Review Article - (2019) Volume 20, Issue 2
Mar Achalandabaso Boira1, Luis Ferreira2, Caroline Conlon3, Kevin C Conlon3
1St Vincent´s University Hospital, Dublin, Ireland
2Queen Elisabeth Hospital, Birmingham, United Kingdom
3Department of Surgery, Trinty College Dublin, Dublin
Received Date: January 16th, 2019; Accepted Date: February 25th, 2019
Introduction Pancreatitis can be associated with walled off necrosis and fistula resulting in significant morbidity and mortality. We present a case of a patient without previous history of abdominal pain or acute pancreatitis who, while being investigated with respiratory symptoms, was diagnosed with lung cancer and was found to have a Pancreatico-colonic fistula. The aim of the study was to perform a systematic review on pancreatico-colonic fistula and assess if conservative management can be possible in specific situations. Material and Methods Available literature in English was reviewed until January 2019. PRISMA guidelines were followed identifying 91 records. After screening, seven papers reporting seven patients were identified as definitive pancreatico-colonic fistula and included. All of these were case-reports. Results-Case report A sixty-seven-year-old man with smoking history and strong alcohol intake presented with weight loss and non-productive cough. There was no prior history of pancreatitis or significant abdominal pain. A chest x-ray, showed a left upper lobe pulmonary lesion. Computed tomography demonstrated an abnormal pancreas with intra-panrenchymal gas along body and tail tracking back towards the transverse colon. A gastrografin enema showed pancreatic duct filled with contrast retrogradely through the transverse colon. As he was asymptomatic from the pancreatic standpoint a conservative approach was adopted. Literature review Eight cases (including the authors`) were identified, 3 were incidental, 3 were following recurrent pancreatitis and 2 were diagnosed after laparotomy. Our case appears to be the first that presented without a prior history of acute pancreatitis. Treatment was conservative in 3, endoscopy in 3 and surgical in 2 cases. Resolving fistula in follow up occurred in 6 and all patients were alive at the time of the publications. Discussion Pancreatico-colonic fistula is rare and potentially fatal complications. Our case is unique as the patient presented with no prior history of pancreatitis. As in our case, a conservative, non-operative course is appropriate in selected patients.
complications; Pancreatitis, Chronic; Pancreatic Fistula
CBD common bile duct; CT TAP CT toraco-abdominopelvic; CXR chest x-ray; IPN infected pancreatic necrosis; PCF pancreatico-colonic fistula; PD pancreatic duct; OTSC over the scope clips; WON walled off necrosis
Pancreatitis is an acute inflammatory process of the pancreas with variable grades of severity [1]. It can be severe and associated with local and/ or systemic complications. Colonic complications are well known and present in 1-3.3% of all patients with acute pancreatitis, increasing to 15% in severe cases [2, 3], particularly in those with necrotising pancreatitis or walled off necrosis (WON). It is thought to occur as a consequence of pancreatic or peripancreatic inflammation and infection and can also be secondary to percutaneous drainage or surgical debridement of pancreatic necrosis [4]. Typical clinical manifestations are diarrhoea, hematochezia, and fever.
We present a case of an incidental diagnosis of a pancreatico-colonic fistula (PCF) in a patient without documented episodes of acute pancreatitis. The literature on the topic was reviewed assessing presentation, diagnosis and management. The aim of the study was to identify this rare but potentially dreadful entity and if conservative management can be possible in specific situations.
A literature search was undertaken using PUBMED as search engine including all papers published in English until January 2019 and the references were cross-checked for additional studies. The MESH headings used were pancreatic fistula, colonic fistula, acute pancreatitis, colonic complications. The target of the search was to identify articles providing data on patients with acute, chronic or acute on chronic pancreatitis who suffered as complication PCF defined as clear communication from pancreatic duct (PD) to colon visualised in computed tomography (CT), CT with soluble contrast enema, ERCP or colonoscopy and that reported type of management performed. Exclusion criteria were defined as fistula aetiology unrelated with pancreatitis, lack of appropriate imaging capable to clearly define communication from PD to colon, fistula from colon to pancreatic abscess, infected pancreatic necrosis (IPN), WON or pseudocyst, not specifically communicating with pancreatic duct and articles in a different language than English.
