age was 51.5 (21-73). There were eight men (median age: 52.5 (43-63)) and 24 women (median age: 51.2 (21-73)) (Table 1).
There was no pathologic finding in abdominal USG of 20 patients. In 11 patients; indirect findings of biliary pancreatitis were detected as choledocholithiasis, dilated choledochus, dilated wirsung and dilatation of intra-extra hepatic biliary tree. Twenty-three patients were screened with MRCP. Biliary calculus and dilatation had been detected ın 17 of these patients. Biliary tract was normal in six of these patients.
Two patients having a Ranson score above three and increasing values of WBC and CRP had been viewed with oral contrast enhanced angiographic abdominal CT at the time of admission. One patient had been screened with CT due to high WBC and CRP levels, and edematous pancreatitis was detected. CT was performed to the other patient due to the contraindication of MRI screening, and choledocholitiazis and bile duct dilatation was observed.
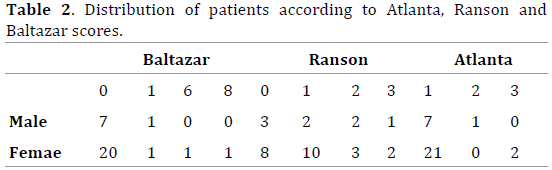
Average Ranson score calculated was 1. For revised Atlanta scoring system, 28 of the patients were evaluated as mild, one as moderate, and two of them were severe. In two of the severe cases, necrosis was seen on the CT scan, and edematous pancreatitis was found in one of the moderate case. Average Balthazar score found for the mild cases were 0, moderate ones; 0, and for the severe cases as seven (Table 2).
Ten of the patients had once a history of ERCP, three others had twice ERCP record. ERCP was performed to 19 patients (61%) whom were considered as mechanical obstruction radiologically and clinically. Stone extraction from common bile duct was performed in 12 patients during the ERCP procedure. No stone was detected in seven patients. Decision to perform ERCP was made according to clinical course (cholestatic enzyme levels) and radiologic screenings of the patients (Abdominal USG and MRCP).
ERCP was performed for three of the patients because of elevated cholestatic enzymes and bilirubin levels although radiologically the biliary tract was normal. Severely infected necrotizing pancreatitis had occurred in two of the patients and it was fatal due to sepsis and multiple organ failure in these patients. Percutaneous drainage procedure was performed to one patient after a collection was detected in the gall bladder bed. Average length of hospital stay was 4-5 days (1-13 days). There was no correlation among CRP levels, necrosis and clinical severity. There has been confirmed a time interval ranging from a few days to years between the time of cholecystectomy and first recurrence of biliary pancreatitis.
Accurate patient history and essential physical examination have paramount importance in reaching the diagnosis of pancreatitis. The patient must be questioned about a possible biliary colic history. The patients mostly complain with severe epigastric pain radiating to the back. This is usually accompanied by abdominal distension (could be secondary to intraperitoneal collection) with nausea and vomiting [6].
Bile stone occurrence depends various etiologies as the amount of bile salts within bile and cholesterol ratio, the balance between the factors that stimulate micelle formation and the ones that prevent it, and infectious pathologies [7]. Bile duct stones are still the leading reason of acute recurrent pancreatitis in cholecystectomized patients. During cholecystectomy; sometimes stones missed in biliary tract and they cause to cystic duct stump or intrahepatic litiazis. Especially the stones, which occur after ERCP and sfincterotomy, have a high prevalence. In our study; we evaluated the rates of recurrent biliary pancreatitis seen in patients who had history of cholecystectomy before. It is discussed if cholecystectomy is a factor in reducing the prevalence of recurrent pancreatitis.
Liver function tests and bilirubin levels seen in normal range for patients having acute biliary pancreatitis. Considering that, these patients must be evaluated more carefully. To prevent the calculi remain in the biliary tract, preoperative cholangiography is preferred during cholecystectomy. By this, the calculi in the biliary tract can be spotted and it becomes possible to make intervention during the operation. Stone extraction can be made by the exploration of the cystic duct and common bile duct, and the function of sphincter of Oddi can be preserved [8, 9]. To apply this procedure, there should be enough equipment and the surgery team should have the necessary experience needed. In our study; 13 patients (42%) were diagnosed as mechanical icterus, findings of cholangitis were observed in two patients (6%). On the other hand, in some these patients neither radiologically nor with ERCP, calculi had been seen. Cholestatic values had been found above normal limits with biochemical tests.
The usage of intraoperative cholangiography in every patient is not a cost effective approach. Besides that, intraoperative cholangiography is not predictive in detecting small stones and the secondary calculi, which can occur after the operation. Also, it might be unnecessary to perform intervention for ones that pass sphincter of Oddi. Intraoperative cholangiography can be used in selected cases, which have a doubt about calculi in the preoperative radiological view of the biliary tract.
Cholecystectomy is suggested to decrease the risk of acute biliary pancreatitis in patients who have known calculi in the gall bladder and clinically symptomatic. In studies done with large patient populations, it has been seen that early time cholecystectomies (In three days after the clinic had begun, or six weeks later) after the local or systemic complications of biliary pancreatitis residue, the recurrences were seen much less. By this, complication rate (Biliary colic, choledocholitiazis, cholangitis and recurrent pancreatitis) which occur due to calculi in the biliary tract decreases [10].
Sphincterotomy with stone extraction procedure done with ERCP is the gold standard approach for the calculis in the common biliary duct. It is not preferred for acute biliary pancreatitis cases with mild clinic, but can be helpful for the ones which have associated cholangitis clinic and not suitable for cholecystectomy [11].
When these two different approaches compared; ERCP is not superior to cholecystectomy on the long term to decrease the rates of biliary recurrences, addition to that it must not be preferred unless necessary [12]. Some of the patients who underwent cholecystectomy with acute biliary pancreatitis undergo pancreatitis after cholecystectomy and it is important that patients in such a risk group can be determined in advance. In our study, although the number of patients was low it is shown that patients with previous history of ERCP, or those with high cholestasis exacerbations in first pancreatitis attack were in the risky group. Cholecystectomy alone is not enough to prevent pancreatitis in patients in such a risky group.
In our study, it has been stated that only cholecystectomy, does not prevent the risk of pancreatitis occurrence completely. Because of that, it must evaluated in all different aspects such as; clinical course (age, any other known diseases, previous attacks), ultrasonography of the biliary tract and MRCP if necessary, and must act accordingly. Considering the variable periods of time between each attack, prospective randomized studies having longer observation times with higher patient populations are needed.
The authors have declared that no competing interests exist.