- (2010) Volume 11, Issue 6
Omar Javed Shah1, Irfan Robbani3, Showkat A Zargar2, Ghulam N Yattoo2, Parveen Shah4, Sadaf Ali1, Gul Javaid2, Altaf Shah2, Bashir A Khan2
Departments of 1Surgical Gastroenterology, 2Medical Gastroenterology, 3Radiodiagnosis and Imaging, and 4Pathology; Sher-i-Kashmir Institute of Medical Sciences. Srinagar, Kashmir, India
Received July 19th, 2010 - Accepted August 24th, 2010
Context The pancreas is an infrequent site of hydatid disease. Objective This study aims at giving better insight into the diagnostic and managerial approach to the disease. Patients Six patients with hydatid cysts of the pancreas. Design Retrospective review of the clinical records. Results The six patients (four men, two women) ranged in age from 18 to 68 years. Five of the cysts were primary while one had an associated cyst in the liver. Abdominal pain, vomiting, abdominal mass and dyspeptic symptoms were seen in cysts involving the body and tail. Two patients having cysts in the head of the pancreas presented with obstructive jaundice. An indirect hemagglutination test and an enzyme-linked immunoabsorbent assay were positive for the presence of specific hydatid antibodies in four patients. Abdominal ultrasonography, computed tomography and magnetic resonance cholangiopancreatography (MRCP) successfully imaged the cysts and also defined the relationship of the lesion with the pancreatic duct. All patients underwent surgical exploration. Three patients had intraoperative fine needle aspiration cytology of the cystic lesion for microscopic and electrolyte analysis. A preoperative diagnosis was possible in two patients and, in the other four, the diagnosis was made intraoperatively and confirmed on histopathological examination. Patients with cysts located in the tail underwent a distal pancreatectomy with a splenectomy while those with cysts in the body had a pericystectomy or central pancreatectomy. Cysts of the head were treated with evacuation, partial cystectomy and tube drainage. There were no postoperative complications, and no evidence of cyst recurrence was observed during the follow-up period. All the patients were followed up at three-month intervals with a mean follow-up time of 58.7 months (rang: 4-120 months); no patient had cyst recurrence or dissemination. Conclusion A hydatid cyst is an uncommon cause of cystic lesions in the pancreas and should be included in the differential diagnosis of cystic lesions of the pancreas, especially in endemic areas. Intraoperative fine needle aspirate for microscopic and electrolyte estimation seems to be an effective method for establishing a proper diagnosis. MRCP, which can depict the communication of the cystic lesion with the pancreatic duct, helps in defining the type of surgical treatment. Cysts in body and tail are best treated by resectional methods whereas, for those in the head region, a cystectomy with simple drainage is a simple, quick and effective solution.
Echinococcosis; Pancreatectomy; Pancreatic Cyst
Echinococcosis is one of the world’s most widespread parasitic zoonoses, with transmission occurring in countries boarding on the Mediterranean as well as those in Asia, South America and Oceania [1, 2]. The liver is the first and the main barrier to parasitic embryos which migrate from the intestine and gain access to the portal circulation. The majority of the embryos are thus trapped in the liver and some pass over to the lungs or any other part of the body; the liver and the lungs are the most frequently involved organs [3]. A hydatid cyst of the pancreas is uncommon; the incidence reported is less than 2% [4, 5]. Because of its rareness and a considerable overlap of imaging features, a preoperative diagnosis is usually difficult. Management may be difficult as a hydatid cyst in the head of the pancreas may closely simulate a cystic tumor. In this study, we report our experience with six cases of hydatid cysts involving the pancreas.