The PubMed search with the Mesh headings previously stated provided 32 records and another 59 were obtained by cross reference. No duplicate records were identified. Articles were reviewed following the PRISMA guidelines. 91 records were screened by title and 29 were excluded because were unrelated to the topic, not in English, reporting fistula communicating pancreas to skin or peritoneum, related to splenic artery pseudoaneurysm or due to ingestion of corrosive. 62 full-text articles were assessed for eligibility. 55 were excluded due to no reported defined fistula from PD to colon (13 records described fistula to pancreatic abscess/IPN/ WON, 10 records described fistula to pancreatic pseudocyst and in 32 records diagnostic image consisted only in plain film abdominal X ray or the CT/ERCP/colonoscopy could not clearly define communication from PD to colon). Finally, 7 papers were identified for full examination and analysis. All of those were single case reports (Figure 1).
Case Report
We present a sixty-seven-year-old man with no known previous medical history but a 60 pack year smoking history and excess alcohol intake that presented to our hospital with significant weight loss, non-productive cough, short of breath and worsening of his basal status over the last few weeks. There was no history of abdominal pain, pancreatitis, diarrhoea or previous surgical interventions. On admission, his chest x-ray (CXR) showed a suspicious left upper lobe lesion with a left basal pleural effusion. A computed tomography scan of the Chest, abdomen and pelvis (CT TAP) showed a 4.2 cm enhancing mass in the left upper lobe consistent with a primary lung neoplasm. There was also extensive pancreatic parenchymal calcification predominantly in the pancreatic head with ductal calculi and pancreatic duct dilatation.
Three weeks after presentation he complained of right sided abdominal pain. A clinical diagnosis of possible biliary colic was made and a biliary ultrasound was performed. This demonstrated a contracted thick walled gallbladder. In addition, the pancreatic duct was again noted to be dilated with a suggestion of an obstructing pancreatic head mass (Figure 2a). To clarify those findings a CT pancreatic protocol was performed which showed extensive pancreatic parenchymal calcification predominantly in the pancreatic head, with ductal calculi and a pancreatic duct which was dilated measuring 1 cm maximal diameter. A focal pancreatic mass was not identified. In the body and tail of the pancreas, there was gas evident within the pancreatic duct itself and also adjacent to the pancreatic duct in the tail. The gas adjacent to the pancreatic tail tracked back towards the distal transverse colon and there appeared to be a fistula to the lumen of the colon. In addition, there was a rimenhancing fluid collection adjacent to the spleen which measured 3.2 × 6.1 cm in maximal transverse diameter. There was associated moderate left pleural effusion with left lower lobe collapse and a small right pleural effusion. Neither focal liver lesions nor biliary ductal dilatation was seen. Gallstones were noted in the contracted gallbladder (Figure 2b). A gastrografin enema was performed where the pancreatic duct was seen to fill with contrast as the contrast filled retrogradely through the transverse colon. The fistula appeared to arise at approximately the level of the splenic flexure (Figure 2c). Finally, a colonoscopy ruled out any possible colonic neoplasm but failed to identify the fistula orifice.
Figure 2: (a). US Pancreatic duct dilatation. (b). CT pancreas. The gas adjacent to the pancreatic tail tracks back towards the distal transverse colon and there appears to be a fistula to the lumen of the colon. (c). Gastrografin enema. The pancreatic duct was seen to fill with contrast as the contrast-filled retrogradely through the transverse colon. The fistula appears to arise at approximately the level of the splenic flexure.
No active cause for the PCF was demonstrated. There was a long standing history of alcohol excess but no prior hospital admissions with abdominal pain or pancreatitis.
Review of the Literature
Out of 91 records identified only 7 cases reported a true PCF. Patients were predominantly male (7/8), with a mean age of 60.4 years (range 42-78 years). A prior history of alcohol abuse was present in all but one patient. No comorbidities were stated. Presentation was chronic pancreatitis in 3/8 cases, bowel obstruction in one case and abdominal pain in 2 cases. Two of eight cases were found incidentally on CT findings and one following a ERCP. Two patients were diagnosed following a laparotomy for pancreatitis. Our case was the only one that presented without a prior history of pancreatitis, or prior surgery. Aetiology was given as alcohol-induced pancreatitis in seven cases and gallstone disease in one. In all cases, the transverse or left colon was the area affected. Computed tomography was the initial diagnostic test in 6/8 patients and in 3/8 patients findings were confirmed with watersoluble contrast enema. ERCP was the diagnostic tool in more than half of the cases (5/8) and colonoscopy was used as the main diagnostic or confirming test in 2/8 cases (Table 1).
