Review Article - (2020) Volume 21, Issue 4
1Department of General Surgery, Ospedali Riuniti Marche Nord, Pesaro, Italy
2Department of General Surgery, Carlo Urbani Hospital, Jesi (Ancona), Italy
Received Date: April 06th, 2020; Accepted Date: July 16th, 2020
Pancreatic cancer ranks among many of the death causes linked to cancer. The average diagnostic scale of pancreatic cancer is around 31 mm & hasn't substantially changed in the past thirty years. The late-presenting indications were associated with poor early tumour diagnosis. Commonly used imaging techniques used in the pancreatic cancer diagnosis is Magnetic Resonance Imaging, Endoscopic Ultrasound, and Computer Topography. In the Pancreatic Ductal Adenocarcinoma treatment, vascular resection remains a topic of debate. Vascular resection should only be conducted on carefully selected subjects that have an proof for the occurrence of resectable tumours or borderline resectability tumours from the pre-operative imaging investigations. Resection at an early stage of pancreatic cancers is the best chance of cure. Venous resection and reconstruction have become a standard technique to achieve negative margins, and in complex venous resections/reconstructions, it is highly advisable to seek the help of experienced vascular surgeons.
Pancreatic cancer ranks among many of the death causes linked to cancer. The average diagnostic scale of pancreatic cancer is around 31 mm & hasn't substantially changed in the past thirty years. The late-presenting indications were associated with poor early tumour diagnosis. Commonly used imaging techniques used in the pancreatic cancer diagnosis is Magnetic Resonance Imaging, Endoscopic Ultrasound, and Computer Topography. In the Pancreatic Ductal Adenocarcinoma treatment, vascular resection remains a topic of debate. Vascular resection should only be conducted on carefully selected subjects that have an proof for the occurrence of resectable tumours or borderline resectability tumours from the pre-operative imaging investigations. Resection at an early stage of pancreatic cancers is the best chance of cure. Venous resection and reconstruction have become a standard technique to achieve negative margins, and in complex venous resections/reconstructions, it is highly advisable to seek the help of experienced vascular surgeons.
Pancreatic cancer; Portal Vein; Pancreaticoduodenectomy
EU Endoscopic Ultrasound; CT Computer Topography; MRI Magnetic Resonance Imaging; PDAC Pancreatic Ductal Adenocarcinoma; PV Portal Vein; SMV Superior Mesenteric Vein; SMA Superior Mesenteric Artery; NCCN National Comprehensive Cancer Network; MDT Multidisciplinary Team; EUS Endoscopic Ultrasonography; ISGPS International Study Group for Pancreatic Surgery ; PD Pancreaticoduodenectomy
Pancreatic cancer is ranked as the fourteenth commonest cancer in the world as well as the 7th highest cause for cancer related mortality. Epidemiology estimations reported 4.58.918 diagnoses & deaths of 4.32.242 patients from pancreatic cancer worldwide in 2018 [1]. In Europe, there were more than 78,000 new case subjects in 2012 [2]. Each year in the US, approximately 43,000 people die of pancreatic cancer making it the 4th commonest cancer linked death cause [3]. Despite investigation and improvements in the treatment of this ailment, it’s prone to become the 2nd chief cancer-linked death cause within the next decade [4]. Approximately 55,440 (26,240 women & 29,200 men) were estimated to be confirmed with pancreatic cancer in the year 2018, and approximately 44,330 (21,310 women & 23,020 men) might have died from pancreatic cancer [5]. 1-5% of average long-term rates of survival are linked to pancreatic cancer PDAC (pancreatic ductal adenocarcinoma), demonstrating poor predicted survival [6]. A number of factors led to an increased pancreatic cancer risk. Such factors of risk range from; usage of tobacco, obesity, overweight, occupational exposure to certain chemicals (benzene, dyes, petrochemicals & pesticides), family history, ethnicity, gender, age, hereditary inherited syndromes, chronic pancreatitis, diabetes, stomach problems, liver cirrhosis, diets, physical inactivity, alcohol and coffee [7]. Pancreatic cancer signs & indications differ depending on the location & tumour stage. The tumours at the pancreas head cause obstructive jaundice & loss of weight resulting in diarrhoea & steatorrhea. Tumours of the tail & body usually lead to pain in the abdomen & loss of weight. Pain is also commonly linked to pancreatic cancer. The pain typically acts as a dull, deep pain, originating from the upper abdomen, radiating to the back [8].
