Key words
black and minority ethnic (BME)
groups, cultural competence, devolution, mental
health, Wales
Introduction
Over the past two decades, research has shown that
factors such as ‘race’ and ethnicity, socio-economic
status and geographic location impact on the level of
access to mental health information and treatment, as
well as on the utilisation, experience and knowledge of
mental health and social care provision (Sashidharan,
1993; Smaje, 1996; Bhugra et al, 1997; Fernando et al,
1998; O’Connor andNazroo, 2000; Arai and Harding,
2002). It is also increasingly evident that how services
are used and experienced by individuals from different
ethnic groups is just as much a product of their own
beliefs, needs and expectations as it is a product of the
attitudes and perceptions of service providers (Owens
et al, 1991;Nazroo, 1997). Stereotypical views of black
and minority ethnic (BME) people, racism, and cultural
ignorance have been shown to undermine the
way in which health and social care service providers assess and respond to minority ethnic patients and
clients (Currer, 1994; Cochrane and Sashidharan, 1996).
Some, therefore,must struggle with a health and social
care system that is not yet adequately equipped to
respond to their needs, despite statutory obligations
and legal requirements (Lloyd and Fuller, 2002). These
disparities suggest that ‘mainstream’ mental health
services may be failing to meet the needs of BME
people, resulting in a spiral of disaffection, reluctance
to seek help and re-admission to hospital in times of
crisis (Secker and Harding, 2002). In a recent publication
on the perceptions of African and African-
Caribbean service users by Keating et al (2003), this
was explained as ‘circles of fear’, with staff members
perceiving service users as potentially dangerous, and
service users perceiving services as harmful.
Socially ascribed differences such as ‘race’, ethnicity,
and religion have become increasingly significant
considerations for mental health practitioners, as well
as health policy makers. Recent drivers include the
Race Relations (Amendment) Act 2000 that insists
that public authorities provide a quality of service to
BME groups that does not exclude and discriminate.
Also important are recent publications such as Inside
Outside: improving mental health services for black and
minority ethnic communities in England (Department
of Health, 2002), Delivering Race Equality: a framework
for action (Department of Health, 2004) and
Delivering Race Equality in Mental Health Care: an
action plan for reform inside and outside services and the
Government’s response to the independent inquiry into
the death of David Bennett (Department of Health,
2005). Although these documents differ in their focus
and emphasis, taken together they aim to provide the
framework for achieving equality of access, experience
and outcomes to BME mental health service users in
England (Bhui et al, 2004).
Like all public services in the UK, in Wales, attempts
are being made to critically appraise the NHS, and
work to ensure that a robust and responsive service is
provided to all members of the population. According
to the 2001 Census, the number of people from BME
backgrounds in the UK was 4.6 million (7.9% of the
total population). Out of a population of approximately
2.9 million people in Wales, in 2001, 2.1%
(60 900) were from BME backgrounds. Since 1991,
there have been increases in the proportion of African,
Indian, Pakistani, Bangladeshi, and Chinese people
living in Wales, as well as an increase in the number of
people who classified themselves according to ‘Mixed’
categories listed in the census classification system.
Although there are pockets of BME people living
throughout Wales, the minority ethnic population is
largely concentrated in urban areas of the south east,
with by far the largest concentrations in Cardiff and
Newport (25 700 and 6600, respectively), accounting
for over half the total and representing 8.4% and 4.8%,
respectively, of census-enumerated population in these
two local authority areas.
The challenge to modernise mental health services
in Wales is great. In a report on mental health trusts
in the UK, the Commission for Health Improvement
(since taken over by the Healthcare Commission)
stated that both policy and services are less developed
in Wales, and that an older, more institutional model
of care is prevalent (Commission for Health Improvement,
2004, p. 6). Added to this is the dearth of
knowledge about the health and healthcare needs of
BME groups (Aspinall, 2003; Walters, 2004). Although
there is anecdotal evidence to suggest that Englandbased
studies have relevance in Wales, there remain
major gaps in our knowledge of the mental health
needs of BME people in Wales. Equally important, there remain major gaps in our knowledge of the
perceptions of health and social care practitioners
seeking to provide appropriate mental health information
and care.