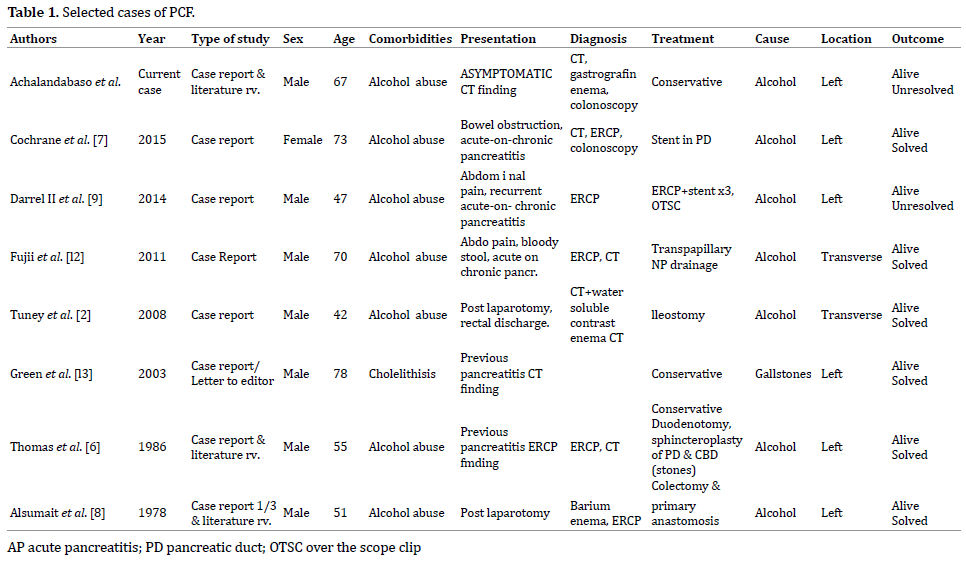
Patient details are as shown in Table 1. Treatment was varied and heterogenous. Observation was adopted in 3/8 cases, endoscopic management (pancreatic duct stent, over the scope clips-OTSC-, transpapillary nasopancreatic drainage, hemoclippings and glue injection) in 3/8 and surgical resection in 2/8 cases. Duodenotomy, sphincteroplasty of the pancreatic duct (PD) and common bile duct (CBD) was performed in one case with gallstone aetiology but no invasive treatment was directed to the fistula, which healed with conservative management. Two cases were diagnosed post-laparotomy. The first patients presented with severe alcoholic pancreatitis, underwent laparotomy for refractory sepsis, were a necrosectomy was performed and colonic involvement at the descending portion of the colon was discovered. Drainage and ileostomy were carried out. Following the surgery presence of persistent pancreatic juice discharge through the anus led to suspect a PCF, that was confirmed by CT with contrast enema, same technique after six months showed spontaneous closure, therefore, the ileostomy was closed. The second patient presented after 2 years of the first episode of severe acute pancreatitis with colonic resection and primary anastomosis, with abdominal pain, fever and diarrhoea and a barium enema revealed extravasation from the colon to the stomach and an ERCP confirmed fistulous tract beyond the pancreas that communicated with both the stomach and the colon. Underwent relaparotomy with colonic resection, primary anastomosis and pancreaticojejunostomy and choledochojejunostomy.
Patients were successfully treated with resolving fistula in follow up imaging in 6/8 cases, all patients being alive at the time of the respective publications. In our case, only observation was performed and although the fistula is not resolved, the patient is still asymptomatic from the abdominal point of view at 14 months of follow up.
Colonic complications associated with acute pancreatitis are rare but carry an increased risk of mortality when delayed diagnosis and treatment. Incidence varies between 3.3% to 15% depending on the severity of pancreatitis as described in Mohamed et al. [5]. PCF is most commonly associated with walled-off pancreatic necrosis or abscess formation and rarely forms spontaneously, it can also be associated with pancreatic duct disruption. Percutaneous interventional drainage of infected peri-pancreatic collections as well as surgical procedures is associated with an increased incidence.
Classic clinical manifestations for pancreatic colonic fistula include diarrhoea, hematochezia, and fever. The rapid disappearance of a previously noted abdominal mass, especially if associated with gastrointestinal bleeding, is very suggestive of the development of pancreatic duct to colon fistula [6]. Hematochezia is the most common clinical manifestation found in 60% of patients and is associated with a mortality rate of 50-77% [4, 7]. Clinical detection of colonic complications occurs relatively late in the disease course as demonstrated in our series where 3 patients presented with acute on chronic pancreatitis and 2 patients post laparotomy after former episodes of pancreatitis.