PDAC is one of the few poorly predicted cancers, with less than five percent of subjects surviving five years after diagnosis. Surgical resection in these cases is the only hope of curative treatment. Though, only 10 to 20 percent of subjects are fit for resection as nearly fifty percent present with metastatic & thirty five percent with locally advanced surgically un-resectable disease. PDAC's poor prognosis is primarily related to late diagnosis [9, 10] These Days, radical surgical intervention for pancreatic cancer patients is the only possibly therapeutic option. Radical surgical resection accompanied by adjuvant chemotherapy can be carried out in around twenty percent of all PDAC subjects during the diagnosis period & is quite often the only hope for subjects' long-term survival, with an estimated five-year survival of 20 to 25% [9, 11]. During diagnosis, higher then eighty percent of them are un-resectable owing to invasion of retroperitoneal tissue, PV (Portal Vein)/SMV (Superior Mesenteric Vein), hepatic or peritoneal metastases development, invasion of the mesenteric artery, or failure to withstand significant surgical resection. Extended procedures, comprising vascular resections, have become more common in specialist centers as a consequence of advanced technologies & surgical procedures [12]. This has resulted in a substantial improvement in pancreatic surgery & has broadened the resectability boundary & increased the chance of obtaining a curative surgical strategy in pancreatic cancer patients associated with neoadjuvant & adjuvant treatment approaches. Highlevel of biological activity & early retroperitoneal tissue involvement, lymph nodes, & peri-pancreatic blood vessels are the characteristics of pancreatic carcinoma. Most of the pancreatic cancers are detected at an advanced phase. About thirty to thirty five percent are graded as unresectable due to the isolated participation of the portal vein/superior mesenteric [13]. For the first time, Fortner systematically presented the resection idea of the PV for complete tumour removal [14]. At high volume pancreatic centers, resection of portomesenteric vein is currently considered as a standard protocol. For a modern pancreatic surgeon, vascular operating experience is essential. Only resections of artery are still a contentious topic nowadays. Nonetheless, instances of resection comprising reconstruction of major arteries like hepatic artery, SMA (Superior Mesenteric Artery) & the coeliac axis have been recorded, even though in small series of case [15]. With this context here, the techniques, indications & major consequences of vascular resection & reconstruction for extensive pancreatic cancer surgery were reviewed by us.
Classification of PDAC
The pancreatic tumours were traditionally been considered either un-resectable or resectable. NCCN (National Comprehensive Cancer Network) was the first to propose definition for borderline resectable PDAC, that applies to tumours affecting surrounding structures as not to be explicitly un-resectable nor explicitly resectable [16]. Aggressive treatment of this community of neoadjuvant chemotherapy patients has enabled surgery to be practicable & advanced PDAC surgical methods, including vascular & multivisceral resections, have been performed widely [16, 17]. However, vascular resection remains a topic of discussion in the PDAC management, and hence this assessment elasticities and overview of the management & abreast knowledge on vascular resection like indications, techniques, major outcomes in PDAC surgery.