The records of all patients treated for hydatid disease from January 2000 to January 2010 in the Department of Surgical Gastroenterology at Sher-i-Kashmir Institute of Medical Sciences, Srinagar, Kashmir, India were reviewed. During this 10-year period, a total of 340 patients owithhydatidosis were treated, only six (1.8%) of whom had isolated hydatid disease involving the pancreas. Besides recording their complete medical history and clinical examination findings, all these patients were routinely subjected to various laboratory tests and imaging examinations. The laboratory tests included a complete blood count, serum biochemistry, liver function tests and serum amylase level estimations. Serological techniques, such as indirect hemagglutination test, enzyme linked immunosorbent assay (ELISA) and Casoni’s test, were also carried out on all patients. Radiological tests included a plain Xray of the abdomen, abdominal ultrasonography, computed tomography (CT) and magnetic resonance cholangiopancreatography (MRCP). All patients underwent surgical treatment and the diagnosis was confirmed by exploration. After protecting the operative field by gauze soaked with a scolicidal agent, aspiration of the cyst content was also undertaken in three cases using a 22 gauge disposable needle; the aspirate was collected in a plastic syringe and evaluated for color, sodium, potassium and chloride content. Smears obtained directly from the aspirated fluid as well as from centrifuged deposits were routinely stained with Leishman’s stain and examined under the microscope. Tissue specimens were collected for histopathological examination in order to confirm the diagnosis. After being discharged, all patients were followed up by means of routine hospital visits or telephone contact.
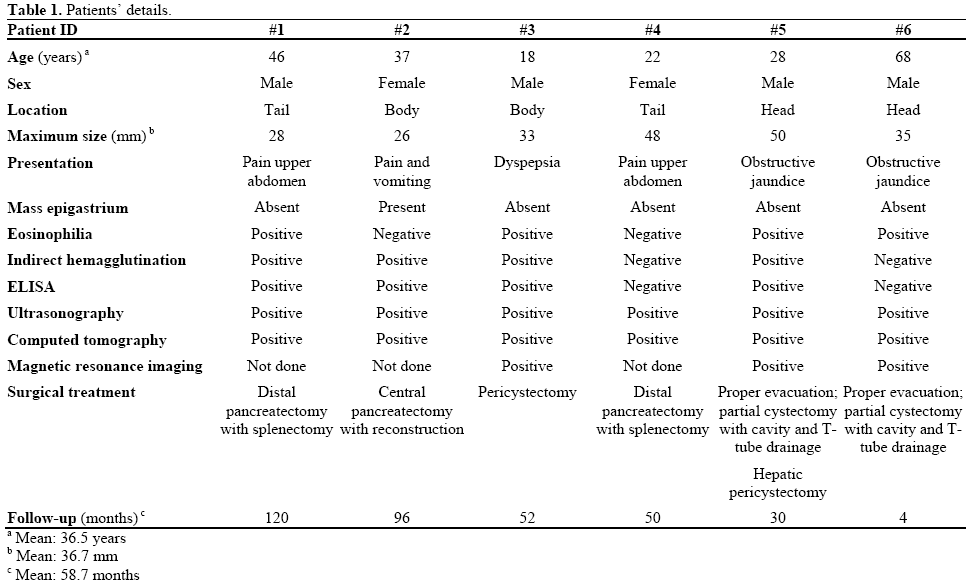
The six patients studied included four men and two women; their ages ranged from 18 to 68 years (mean 36.5 years; Table 1). The clinical presentation of patients was determined by the site of the cyst involving the pancreas. Abdominal pain, vomiting and dyspeptic symptoms were predominantly noted in the cysts involving the body and tail of the pancreas. Two patients presented with obstructive jaundice due to the extrinsic compression of the common bile duct. A palpable upper abdominal swelling and tenderness was noted in one patient having a cyst in the body of the pancreas. Eosinophilia was observed in three patients, and elevated bilirubin and alkaline phosphatase levels were found in two patients presenting with obstructive jaundice. An elevated level of serum amylase (610 U/L; reference range: 25-125 U/L) was also observed in one patient with obstructive jaundice. Indirect hemagglutination and ELISA tests were positive for the presence of specific hydatid antibodies in four patients but Casoni’s test was positive in only two patients. Plain X-ray of the abdomen revealed classical curvilinear calcification in only one patient with a hydatid cyst in the pancreatic body (Figure 1). Ultrasonographic examination which recorded the site, size and extent of the lesions, documented the cystic lesions as anechoic rounded structures in all cases. An abdominal CT scan documented the cysts as spherical hypodense space-occupying lesions. All the lesions were solitary, measuring 26-50 mm in diameter (mean 36.7 mm). Five lesions were cystic with thin walls and one lesion appeared as a multiseptated cyst. Magnetic resonance imaging for defining the lesion and its relationship with the pancreatic duct was performed in three patients (two lesions in the head and one in the body of the pancreas). Two lesions were located in the head (Figure 2, 3, 4, 5), two in the body (Figures 6 and 7) and two in the tail region of the pancreas (Figure 8). In two cases, a preoperative diagnosis was possible due to the presence of classical features which also included a concomitant hydatid cyst in the liver in one patient. All patients underwent surgical exploration; intraoperative cyst puncture for aspiration cytology was successful in three cases (two cases with cysts in the head and one case with a cyst in the body of the pancreas); the results of cytological examination were positive in all cases. A fragmented laminated membrane was observed in two patients, scoliosis in three and hooklets in one patient (Figure 