It is also important to note that Wales has a long
history of minority ethnic settlement. Thus, the histories,
settlement patterns, residential status and occupational
profiles of BME groups in Wales are different
from those elsewhere in the UK, and it is important to
consider the particularities of the Welsh context when
examining the health and social care of BME groups.
Of importance is the ‘hyper (in)visibility’ of BME
groups: the awareness and acceptance in Wales of the
long-established presence of diverse ethnic groups,
which exists alongside a lack of attention to the impact
of such diversity on Welsh society and which works to
render BME groups invisible. In their recent analysis
of contemporary Welsh society, Williams et al (2003)
note that although there is an increasing focus on
diversity and equality in public policy, this paradox
remains. On the one hand, there is a renewed interest
at policy level, research and in the media while a
plethora of policy statements carry the statement and
ethnic minorities. On the other hand, there is growing
awareness of disenfranchisement, compounded by
marginalisation, widening inequalities and widespread
racism.
However, devolution has opened up new opportunities
for assessing and addressing equality issues.
Policy shifts in Wales have led to the amalgamation of
health and social care policy making. With constitutional
reform, the equality of opportunity directive
has been thrust to centre stage and, as Chaney and
Fevre (2002) suggest, the merits of the ‘Welsh model’
equality duty are based on the fact that it is allembracing
in scope, requires government to be proactive
in all equality matters, and conveys legally
enforceable rights. Coupled with the requirements of
the Race Relations (Amendment) Act 2000, this statutory
framework suggests a strong equalities context
within which to develop effective and appropriate
health and social care strategies for all population
groups in Wales.
Aims of the BE4study
This paper reports on one aspect of a two-year study:
the perceptions of mental health nurses, social
workers and other health and social care professionals
in relation to the quality of access to mental health
information and care given to BME people in a large
Welsh city. The BE4 study was the first study in Wales
since devolution that sought to examine and provide
a baseline of evidence of the mental health information
and care needs of specific BME groups. Drawing on the census classification system, further links
were made to the following subgroups: black African,
Bangladeshi, African/black Caribbean, Chinese, Indian
and Pakistani. The South Asian subgroups were expanded
into the following ethno-religious categories:
Pakistani Muslims, Bangladeshi Muslims, Punjabi
Sikhs and Gujarati Hindus. Other subgroups that
reflected the city’s demography that were added include
Somali, Sudanese and Yemeni.
The funding for the study was secured by a national
BME mental health voluntary organisation who commissioned
a university in south east Wales to conduct
the study. The wider aims of the BE4 study were as
follows:
• to carry out a needs assessment in order to provide
a baseline of evidence of the mental health and
social care information and treatment needs of the
target groups
• to identify gaps in access to service provision and
care, making recommendations in how to develop
a multi-agency, multi-sector, multi-professional
practice framework.
Methodology and ethical
considerations
In keeping with the aims of this project, a mixed
research methodology was used, one that drew on
aspects of action research and qualitative data collection
to explore, describe and develop an understanding
of the experiences of a sample of health and social
care/welfare professionals. The sample was purposive,
with snowballing technique/reference sampling also
employed (see Table 1). Recruitment was targeted at
the following organisations and services: local statutory
community mental health teams (CMHT), as well as health, mental health, social care and welfare professionals
including midwives, general practitioners (GPs),
alternative health therapists, community workers and
researchers. Health and social care professionalsworking
in the equalities sector were also invited to participate.
The inclusion and exclusion criteria reflected the aim
to develop a sample of practitioners, professionals,
advocates and researchers based in the health, social
care/work and equalities statutory and non-statutory
sectors in Wales, who worked with a significant number
of people from the targeted BME backgrounds. A
significant majority of people interviewed worked in
the front-end of services, and were seeking to address
the immediate and often complex needs of individuals
they were in direct contact with in a pressurised, often
understaffed and under-resourced working environment.
Approval to conduct this study was obtained from
the local research ethics committee, the NHS trust
covering the area where the study was conducted, and
the university research ethics committee. A letter of
invitation and an information leaflet were provided
for each potential participant, detailing the aims of
the study, what was to be required in terms of time
commitment, and what was to happen to the data
collected. The leaflet also stated that participation was
entirely voluntary, and that all data would be anonymised.