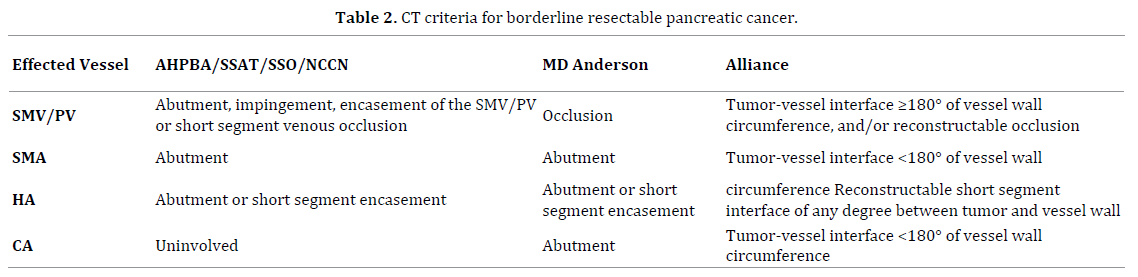
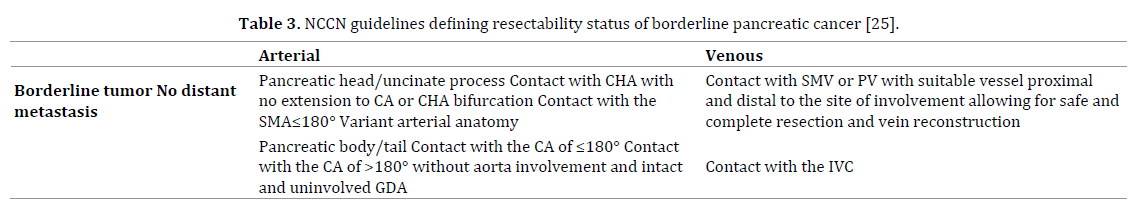
For localized PDAC, three resectability grades are described; these are “resectable”, “borderline resectable”, & “unresectable”, summarized in (Table 1) [18]. If the celiac trunk & SMA, the SMV & PV are patent, & if there are no distant metastases then pancreatic ductal adenocarcinoma is well-defined as resectable. However, more subjects have been encompassed in a growing borderline resectable disease category with the advancement of more comprehensive tools of imaging & surgical procedures [18, 19]. Patient’s with focal tumour abutment of superior mesenteric artery (<180°), gastroduodenal artery encasement up to the hepatic artery, or SMV/PV involvement that can be resected & reconstructed. Patients with tumour encasement (more than half of the vessel circumference) or an occlusion/thrombus of superior mesenteric artery, an un-re-constructable superior mesenteric vein or SMV-PV confluence occlusion, or a direct involvement of the aorta, inferior vena cava, or celiac axis are not fit for surgery [18]. In combination with vascular resection, the basis of pancreatectomy is to upsurge the likelihood to attain a curative R0 resection. Neoadjuvant method is not advised in venous borderline resectability, but upfront surgery must be carried out instead, & if the intraoperative outcome matches the situation of presumed borderline as described above completed as an en bloc tumour removal with venous replacement [18, 19]. Subjects classified as borderline resectable based on features of arterial involvement observed at imaging ought to go through surgical examination to attain further confirmation of any arterial infiltration, and if there is confirmation of an arterial borderline resectability intra-operatively as a true arterial involvement, palliative treatment ought to be considered as the standard of care [18, 19].

Indications for Vascular Resection
Extended surgical methods, such as multivisceral & vascular resections, are been performed commonly in Pancreatic ductal adenocarcinoma owing to improved surgical procedure & intensive care, including exact management of complications [17]. Combined PV resection with pancreatectomy ought to be addressed with a view to attain clear margins of resection based on pre-operative imaging in suspectable cases of portal vein invasion instead of deciding purely on the basis of operational findings. All subjects ought to go through CT (contrast-enhanced tomography) as regular pre-operative work up. The development of computed axial tomography with multislice multi-detector allows imaging of entire pancreas in the peak contrast intensification. Also, it is also possible to process the information from the contrast-enhanced tomography to obtain 3D images & visualizing different view planes. Spiral computed axial tomography with IV contrast & thin-section technique may precisely evaluate the relationships of low-density tumor formation to the celiac trunk, SMA & superior mesentericportal vein confluence. Based on the discussion of MDT (Multidisciplinary Team), MRI, EUS & laparoscopy must be carried out on an individual subject basis. MRI is generally prescribed when liver metastasis is suspected to be present. As per Ishikawa et al [20] & Nakao et al [21], the indications are confined to unilateral (≤ 180°) segmental vascular involvement. Particular attention was given to the omission of the deep retroperitoneal invasion cases, characterized by the intact connective tissue’s absence between the right lateral side of SMA & the tumor. As an absolute contraindication, the involvement of isolated artery isn’t accepted. At this stage, EUS (Endoscopic Ultrasonography) is more effective in detecting invasion in the porto-mesenteric system & in the specialized medical centers it is a standard procedure. Tumors with simultaneous numerous blood vessels involvement at the same time or with a massive retroperitoneal invasion are treated as resectable only in the case of neoadjuvant chemotherapy sensitivity.