9). The laminated membrane was seen as a foliated, acellular, pale, eosinophilic structure which stained strongly positive with periodic acid Schiff staining and negative with alcyan blue staining. The hooklets had a characteristic shape presenting as a blade, a guard and a root. They were not stained with Papanicolaou stains and their appearance was enhanced by turning down the microscope condenser. There were no complications after diagnostic aspiration. In all three cases, the aspirated fluid was colorless and contained a mean sodium level of 128 mEq/L (range: 128-130 mEq/L), chloride level of 69 mEq/L (range: 65-70 mEq/L) and potassium level of 5.8 mEq/L (range: 5.4- 6.3 mEq/L). Cysts in the distal pancreas observed in the two patients were treated by a distal pancreatectomy with splenectomy. Cysts in the body were treated by a pericystectomy in one patient (Figure 10) and a central pancreatectomy in another patient. Cysts in the head region in two patients were treated with evacuation, partial cystectomy and tube drainage of the cavity after protecting the surgical area with a scolicidal solution (Figure 11). Both patients underwent T-tube drainage of the common bile duct; there was rapid regression of the jaundice in these patients. The T-tube cholangiogram confirmed the free flow of bile into the duodenum; the tubes were eventually removed in the third postoperative week. Postoperative confirmation of the hydatid cysts was obtained on the basis of the histopathological findings. There were no postoperative complications; all patients recovered uneventfully. The antihelminthic drug, albendazole, was administered postoperatively (10 mg/kg body weight/day) in all cases for a period of 6 months. All the patients were followed up at threemonth intervals and each patient underwent clinical examination, abdominal ultrasonography and indirect hemagglutination tests; no patient had cyst recurrence or dissemination. The mean follow-up time was 58.7 months (range: 4-120 months).
Figure 2. Contrast-enhanced computed tomography scan showing whorled appearance of a hydatid cyst in the region of pancreatic head (thick arrow) causing atrophy of the pancreatic parenchyma with a dilated duct (arrow head) anterior to the splenic vein (curved arrow). Note another hydatid cyst in segment VI of the liver with separation of the membranes (thin arrow) (Patient #5).
Echinococcosis is a cosmopolitan zoonotic problem of man caused by the larval stage of the cestode of the genus Echinococcus. Infection of the intermediate host caused by ingestion of the eggs of Echinococcus granulosus (cystic hydatidosis) leads to the development of hydatid disease characterized by the appearance of hydatid cysts. Normally, Echinococcus granulosus completes its life cycle involving dogs (definitive host) and sheep and goats (intermediate hosts). Man serves as a intermediate dead-end host and is affected by hydatidosis. This can happen only when man consumes vegetables contaminated by the excreta of infected stray dogs. Most cysts are acquired in childhood and are not diagnosed until the third or fourth decade of life; only about 10 to 25% of cases present in childhood [6]. In the present study, one patient was under 20 years of age. Hydatid cysts which may develop anywhere from the toe to the crown of the head, are commonly located in the liver and less commonly elsewhere; pancreatic involvement is occasional and is estimated to range from 0.14 to 2% [4, 5, 7, 8]. Even inside the pancreas, the location of the hydatid cyst is not uniform; its distribution pattern being 57% in the head, 24% in the body and 19% in the tail [9, 10]. However, in the present study involving six cases, the distribution of the cyst was even, two cases were located in each of the head, body and tail regions of the pancreas. Clinical presentation varied according to the anatomical location of the cysts. Cysts in the body or tail were virtually asymptomatic and presented only as a swelling with potential for subsequent effects. A cyst in the head could present with obstructive jaundice due to extrinsic compression of the common bile duct; only a few cases of this nature have been reported in the literature [7, 8]. In the present study, we encountered two patients with hydatid cysts in the pancreatic head, presenting as obstructive jaundice.