All participants were required to sign a consent
form prior to the interview, and were given two to
threeweeks to decide whether they wished to be part of
the study.
An interview protocol was developed and was
divided into a number of topics. The topics covered
in the interviews with this group of participants
included: working with a diverse client base; solutions
to specific issues; the role of non-statutory services;
and commissioning and management issues. BE4 staff
conducted the interviews. Flash cards with key phrases
taken from the interview protocol were also used to help generate discussion. Unlike a list of questions,
cards can be shifted around and exchanged between
the interviewee and the interviewer, and this makes
them a great interactive tool. Designed to look like a
deck of cards, the block text on the cards was in a range
of colours (maroon, aqua, purple, blue, green, and
yellow), and each colour represented a key research
theme and topic to be discussed. The cards were useful
in that they allowed people to ‘handle’ key concepts
and use the cards to guide the discussion.
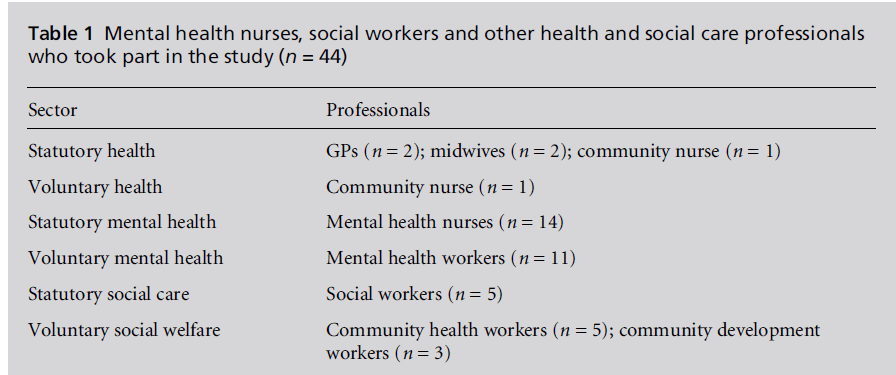
Table 1: Mental health nurses, social workers and other health and social care professionals
who took part in the study (n = 4 4 )
Analysis of data
The interviews were tape recorded and transcribed
verbatim. Data analysis was conducted using an inductive
approach: the constant comparative method
(Maykut and Morehouse, 1994). Relevant themes
within the text were gradually identified, compared
and coded. Two members of the research team took
part in the analysis of the data. The NVivo computer
software package was used to help in the coding process.
The research literature and list of topics underpinning
the interview schedule were used to help refine the
themes. Several themes emerged from the data that are
of importance to this paper: ‘addressing common
barriers’, ‘working with a diverse client group’, ‘ethnic
monitoring and patient profiling’, and ‘strong managerial
leadership’. Each theme is discussed below, with
excerpts taken from the data gathered from the participants.
It was considered important to make use of
direct quotations that allow the voices of the participants
to be heard.
Addressing common barriers
Several key issues were raised under this theme. The
first was the use of terminology in a multi-ethnic
setting, and the fact that terms, especially mental
health terms, do not easily translate across cultures
and languages. With this came confusion as to the
range of mental illnesses understood in western psychiatry
and psychology, which had led to the rejection
of the term mental health used by some health professionals.
As one mental health nurse commented:
‘Well one of the clients we have, when she was first
referred, she asked why she had to come to us and I said
because this is a mental health project and she became
almost hysterical and said ‘‘what do you mean, mental
health? Mental health!’’, and I said, ‘‘oh you suffer with
depression don’t you’’, and she said ‘‘oh depression’’.
Depression was acceptable but the label mental health
wasn’t and I have seen that in other people ... the word
mental health is not used.’
Secondly, the awareness of stigma was understood by
some of the participants to be an important element
that shaped how people from BME backgrounds
approached and engaged with services. It was clear
that there was an awareness of the fact that social
rejection of people with mental illness labels included
rejection from community activities, leisure pursuits,
employment, and relationships.A mental health nurse
put into context the stigma often associated with
mental health. As the respondent stated:
‘It is a very uncomfortable term and it is a label, a stigma ...
I know it is in wider society, but I think the people we work
with it is even harder ... I think it is because of this word
[pointing to the next card] ‘‘community’’ and their status
and position in the community and I think that plays a
major role ... the link with community and being part of
the community ...’