As per these suggestions, pre-operative resectability assessment ought to be done on the basis of CT scan with a protocol that is pancreas-specific, such as a “hydropancreas” CT. For localized Pancreatic ductal adenocarcinoma, 3 resectability grades are defined, these are “resectable,” “borderline resectable,” & “unresectable” [18].
When there is no presence of vascular attachment i.e. no distortion of the venous structures & clearly preserved fat planes toward the arteries, then a tumour is classified as resectable. When occlusion/narrowing/distortion of the mesentericoportal veins is diagnosed with a technical reconstruction possibility on the veins’ distal & proximal margin or an attachment at the hepatic artery without the celiac axis or a semi circumferential abutment (≤ 180°) of the SMA then the resectability is classified as borderline. Tumours with celiac trunk and/or superior mesenteric artery infiltration or as tumours that involves the SMV, PV, or their confluence then these locally advanced tumour is classified as surgically unresectable tumours. The “encasement” term means that the tumour cannot be distinguished from the blood vessel for more than 180° of the latter’s circumferences. A tumour is well-defined as unresectable when it has distant presence of metastases, having superior mesenteric artery encasement >180°, any celiac abutment, unreconstructible superior mesenteric vein/PV, invasion or encasement of aortic/IVC, or lymph nodes metastases beyond the resection field.
Given the advancement of pancreatic imaging, it might be difficult to distinguish between the resectable disease (stage I & II) & locally advanced disease (stage III) & such cases are classified as “borderline resectability”. Vascular resections are typically needed in cases often defined as having “borderline resectable” findings. Borderline resectable carcinoma is defined as per 2009, exert consensus statement [22] & encompasses involvement of short superior mesenteric vein/portal vein with free proximal & distal venous segments, allowing secure reconstruction & superior mesenteric artery less than 180° or involvement of short hepatic artery with intact truncus coeliacus. The discrepancy from the classification of M.D. Anderson Group is taken into consideration the tumours, abutting or encasing (relying on the tumourvessel interface degree) the superior mesenteric vein/ portal vein borderline but is not resectable [23].
The Cao et al TVI-classification takes into account the circumferential interface of radiographic tumour vein & its importance as a prognostic tool for concomitant resection of vessel [24].
A consensus statement standardizing the definition of the “borderline resectability” term in compliance with the NCCN (National Comprehensive Cancer Network) guidelines and also the concept of extended resections issued by the ISGPS (International Study Group for Pancreatic Surgery) (Table 2) [18, 22, 23].
The methodology ought to be distinct when diagnosing the borderline findings in the involvement of arterial & venous vessel. In venous borderline resectability, the neoadjuvant therapy is not advised. Upfront surgery ought to be carried out &, if the intra-operative finding matches the situation of presumed borderline as per above demarcation, completed as an en bloc tumour removal with venous replacement [18]. In comparison, palliative treatment must be considered the standard of care when the arterial borderline resectability which was suspected is confirmed intra-operatively as a true arterial involvement. The neoadjuvant therapy may be used to stratify & identify the subjects with borderline findings that don’t profit from extended resections. Subjects under neoadjuvant therapy with a clear progression of tumour must be omitted from secondary exploration. Vascular resection should be carried out in subjects who are cautiously chosen with data for the resectable tumours’ presence or with borderline resectability tumours from pre-operative computed axial tomography.
For Vascular Resection and Reconstruction
The NCCN (National Comprehensive Cancer Network) guidelines definition is based on the tumor relation with the involved major vessels (Table 3) [25].
Depending on the extent of the invasion of the PV & SMV, different techniques for resection & reconstruction are used. In minimal invasion cases, a partial resection & reconstruction with an autologous patch may be performed. A peritoneal patch has been described as feasible [26]. In cases of broader invasion, segmental resection and reconstruction should be performed. When an end-to-end anastomosis isn’t possible, autologous, homologues, or prosthetic (ring) grafts are the options [27]. The classification proposed by the International Study Group of Pancreatic Surgery divided the venous resection in 4 types depending on the performed reconstruction: venorrhaphy, patch, primary anastomosis, & interposition conduit [28]. However, with large-scale mobilization of the root of the mesentery, an end to end anastomosis is almost always likely. Technically, an extensive Kocher Maneuver together with a Cattell-Braasch maneuver is a safe technic to perform pancreatic and venous resection. 45 subjects, who went through pancreatectomy with portomesenteric resection in a retrospective study, none had a thrombosis after a median follow-up of 22 months [29].
