Keywords
Spontaneous coronary artery dissection, Iintramural hematoma, Coronary wall, Acute coronary syndrome, Coronary angiography
Abbreviations
ACS: Acute Coronary Syndrome; AMI: Acute Myocardial Infarction; BB: Beta-Blockers; BRS: Bio-Resorbable Scaffolds; CABG: Cardiac Artery Bypass Graft; CCB: Calcium Channel Blockers; CCTA: Coronary Computed Tomography Angiography; DAPT: Dual Antiplatelet Therapy; DES: Drug Eluting Stents; FMD: Fibromuscular Dysplasia; IMH: Intramural Hematoma; IVUS; Intravascular Ultrasound; OPT: Optical Coherence Tomography; PCI: Percutaneous Coronary Intervention; SCAD: Spontaneous Coronary Artery Dissection; SES: Sirolimus Self- Expandable Stent
Introduction
Definition
Spontaneous coronary artery dissection (SCAD) is defined as spontaneous separation of the coronary wall layers, not related to trauma, medical procedures, or atherosclerosis. The dissection causes the blood entry in the vascular wall with the consequent formation of false lumen and intramural hematoma (IMH) [1].
Epidemiology
The first case of SCAD was an autopsy report described in 1931 by Pretty [2]. A better awareness of the disease and the improvement of coronary diagnostic imaging has over time led to an increased number of diagnoses. In the coronary angiography era SCAD prevalence has risen from 0.2% to 1.1% [3,4] to 1.7% to 4% according to more recent reports [5,6]. The prevalent occurrence of SCAD in women has also been well documented: Vanzetto reported a 8.7% prevalence of SCAD in women younger than 50 years in a series of more than 10000 acute coronary syndrome (ACS) patients [7].
Same prevalence (9%) has been recently confirmed by a Canadian study, conducted in a population of young women (<50 years) who underwent coronary angiography [8]. Moreover, Nakashima et al. recognized SCAD as the cause of acute myocardial infarction (AMI) in 35% of women under 50 years, while Elkayam et al. showed that SCAD is the most common cause of pregnancy-related AMI (mean age 34 years), especially in the third trimester of pregnancy or in postpartum period [9,10]. A gender preference seems thus unquestionable: women cover about 90% of the diagnosed SCAD with a mean age of 44-55 years and similar involvement of all races [5,9,11].
Pathogenesis
SCAD can affect any layer of the vascular wall: intima, media or adventitia. Two pathogenetic mechanisms have been proposed to explain the spontaneous separation of the vascular wall layers: the “primary” laceration of coronary endothelium and the rupture of the vasa vasorum, both leading to IMH; the consequence of blood accumulation inside the vascular wall is the reduction of coronary flow within the true lumen and an impaired myocardial perfusion [12].
Many non-atherosclerotic conditions can promote or precipitate SCAD, as documented in literature. Fibromuscular dysplasia (FMD) is an inflammatory non-atherosclerotic vascular disease strongly associated with SCAD and should be always investigated [13-16]. Pregnancy is also considered a condition predisposing to SCAD; this association may be due to the drastic hemodynamic changes and the increase of several hormone levels [17,18]. In particular, progesterone levels elevation alters the fibro-elastic composition and collagen production of the vascular wall, while the increase of estrogen drives a pro-thrombotic state [19,20]. Pregnancy and chronic use of hormonal therapies are indeed considered contributory causes of SCAD [21,22].
Chronic inflammatory diseases, such as polyarteritis nodosa, Crohn’s disease, ulcerative colitis, sarcoidosis, Churg-Strauss syndrome, Wegener’s, granulomatosis, rheumatoid arthritis, giant cell arteritis, celiac disease could cause SCAD through a long term vasculitic process [1,23,24].
Also, some connective tissue disorders, such as Ehlers- Danlos syndrome, systemic lupus erythematosus, Marfan syndrome, cystic medial necrosis, alpha-1 antitrypsin deficiency, polycystic kidney disease, seem to contribute significantly to the development of SCAD because of an alteration of the elastic fibers composition of coronary wall [1,25,26].