Due to compression of the pancreatic duct from a hydatid cyst located in the head region, recurrent acute pancreatitis rarely occurs [11]. Although such a presentation was not observed in this study, the MRI findings of one patient revealed gross dilatation of the pancreatic duct due to local compression by the hydatid cyst in the head region. The routine laboratory investigation of all cases of hydatid cysts in the pancreas was non specific except for the presence of eosinophilia. Specific serum antibodies or circulating antigens detected by a variety of immunodiagnostic techniques, indirect hemagglutination assay, immunoelectrophoresis and co-electrophoresis confirm the diagnosis in 50 to 94% cases of hepatic hydatidosis and in 65% cases of pulmonary hydatidosis [12]. In this study, indirect hemagglutination and ELISA tests were positive in only four cases. Casoni’s intradermal test has been abandoned owing to its relatively poor diagnostic accuracy. False positive results have been reported in healthy individuals from endemic areas and also in patients affected by other parasitic infestations [13]. The positive tests need confirmation using the arc 5 immunodominant and specific antigen (antigen 5) of the cestode. There is no cross reaction of this test with other non cestode parasites. Following treatment, the antibody titers start falling at 3 months and eventually become negative within a period of 12-24 months [14]. Although the presence of cystic lesions in the pancreas are easily detected by ultrasonography, CT and MRI modalities, all these methods have limited sensitivity in making a specific diagnosis because of the considerable overlap of imaging findings. Recent results suggest that the diagnostic accuracy of ultrasonography in abdominal hydatidosis is in the range of 93-98% [15]. The demonstration of daughter cysts and hydatid sand by ultrasonography favors the diagnosis of hydatid disease. Nevertheless, the diagnosis of a hydatid cyst in the pancreas may be possible on the basis of imaging findings alone but not without a high index of suspicion. The presence of a thickened and more laminated wall than that of a simple cyst and a thin layer of calcification within the lesion associated with a liver hydatid may suggest a pancreatic hydatid. In this study, two patients with similar features were diagnosed as hydatid pancreas cases preoperatively. Besides the characteristic epidemiological setting, the features suggestive of pancreatic hydatidosis include the presence of: a) daughter cysts and typical egg-shell cyst wall calcification on abdominal radiography; b) an undulating double lining membrane demonstrated by ultrasonography, CT or MRI; or c) peripheral eosinophilia and positive hydatid serology [16, 17]. MRI, due to its higher soft tissue contrast and multiplanar capability, gives better differentiation among cystic neoplasms and furthermore, it can better depict the fluid content of cystic lesion and communication with the pancreatic duct. These findings in pancreatic hydatids may help in designing the type of surgical procedure preoperatively (drainage or resectional procedure). Although fine needle aspiration biopsy cytology of the cystic lesion has been recommended as a method of differentiating hydatid cysts of the pancreas from other cystic lesions, it carries a potential risk of needle tract or peritoneal dissemination of the viable parasite or neoplastic cells [18]. Accidents of this kind are known to have occurred following rupture or puncture with coarse needles during surgery [19, 20] but have not been reported after fine needle percutaneous punctures [21]. In endemic areas, it is always advisable to assume that it may be a hydatid cyst even if laboratory tests are negative. In the present study, three cysts (two in the head and one in the body of the pancreas) underwent intraoperative fine needle aspiration for diagnostic purposes. All these cases were diagnosed as positive on the basis of microscopic examination; the electrolyte values of the cystic fluid supported the diagnosis. Similar hydatid fluid electrolyte values have been reported in other studies [22]. The differential diagnosis of a cystic lesion in the pancreas includes an entire range of conditions which, besides the pseudocysts, includes cystic neoplasms, such as serous and mucinous cystadenoma, cystadenocarcinoma, cystic islet cell and papillary cystic tumors, and solid tumors. Cystic lesions are rarely associated with polycystic disease, lymphoepithelial cysts or vascular tumors (hemangiomas or lymphangiomas). It must be remembered that the majority (80%) of cystic lesions are pseudocysts and 10% are potentially curable cystic neoplasms which require complete excision [23]. Radiological features, cyst fluid analysis