In a retrospective examination of a prospectively gathered database of two hundred forty one subjects who went through pancreatectomy with venous resection, no differences in mortality, morbidity & long-term survival were noticed related to patients who underwent a standard resection [30, 31]. In a large multicenter retrospective review from the United Kingdom that included 1588 subjects with borderline resectable tumors, venous resection in pancreatic cancer surgery was also reported as safe & feasible [32]. Median survival (eighteen months for the standard procedure &18.2 months for patients undergoing venous resection, P=0.0001) and in hospital mortality were similar in both groups [33]. Thus, if a resection with a tumor negative-margin seems possible, venous resection should be performed if necessary. Such an approach is now internationally well accepted.
Venous Resections
Involvement of major vessel in PDAC subjects has been a contraindication to resection, historically. Fortner, in 1973 outlined a surgical method of regional pancreatectomy which involves en bloc peripancreatic soft tissue resection, regional lymph nodes with portal vein (type I) resection, or major artery resection & reconstruction (type II). While these extended resections attained improved rates of resectability, high mortality (twenty three percent) & high morbidity (sixty seven percent) linked to low rates of survival (three-years survival rate three percent) inhibited generalized adoption of resection & reconstruction of major vessel [14]. Nevertheless, major improvements in surgical & radiological procedures could be accomplished, which would result in enhanced preoperative staging, better selection of subjects as well as reduction of surgical mortality & morbidity [34]. Contrary to involvement of artery, the superior mesenteric vein or portal vein invasion isn’t in itself an unresectability criterion. [35, 36]. Unlike arterial resection, widespread acceptability of Pancreaticoduodenectomy (PD) with PV approaches has been achieved in many centers around the world & can be safely performed with no peri-operative mortality or morbidity increase in comparison to standard PD [35, 36, 37, 38]. When there is involvement of Portal vein or superior mesenteric vein, attempting a resection is legitimate & venous excision is either performed by a tangential resection or by a segmental resection [39, 40].
Venous Resection and Reconstruction - Technical Outcomes
Depending in the type of reconstruction that is performed, different venous patency and patient outcomes have been reported. Direct vein reconstruction without patch or interposition graft has a lower rate of thrombosis [41]. The length of the reconstruction has also an important role in patient outcomes. In a Japanese retrospective analysis of 810 subjects, 9% subjects suffered severe anastomotic stenosis within the first post-operative year. A significant part of these subjects was symptomatic with gastrointestinal bleeding or hepatic encephalopathy. Operation time over 520 minutes and resection length over 31mm were predictors of anastomotic stenosis [42].
Snyder et al reported long-term venous patency rates after reconstruction of seventy two percent at a median follow up of 7 months. [25]. Patients with portal vein thrombosis suffered 24.3 months of worse overall survival. Median overall survival of the subjects without portal vein thrombosis was 35.0 months [43]. Prosthetic grafts were associated with a 4 times increased risk of early portal vein thrombosis. The role of anticoagulation for these patients is still not clear [44]. In a retrospective review of 128 subjects who went through portal vein resection and reconstruction during pancreatectomy, survival of subject was 66% at one year. The use of a prosthetic graft was associated with a worse survival [45]. Alternatives to prosthetic grafts could be the use of bovine pericardium and cold-stored cadaveric venous allograft. PV reconstruction with the extern iliac vein or peritoneum has also been reported [27, 46]. In a retrospective review from Norway, no changes in post-operative morbidity and mortality were seen when comparing reconstructions with cold-stored cadaveric venous interposition allografts or primary end-to-end anastomosis after segmental vein resections. In addition, 18.6 months was the assessed median overall survival in subjects who obtained venous allografts & 20.5 months in the other group [47, 48, 49]. In a recent paper from Germany, the histopathological infiltration of the portal vein was analyzed as an outcome factor. Considerably higher metachronous liver metastasis incidence was seen in subjects with true vein invasion. 11.9 months was the median overall survival for these subjects & for those patients without true venous invasion it was 16.1 months [50]. Subjects with poorly differentiated tumours after venous resection had a shorter life span in comparison to those with well & moderately differentiated pancreatic cancer who had longer life span (12.5 months median survival vs. 24.5 months, P=0.023) [51]. Thus, pancreatic surgery with vein resection alone cannot change the tumour biology. Thus, perioperative treatment and intensified chemotherapy regimens, including individualized therapy targeting the metabolic reprogramming in cancer cells, will be more and more important [52].