In addition to the over-exposed conditions favoring the development of SCAD, numerous stressful events, such as intense physical exercise and use of sympathetic-mimetic substances, could represent precipitating factors [27-31]. The underlying pathogenetic mechanisms include the intense release of catecholamines and the increase of intra-abdominal pressure, due to prolonged Valsalva-like activities, leading to an increase of coronary arteries shear stress and amplified risk of rupture of intimal wall or vasa vasorum.
Clinical Aspects and Diagnosis
Clinical aspects
Clinical presentation and severity of manifestations is variable in patients with SCAD, depending on the degree of reduction of the true lumen, and the number and extension of the involved vessels [32]. For this reason, patients affected by SCAD could be either completely asymptomatic or present with ACS, cardiogenic shock, cardiac arrest or sudden cardiac death, although this fatal presentation seems to be underestimated [33,34]. Most patients presenting to medical attention manifested typical symptoms of ACS (chest pain, nausea, vomiting, diaphoresis, dyspnea) sometimes accompanied by the increase of cardiac enzymes [35].
The increase of cardiac necrosis markers is often mild, as demonstrated by a Japanese study that emphasizes a less extensive myocardial damage in the presence of SCAD rather than of atherosclerotic lesions; as a supporting evidence, left ventricle ejection fraction during hospitalization for SCAD is better preserved and likely to rise in the follow-up [9,36].
Diagnosis
Coronary angiography
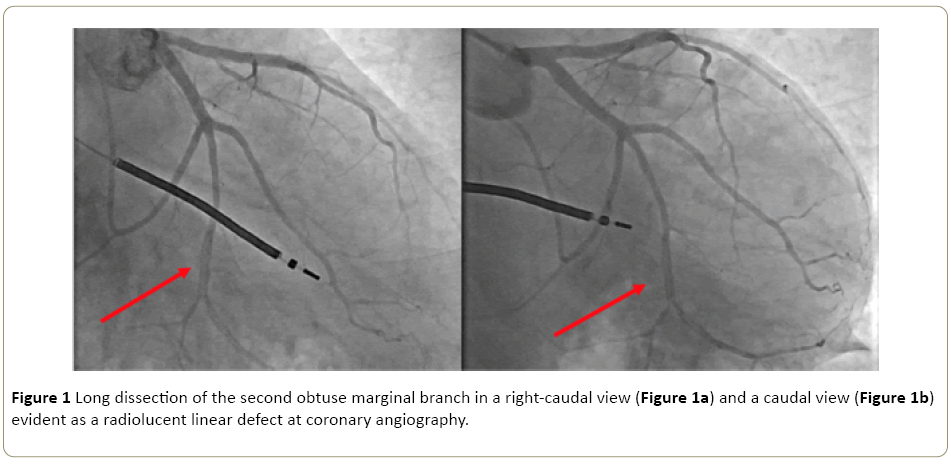
Coronary angiography is the first-line examination in order to identify and type a SCAD; classic angiographic features include extraluminal contrast spreading, multiple lumens and reduced intraluminal filling [37-40] (Figure 1a and 1b). Saw et al. recognized and classified three different subtypes of SCAD on the basis of coronary angiography: type 1 detects the pathognomonic lesion of SCAD characterized by intimal lesion with false lumen evidence; type 2 describes the presence of widespread and long stenosis (typically >20 mm) limited either to the area of IMH (type 2A) or involving the coronary in toto (type 2B); type 3 concerns a focal stenosis (<20 mm) similar to an atherosclerotic lesion and, therefore, worthy of further investigations such as intracoronary imaging [1].