For another respondent, a mental health nurse, it was
important to see the link between stigma and wider
societal discrimination, racism and social exclusion
that work to layer, in particular ways, the care given to,
and expected by, people from BME backgrounds. As
the respondent stated:
‘BME patients go through discrimination and when the
stigma of mental illness is attached to them, it is what I call
double discrimination ...’
A third issue identified as a common barrier was that
of language and communication barriers. This was
an overwhelming concern for all those interviewed.
Although a common and often noted problem, this
issue was considered of particular importance for
older people from BME communities, including those
from the Caribbean who might speak Patois or English
with a strong accent. From the perspective of one
respondent who worked in BME community health
and social welfare, and who provided information to
people who could speak and read English, there is
more to consider than the provision of information
in relevant languages. It is also important to provide
appropriate messages. As she stated:
‘I kept saying to them [my clients] ... these leaflets are in
your GP practices within your surgeries or if you go to the
hospitals you could ask for this information ... and what
people have talked about is, yes there are leaflets around ...
but the leaflets are not something that we could relate to
straight away."
Working with a diverse client group
More proactive mental health nurses, midwives, social
workers and social welfare professionals appeared to
take pride and have added confidence in personal
engagement strategies. It is a skill that has to not only be built on, but used in everyday practice, as explained
by one participant:
‘I certainly think it is something that can be built upon ...
it is one thing knowing the theory, it is another thing
knowing it in practice. The fact that I am working in
[areas] with the highest ethnicity mixes [in Wales] throws
you into the middle of something and you suddenly have
to embrace and understand quickly ... you have to find a
way to change your thinking and processes to accommodate
them.’
Moreover, the development of more responsive, appropriate
care and treatment models that are linked,
but not necessarily rooted in the dominant western
medical model remains an important theme to emerge
in relation to this group’s work with their diverse
client groups, as the following excerpts highlight:
‘Other concerns are what examples [there are] that might
be culturally transferable ... It is finding examples to get
that point over is the hardest. It is just a bit of, you try
something, it works, you try something else, it doesn’t ... It
is a bit of trial and error ...’
Another respondent stated:
‘I would like a lot more on culturally appropriate ways of
dealing with issues that affect the communities we work
with, you know, issues that are their priority rather than
our priority.’
Linked to this is the need for ongoing, practical
training to supplement and build up into a professional
competence the skills needed to work with a
diverse client base:
‘There is information that gives you understanding of
people’s beliefs, but how [do] those beliefs impact on your
professional interactions? [I am] very aware of issues to do
with public holidays and religious festivals and things like
Ramadan and times that we could visit people, but very
often those have been picked up by trial and error rather
than [via] a particular training package.’
Ethnic monitoring and patient
profiling
Although many participants were aware of the importance
of ethnic monitoring, there is clear indication
that the structures and training for effective and
useful data collection are presently lacking. As one
health and social care service manager, explained:
‘Yes a real bugbear with me. Our social workers just refuse
to do it sometimes, and as far as I am concerned, the
argument’s been won, there is very good reason for
monitoring ethnicity. It is one of the mandatory fields
and yet they say they are too embarrassed to ask, which is
ridiculous.Weask them whether they are incontinent, but
not what their ethnic origins are.’
For others, the issue was not only ethnic monitoring,
but the importance of patient profiling, being aware of
the ethnic, cultural, social and environment factors
which impact on one’s mental health, as highlighted
by the comments made by two service managers
‘It might be someone who is white who is Welsh ... we
actually need to consider what their background is as to
whether they need a female or a male or a nurse or social
worker, or whoever, in that they might have been
traumatised through domestic violence ... You don’t
know about people’s experiences, so if you have got that
information along with the ethnicity then that again helps
meet that patient’s needs.’
The second manager stated:
‘We are beginning to keep data on ethnicity in respect of
access. We are at quite an early stage ... [but] we don’t
record it adequately and one of my jobs is to try and look
at developing the system so we do actually do that 100% of
the time ... [You] can’t actually deduce a great deal from
what we have at present, apart from anecdotally. If we
don’t know what the need is we can’t meet it and that is
not just about Race Relations Act, that is also about care
planning ... That is the kind of thing we need to do, we
need to make sure that it is happening in an organised
way.’