Arterial Resection
Ever since fortner first proposed the idea as part of regional pancreatectomy, since then arterial resection for PDAC has become a subject of controversy. Venous resection & reconstruction are quite common nowadays when the pancreatic tumour can't be isolated from the adjacent portal vein or superior mesenteric vein. Nevertheless, due to the high rates of mortality & morbidity related to arterial resection & reconstruction, several researchers consider the invasion of hepatic artery, the celiac axis of the superior mesenteric artery, as a contraindication to surgery [53, 54]. Lately, with the rise of effective systemic treatments, emphasis is been focused on the possible advantage of primary tumour resection, even in the complex arterial abutment or encasement setting, particularly when it is the only site of measurable disease, after neoadjuvant treatment [55]. Even though in some subjects arterial invasion is classified as borderline resectable as per the ISGPS consensus statement, an upfront resection is recommended rarely, even though it can be conducted technically [18]. In addition, arterial invasion typically predicts considerable mesenteric neural plexus involvement with the incapability to attain a negative margin of retroperitoneal resection even with radical extended surgery. In short, arterial resection can be safely performed by skilled hands, but so far up to now it is not represented as standard method of treatment.
Summary
In comparison to no resection, PD with venous resection particularly with R0 resection increases survival. When compared to PD with no vascular resection, morbidity & mortality rates are greater in PD with venous resection. With respect to PD with venous resection after neoadjuvant therapy, poorer oncological outcome is seen in PD with upfront venous resection (increased R1 resection risk, poorer rate of survival). PD with arterial resection is linked to higher rates of mortality & morbidity (than venous resection PD) and hasn't really proven to be of any benefit. A distal splenopancreatectomy with celiac axis resection is related to higher rates of mortality & morbidity & the oncological advantage of this method hasn't been demonstrated clearly. Today, literature offers further encouragement for neoadjuvant treatment in pancreatic cancer management. The objective ought to be to wait for outcomes of RCTs which includes clearly resectable tumours, neoadjuvant treatment as well as a complete R0 resection in all subjects needing planned vascular resection with (or with no) reconstruction. Such subjects ought to be handled during pancreatic resection by a skilled team in both pre-operative/neoadjuvant treatment & vascular resection. Not every center has such skills/experience hence creating another strong issue for regionalizing complex cancer care involving multiple remedies.
Key Recommendations
For operative planning, CT with intravenous augmentation is the proper imaging modality, but for searching liver metastasis, MRI is considered better.
To reduce the time of liver ischemia, venous resection ought to be performed at the end of resection.
The most utilized suture material is Prolene 5/0
Direct anastomosis is the preferential approach for reconstruction in segmental resection cases.
Left renal vein is the ideal graft
Regular heparin use is controversial- with subcutaneous 40 mg enoxaparin application twice daily, this could be changed.
Pancreatic cancer has had a poor prognosis history due to its late detection. A family history of pancreatic cancer carefully monitored with a genetic screening has the ability for predicting the early detection, expected incidence & potential pancreatic cancer management. In addition, further screening modalities & examination with imaging techniques & interventional radiology use have helped enhance early detection and pancreatic cancer management. Resection at an early disease stage of pancreatic cancer is the best chance of cure. Venous resection and reconstruction have become a standard technique to achieve negative margins. In complex venous resections/reconstructions it is highly advisable to seek the help of experienced vascular surgeons.
All named authors hereby declare that they have no conflicts of interest to disclose.