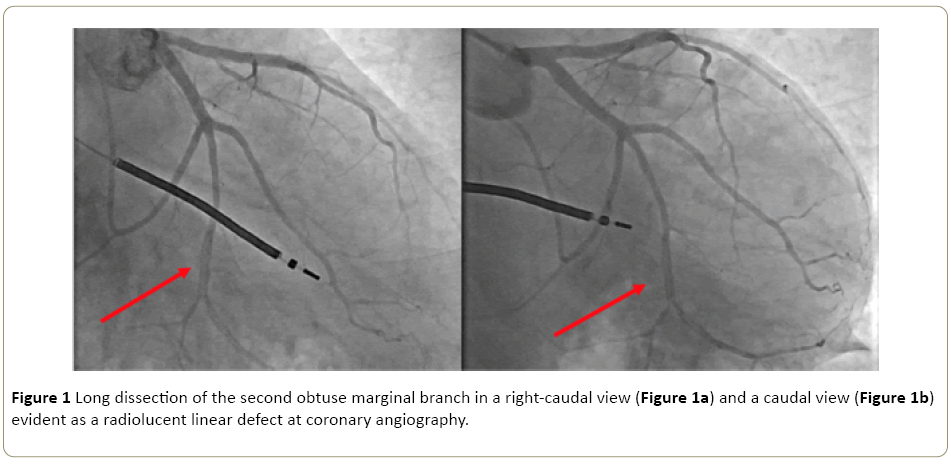
Figure 1: Long dissection of the second obtuse marginal branch in a right-caudal view (Figure 1a) and a caudal view (Figure 1b) evident as a radiolucent linear defect at coronary angiography.
In consideration of this angiographic classification, Saw proposed a diagnostic algorithm for suspected SCAD including both clinical and anamnestic elements: absence of atherosclerotic risk factors, ACS in young women (<50 years), history of FMD, chronic inflammatory or connective tissue diseases, recent physical or emotional stress [41]. If angiographic evidence of false lumen allows an easy diagnosis of type 1 SCAD, in absence of this pathognomonic sign a careful assessment of the angiographic lesion is needed: a type 2 SCAD should be considered if coronary stenosis length is >20 mm and can be confirmed by intracoronary nitroglycerin injection, and a possible repeated angiography after 4-6 weeks; if coronary stenosis is conversely shorter than 20 mm, the distinction from the classical atherosclerosis stenosis becomes challenging and an intracoronary imaging exam should be performed, especially if the suspicion is supported by the absence of atherosclerotic disease in other coronary arteries, and in presence of long (11 mm to 20 mm) and linear stenosis. The most frequent angiographic subtype is type 2 in 67.5% of cases, followed by type 1 in 29.1% and type 3 in 3.4% of cases.
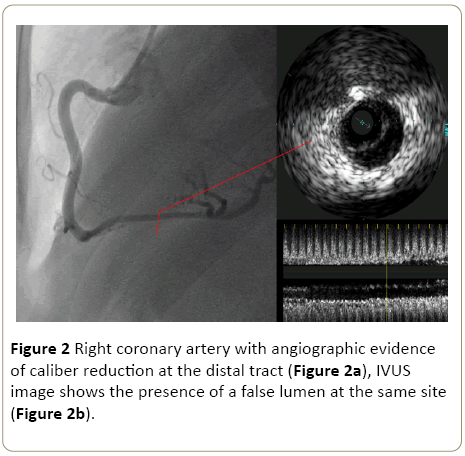
Every coronary segment may be potentially involved but Virmani et al. documented a significantly higher involvement of left anterior descendent (70% to 75% of cases) followed by the right coronary artery (20% of cases); a remarkable predilection for distal and smaller tracts has been also described [42-44]. A gender difference has moreover been reported with left anterior descendent more frequently involved in females, while right coronary artery in males [45,46] (Figure 2).