A related concern is the need to put all these issues into
a broader, albeit specific context, as one participant
stated:
‘[I] think we could probably do more in terms of broader
training about services to black and ethnic minority
people because I don’t think services have got a full view
of their responsibilities ...’
With this was the long-standing and well-established
evidence base underpinning the need for changes in
how services are designed.
Strong managerial leadership
One flash card that sparked comment was ethnicity
agenda. Most comments centred on the need for
clarity, the need in Wales for leadership and the
need for support from above. The following excerpt
highlights some of the tensions involved in seeking to
make change and the need for clear leadership:
‘My perception is that they are keen to turn things around,
but I just wonder how able they are to have mechanisms to
change things around. It raises a question mark because it
hasn’t happened to date. I know it is a really big issue ...
but we have to plan how to change some services in mental
health ... but there are no drivers ... there are no project
managers to see it through.’
Discussion and conclusions
In presenting the findings, it is important to note one
important limitation of this study: the small number
of people interviewed means that generalisations cannot
be made. What the findings offer, however, is a
snapshot of evidence that can be used to contribute to
and informthe ‘normative base of policy and practice’
(Cortis, 2004), with regard to enhancing the quality of
access to mental health information and care available
to BME people in Wales.
The findings highlighted a number of key points.
First, despite the diverse professional backgrounds
and numerous sites in which the participants worked,
there was a general awareness of the barriers faced
by people from BME backgrounds and strategies to,
when appropriate, adapt care to be congruent with the
client’s needs. Second, it became evident that there are
a number of gaps that need to be addressed. From the
findings, it is evident that the more proactive health
and social care professionals we interviewed had an
understanding of the cultural mores of their clients,
making effective use of interpreters, gaining the support
of BME health workers, and building up links
with relevant BME voluntary mental health organisations
and community groups – all key aspects of
providing care in a multicultural context. However,
there were, at the same time, limited indications of
reflection about these strategies or ongoing training to
augment skills in order to ensure that professionals
were open to encounters with a range of people, and
could competently assess and development appropriate
care packages.
It is also important to note that although a significant
number of those interviewed were proactively
working to find positive strategies to delivering care in
a multi-ethnic, multicultural setting, there were
people who were less aware and engaged. Strategies
for improving the quality of information and care are
being developed, but remain highly individualised,
patchy and isolated.
Many of the participants acknowledged the need to
promote good practice and use it to underpin the
development of practice frameworks that not only
address, but provide action plans for, improving existing
services and developing new services. This did not,
however, translate into having such good practice
readily available and accessible, highlighting the need
for the strategic implementation of an equalities and
diversity agenda which cascades throughout the mental
health services. From the data it is clear that the
work to embed issues of equality and diversity on a
strategic level and to ensure that organisational frameworks
are put in place in order to foster and support
both clients and staff has yet to be completed.
Finally, the hyper in/visibility of BME people in
Wales (south east Wales in particular), devolution and
the new opportunities for assessing and addressing
equality issues, coupled with the formalised amalgamation
of Wales health and social care policy making
are all key to understanding (i) the general consensus
of the participants of the need to incorporate cultural
sensitivity in their practice; and (ii) the lack of operational
frameworks to change practice and foster
competent care. Although operating within a rigorous
overarching equality framework, there are in Wales no
regional or national strategies or policies specifically
intended to improve the mental health of minority
ethnic groups or the care and treatment they receive
from mental health services (Saltus and Kaur-Mann,
2005). Thus, unlike other parts of the UK, health
advocates, mental health practitioners, as well as
managers and commissioners in Wales do not yet
have to hand the sharp teeth of a specific policy that
most often underpins national operational directives
and the development of new practice frameworks.
Research to increase the evidence base in this area
and the development of policies and practice frameworks
rooted in an equalities agenda are necessary if
the integrated health and social care system in Wales is
to truly become robust enough to appropriately address
the mental health needs of its increasingly
diverse population.
ACKNOWLEDGEMENTS
The author would like to thank all the participants
who took part in the BE4 study. Also special thanks to
the AWETU All Wales BME Mental Health Group
who commissioned the study, the Welsh Assembly
Government who funded the study, and Kalbir Kaur-
Mann, the BE4 staff member who conducted most of
the interviews.
