- (2012) Volume 13, Issue 4
Gavin Low
Department of Radiology and Diagnostic Imaging, University of Alberta Hospital. Edmonton, Canada
Received April 30th, 2012 Accepted May 2nd, 2012
Choristoma; Diagnostic Imaging; Magnetic Resonance Imaging; Multidetector Computed Tomography; Radionuclide Imaging; Spleen
99mT-HDRBC: 99mTechnetium-heat damaged red blood cell
Dear Sir,
I read with interest the article entitled ‘Intrapancreatic accessory spleen: investigative dilemmas and role of EUS-guided FNA for diagnostic confirmation’ by Krishna et al. in the November 2011 issue of JOP. Journal of the Pancreas [1]. This well written case report and succinct review of the literature outlines the clinical and radiological dilemmas associated with this condition.
Intrapancreatic accessory spleen (IPAS) refers to a focal mass of ectopic splenic tissue located within the tail of the pancreas. It originates embryologically from failure of fusion of the splenic anlarge in the dorsal mesogastrium. While found in 10-30% of post-mortem cases, Mortele et al. reported a prevalence of intrapancreatic accessory spleen of 2 in 1,000 consecutive patients that underwent abdominal CT imaging on older generation computed tomography (CT) scanners [2]. This radiological under-call is due to the small lesion size (a significant proportion of intrapancreatic accessory spleen measure 2 cm or smaller in size) making detection more difficult [3, 4]. However, the last decade has borne witness to a technological imaging revolution with rapid improvements in the diagnostic capabilities of crosssectional imaging modalities such as CT and magnetic resonance imaging (MRI). As these powerful tools are able to detect and resolve lesions with increasing clarity and precision, this has led to a corresponding increase in the detection of incidentalomas on imaging. Many of these incidentalomas are small, asymptomatic and clinically occult. This leaves clinicians with the dilemma of what to make of these incidentalomas, their clinical significance, and how they should be appropriately managed. Within this context, it is reasonable to anticipate that the prevalence of intrapancreatic accessory spleen will increase due to improvements in imaging technology. As a benign asymptomatic condition, intrapancreatic accessory spleen does not require treatment and may be regarded as a ‘do not touch lesion’. The clinical and imaging dilemma lies in that intrapancreatic accessory spleen is frequently misdiagnosed for a pancreatic malignancy. In some cases, this may be due to poor awareness and understanding of the condition. In others, a working diagnosis of intrapancreatic accessory spleen is not entertained for the fear of missing a malignancy. This is regrettable as misdiagnosing intrapancreatic accessory spleen for a pancreatic malignancy leads to unnecessary patient anxiety and inappropriate patient management. This includes performing a distal pancreatectomy which subjects patients to unwarranted postoperative morbidity and risk of postoperative complications.
The differential diagnoses for a small solitary soft tissue mass in the pancreatic tail include intrapancreatic accessory spleen, pancreatic adenocarcinoma, neuroendocrine tumor and pancreatic metastases. These lesions can often be characterized and differentiated on imaging (Table 1). High resolution multiphasic contrast enhanced-CT and/or MRI, widely available in most centers worldwide, can render precise lesion characterization and differentiation. When compared to the spleen, intrapancreatic accessory spleen exhibits a similar attenuation and signal intensity on CT and MRI, respectively, and similar post-contrast enhancement (throughout all vascular phases) [4]. In particular, the arciform pattern of arterial enhancement within the intrapancreatic accessory spleen, similar to that seen in the adjacent spleen, is highly suggestive of the diagnosis (Figure 1) [4]. The arciform pattern of arterial enhancement is secondary to perfusion differences between red pulp and white pulp present within tissues of splenic origin. This arciform enhancement helps to differentiate intrapancreatic accessory spleen from other focal arterially enhancing pathologies in the pancreatic tail such as neuroendocrine tumor (heterogeneous or ring-like arterial enhancement) and pancreatic metastases (heterogeneous arterial enhancement) from hypervascular neoplasms such as renal cell carcinoma. Solid pseudopapillary tumor may show mild heterogeneous arterial enhancement but it is not typically confused with intrapancreatic accessory spleen as it is generally large at presentation (mean size of 9 cm) [4]. Pancreatic adenocarcinoma is a hypovascular neoplasm. In indeterminate cases, specialist tests such as a 99mTechnetium-heat damaged red blood cell (99mT-HDRBC) study, a 99mT-sufur colloid study or a superparamagnetic iron oxide (SPIO) enhanced MRI study may confirm the diagnosis [4, 5]. Intrapancreatic accessory spleen may show high radiotracer uptake on 99mT-HDRBC and 99mT-sufur colloid and sensitivity may be improved if these tests are performed as part of a single photon emission computed tomography (SPECT) examination. On superparamagnetic iron oxide enhanced MRI, intrapancreatic accessory spleen exhibits signal loss similar to the spleen on T2/T2*-weighted MR images due to phagocytosis by reticuloendothelial cells in these tissues [4, 5]. Limitations include small intrapancreatic accessory spleen foci that do not contain sufficient reticuloendothelial tissue to render confident imaging characterization and the specialist nature of these tests (e.g., superparamagnetic iron oxide MRI contrast agents are not routinely performed clinically) which precludes widespread accessibility and uptake. Contrast enhanced ultrasound has also been advocated as a diagnostic test for evaluating intrapancreatic accessory spleen [6]. However, this technique is limited by difficulties in obtaining adequate sonographic visualization of this small deep seated lesion; and image obscuration from overlying bowel gas shadowing. Furthermore, not all centers perform contrast enhanced ultrasound. When noninvasive diagnostic tests fail, fine needle aspiration biopsy employing image guidance (e.g., CT, ultrasound, endoscopic ultrasound) can be performed for cytological diagnosis [1]. However, this is not a full proof procedure and may yield unsatisfactory results due inadequate biopsy specimens and sampling error. The small size of intrapancreatic accessory spleen and deep location make it a challenging target to both access and biopsy. Furthermore, there is a small risk of biopsy related complications such as hematoma, pancreatitis and trauma to adjacent tissues. It is highly preferable if diagnosis can be made non-invasively, whenever possible.