and even operative differentiation with frozen section biopsy may not always succeed in differentiating between various cystic lesions; the policy of complete excision of an unidentified cystic lesion of the pancreas seems justified. Surgical treatment is the method of choice for treating pancreatic hydatidosis; nevertheless, percutaneous drainage of the cyst using hypertonic (20%) saline lavage has been shown to be successful in one report [8]. Of course, the type of surgical treatment for pancreatic hydatidosis depends on the site of the lesion. Resection of the cyst is the ideal method but it is not always feasible and may cause hemorrhage owing to the adherence of the cyst wall to the pancreatic parenchyma. Furthermore, a pancreatic fistula may develop after a partial cystectomy when there is communication between the cyst and the pancreatic duct; a Roux-en-Y pancreaticojejunostomy is recommended in such cases [16]. When a lesion is located in the tail, as was seen in two of our cases, a distal pancreatectomy seems to be an effective surgical procedure; cysts located in the body of the pancreas can undergo a central pancreatectomy. One patient underwent such a procedure in this series and similar treatment was instituted in one additional case which has been reported [24].
Central pancreatectomy has recently been introduced as the best method for the surgical management of pancreatic hydatid cysts located in the body and neck region [24, 25]. The rationale for a central pancreatectomy is to remove the cystic lesion, preserve functional parenchyma and avoid major pancreatic resection. Thus, there is no risk of diabetes or exocrine insufficiency and the upper digestive and biliary anatomy is maintained with consequent digestive, immunologic and coagulative advantages. A pericystectomy is rarely performed because hemorrhage and pancreatic fistulas may be a concern. One patient in this study, who underwent a pericystectomy, had no communication of the cystic lesion with the pancreatic duct as was confirmed preoperatively on MRCP. Cysts located in the head of the pancreas have been treated by various methods, such as a Whipple resection [26], marsupialization and external drainage [27]. Other methods, such as ideal or partial cystectomy and cystoenteric anastomosis, have also been used, with their advantages and disadvantages [28]. Two patients in this series with cysts in the head region had intraoperative fine needle aspiration of the cyst fluid. On examination, the cyst fluid was found to be positive for scolices and electrolyte estimation (lower sodium and chloride values and higher potassium values). The electrolyte content of hydatid cyst fluid can be explained by the large number of parasitic cells present in the cyst and by associated cell lysis. These patients, who underwent preoperative MRCP in order to visualize the relationship of the lesion with the pancreatic duct, were treated by simple excision with drainage of the cavity. This type of treatment for cysts located in the head region presenting with obstructive jaundice seems to be quick, simple and effective; similar results have been reported by others who have followed this line of treatment in such cases [29].
Recurrence is one of the major problems in the management of hydatid disease. It is defined as the appearance of new active cysts following treatment for intra- or extra-hepatic hydatid disease. The failure to achieve permanent elimination of the primary cystic lesio treated is considered to be the cause of local recurrence. We believe that the most effective method for preventing postoperative recurrence is radical surgery. However, this may be indicated only in patients meeting the desirable criteria in terms of age, location of cyst and the relationship of the cyst to the vasculature and other vital anatomical structures.
In conclusion, it may be stated that a hydatid cyst of the pancreas is an infrequent condition. It may present with obstructive jaundice, upper abdominal pain and/or a mass. Although radiological methods may help in diagnosing cystic masses in the pancreas, confirmation of the diagnosis and appropriateness of treatment are best established during a laparotomy. In cystic lesions of this nature, especially those in the head region, intraoperative fine needle aspiration for cytology and electrolyte estimation seems to be an effective method for establishing a proper diagnosis, and MRCP, which can depict the communication of the cystic lesion with the pancreatic duct, helps in defining the type of surgical treatment. A central pancreatectomy may offer an excellent method for treating lesions located in the body and the neck region of the gland.
Conflict of interest The authors have no potential conflict of interest