CONFLICTS OF INTEREST
None.
References
- Arai L and Harding S (2002) Health and Social Care Services for Minority Ethnic Communities in the United Kingdom: a review of the literature on access and use. Occasional Paper No 9. Glasgow: Research Medical Council.
- Aspinall P (2006) A Review of the Literature on the Health Beliefs, Health Status, and Use of Services in the Minority Ethnic Group Population and of Appropriate Health and Social Care Interventions. Cardiff: Welsh Assembly Government.
- Bhugra D, Leff J, Mallett R et al (1997) Incidence and outcome of schizophrenia in whites, African-Caribbeans and Asians in London. Psychological Medicine 27:791–8.
- Bhui K, McKenzie K and Gill P (2004) Delivering mental health services for a diverse society. BMJ 329:363–4.
- Chaney P and Fevre R (2002) An Absolute Duty. Equal opportunities and the National Assembly for Wales. Cardiff: Institute of Welsh Affairs.
- Cochrane R and Sashidharan S (1996) Mental Health and Ethnic Minorities: a review of literature and implications for services in ethnicity and health. York: NHS Centre for Reviews and Dissemination.
- Commission for Heath Improvement (2004) What CHI has Found in Mental Health Trusts. A sector report. www. healthcare-commission.org.uk/_db/_documents/04000051. pdf (accessed 10 August 2006).
- Cortis J (2004) Cultural Diversity. Managing society’s difference and diversity. Multicultural Nursing. Sample issue:13–18.
- Currer C (1994) Pathan women in Bradford – factors affecting mental health with reference to racism. International Journal of Social Psychiatry 30:72–6.
- Department of Health (2002) Inside Outside: improving mental health services for Black and Minority Ethnic communities in England. London: Department of Health.
- Department of Health (2004) Delivering Race Equality: a framework for action. London: Department of Health.
- Department of Health (2005) Delivering Race Equality in Mental Health Care: an action plan for reform inside and outside services and the Government’s response to the independent inquiry into the death of David Bennett. London: Department of Health.
- Fernando S, Ndegwa D and Wilson M (1998) Forensic Psychiatry, Race and Culture. London: Routledge.
- Keating F, Robertson D, McCulloch A and Frances E (2003) Breaking the Circles of Fear. A review of the relationship between the mental health services and African and Caribbean communities. London: The Sainsbury Centre for Mental Health.
- Lloyd K and Fuller E (2002) Use of services. In: Sproston K and Nazroo J (eds) Ethnic Minority Psychiatric Illness Rates in the Community.
- Department of Health. London: The Stationery Office. Maykut P and Morehouse R (1994) Beginning Qualitative Research: a philosophic and practical guide. London: The Falmer Press.
- Nazroo J (1997) Ethnicity and Mental Health: findings from a national community survey. London: Policy Studies Institute.
- O’Connor W and Nazroo J (2000) Ethnic Differences in the Context and Experience of Psychiatric Illness: a qualitative study. London: The Stationery Office.
- Owens D, Harrison G and Boot D (1991) Ethnic factors in voluntary and compulsory admissions. Psychological Medicine 21(1):185–96.
- SaltusRandKaur-MannK(2005) Black and minority ethnic mental health service users in Wales: a snapshot of their views. Mental Health Nursing 25(5):4–7.
- Sashidharan S (1993) Afro-Caribbeans and schizophrenia: the ethnic vulnerability hypothesis re-examined. International Review of Psychiatry 5:129–44.
- Secker J and Harding C (2002) Users’ perceptions of an African and Caribbean mental health resource centre. Health and Social Care in the Community 10(4):270–6.
- Smaje C (1995) Ethnic residential concentration and health: evidence for a positive effect? Policy and Politics 23(3): 251–69.
- Smaje C (1996) The ethnic patterning of health: new directions for theory and research. Sociology of Health and Illness 18(2):139–71.
- Walters V (2004) Health, well-being and access to health and social care of selected minority groups. Unpublished paper presented to the Selected Minority Groups Task and Finish Group, Welsh Assembly Government.
- Williams C, Evans N and O’Leary P (2003) A Tolerant Nation? Exploring ethnic diversity in Wales. Cardiff: University of Wales Press.