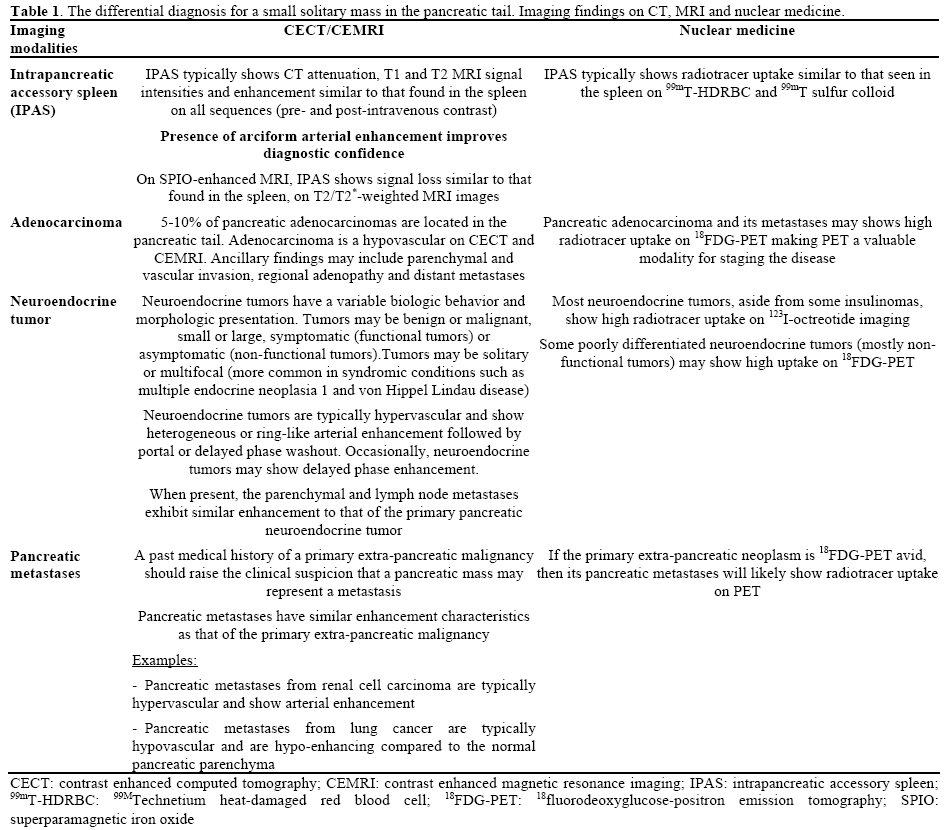
Figure 1. A 59-year-old male with a previous history of a resected duodenal carcinoid tumor. a. .An axial arterial-phase contrast enhanced CT image. b. An axial arterial-phase contrast enhanced MRI image. Arciform arterial enhancement, similar to that found in the spleen, is present in the intrapancreatic accessory spleen (IPAS) (curved arrows) on both the CT and MRI images. The IPAS showed high radiotracer uptake on a corresponding 99mTechnetium heat damaged red blood cell study and remained stable on a follow up MRI examination performed at 12 months.
In conclusion, I would like to reiterate that intrapancreatic accessory spleen, in most cases, can be confidently diagnosed non-invasively on high quality thin-slice multiphasic contrast enhanced CT or MRI. Intrapancreatic accessory spleen shows a similar attenuation, signal intensity and enhancement pattern with the spleen on all sequences. In particular, one should pay attention to the characteristic arciform pattern of arterial enhancement, a feature shared by intrapancreatic accessory spleen and the spleen. This pattern of enhancement permits differentiation of intrapancreatic accessory spleen from neuroendocrine tumors and other arterial enhancing neoplasms in the pancreatic tail, which show heterogeneous or ring like enhancement patterns. In patients with imaging findings characteristic for intrapancreatic accessory spleen, follow-up imaging at 6 and 12 months, for a 1- year duration, is helpful in confirming interval lesion stability consistent with this benign diagnosis.
The study did not involve any grants and there are no disclosures or conflicts of interest