Regarding diagnosis, there is variability among modalities utilised. Computed tomography seems to be the standard initial technique, it can show air fluid levels in the pancreatic duct or directly visualize a fistula to the colon with or without a classical cut-off sign that has also been described in plain films [6]. A contrast enema is an important study when consideration of a colon abnormality arises in patients with known or suspected pancreatitis. Some studies claim ERCP as the gold standard to be done once PCF is suspected [2, 7]. The pancreatogram usually demonstrates tortuosity of the pancreatic duct with extravasation of contrast from the tail of the pancreas into the colon confirming a pancreatic duct-colonic fistula. ERCP can also be therapeutic when used to place a stent in the pancreatic duct or for nasopancreatic drainage. Nevertheless, it is an invasive technique that could be avoided with a water-soluble enema, which can also be sensible and specific, being less aggressive [2, 8]. Colonoscopy should be performed to rule out underlying malignancies since both clinical scenarios can have common symptoms. Despite all the possible imaging techniques in some cases will only be diagnosed intraoperatively. It is apparent that diagnosis of this particular complication can be difficult, therefore, a high index of suspicion must be maintained in patients with severe acute pancreatitis with ongoing disease, in particular, individuals with persistent sepsis, significant diarrhoea or gastrointestinal haemorrhage.
Treatment in the acute/emergency situation has traditionally been surgical or more lately interventional radiology since patients may be haemodynamically unstable [9]. In a retrospective study by Kochhar et al. [10], the investigators found that all patients admitted to their unit over a 4-year period with acute pancreatitis and fistulisation to the colon underwent surgery. However, this review suggests that in fact haemorrhage is an infrequent presentation and surgery was seldom required. Similar data has been reported by Ito et al. [3] where conservative treatment has been shown to be successful in selected patients. Successful non-surgical management options have emerged in the last 20 years, with greater utilization of percutaneous and endoscopic techniques. Endoscopic options for PCF include ERCP with pancreatic sphincterotomy and pancreatic duct stenting, fibrin glue, clips, nasopancreatic drainage or dual modality drainage (percutaneous and endoscopic drainage simultaneously or combined endoscopic and video-assisted retroperitoneal pancreatic debridement). The treatment of large fistulas may require the use of several different endoscopic tools together.
The incidence of GI fistula is much higher in patients that had a surgical intervention prior to being transferred to the referral centre [11]. To an extent the site of fistula dictates the management approach with small bowel fistulas closing spontaneously whereas many colonic fistulas may require active intervention such as percutaneous drainage, endoscopic therapy or surgery (resection with or without diversion). Although it has been shown that colonic fistulas which became apparent after percutaneous pancreatic drainage might close spontaneously [11]. The mortality has been reported to be similar in patients with and without GI fistula [4] although Jiang et al. reported higher mortality in the subgroup of colonic fistula [11].
Our patient developed a PCF without the classical history of prior pancreatitis. He was essentially asymptomatic, required no intervention and remains well on follow-up. Close surveillance is required as these patients are at increased risk of developing exocrine and endocrine insufficiency in the long term.
The authors recognise the limitations of this review. This literature review identified a heterogeneous series of retrospective case reports; the time frame between the first and the last article is more than fifty years, with all the developments and experience gained in the different fields namely endoscopy, interventional radiology, surgery and intensive care management occurring during that timeperiod.
Even though the cases reported were a small number we feel that there is sufficient encouraging experience with endoscopic and interventional radiology to consider conservative management and avoid surgery in selected patients as well as choosing a watch and wait approach, as it may provide a survival benefit for patients that present with a stable condition. Multidisciplinary decision and treatment in high volume centres is mandatory.
PCF fistula can be a common observation in patients with complicated acute pancreatitis being a rare incidental finding in our patient since no episodes of abdominal pain were reported and no infected pancreatic collections or other complications were identified in the imaging performed. Treatment can vary from a watch and wait approach in asymptomatic cases, different endoscopic techniques or surgical resection with or without anastomosis, mainly in symptomatic patients with colonic haemorrhage. To our knowledge, this is the first asymptomatic case of PCF described in the literature, although other cases might have been misdiagnosed in asymptomatic patients. It is infrequent since PCF’s are generally symptomatic and associated with severe necrotising pancreatitis.
All authors are in agreement with the content of the manuscript. There is no conflict of interest.