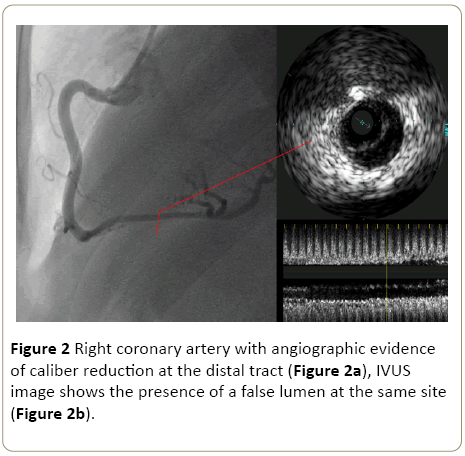
Figure 2: Right coronary artery with angiographic evidence of caliber reduction at the distal tract (Figure 2a), IVUS image shows the presence of a false lumen at the same site (Figure 2b).
Intravascular imaging: As stated above a two-dimensional image of the lumen, supplied by the coronary angiography, is sometimes not exhaustive if SCAD is suspected; new intravascular imaging techniques, such as optical coherence tomography (OCT) and intravascular ultrasound (IVUS), are able to improve the diagnostic accuracy of coronary angiography by providing direct and detailed visualization of the coronary wall [47-49].
OCT utilizes the effects of the light for the evaluation of intracoronary structures. However, since the blood distorts OCT images, the injection of a iodinated contrast agent is necessary during the acquisition. OCT has a considerable spatial image resolution (10 μm to 20 μm) and is therefore able to distinguish all the anatomic features of a SCAD: intimal flap, intraluminal thrombus, false lumen and IMH. Nevertheless, OCT is limited in the ability to observe the entire extension of IMH by the poor optical tissue penetration (1 mm to 2.5 mm) [50,51].
The currently most accessible alternative to OCT is represented by IVUS, that is based on the ability of a piezoelectric crystal to emit ultrasounds which interact with tissues and adjacent structures and are reflected to a transducer with production of images. IVUS has a discrete image resolution (100 μm to 200 μm) but a greater tissue penetration (about 5 mm): when compared to OCT, it allows a better assessment of the false lumen and of the IMH extension but is less effective in evaluating the intima interface [52] (Figure 2a and 2b).
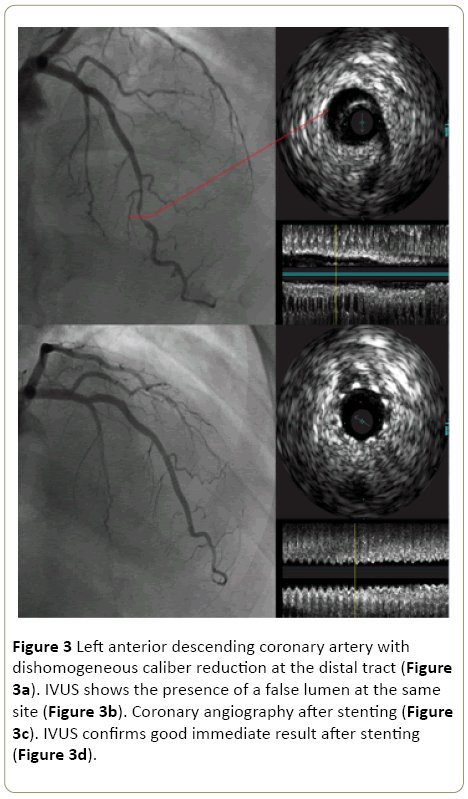
For these reasons, OCT is the intravascular imaging technique of choice in the evaluation of SCAD for its ability to identify the IMH and the double lumen, also considering the limited clinical benefit of assessing the exact transverse extension of IMH [53]. Moreover, these techniques are also helpful in evaluating the proper deployment of either the stent or the bioresorbable scaffold (BRS) if a percutaneous coronary intervention is chosen (Figure 3a-3d). Conversely, although these intracoronary imaging techniques can definite the diagnosis of SCAD, facilitate and guide the correct placement of coronary devices, confirm adequate coverage of the coronary dissection, they are not riskless. The introduction of IVUS or OCT catheters and the injection of a contrast agent for OCT may indeed cause the extension of the dissection and a complete catheter-induced occlusion of the vessel. About the use of these extremely advanced diagnostic tools a careful evaluation of the case by case risk/benefit ratio is thus advocated.
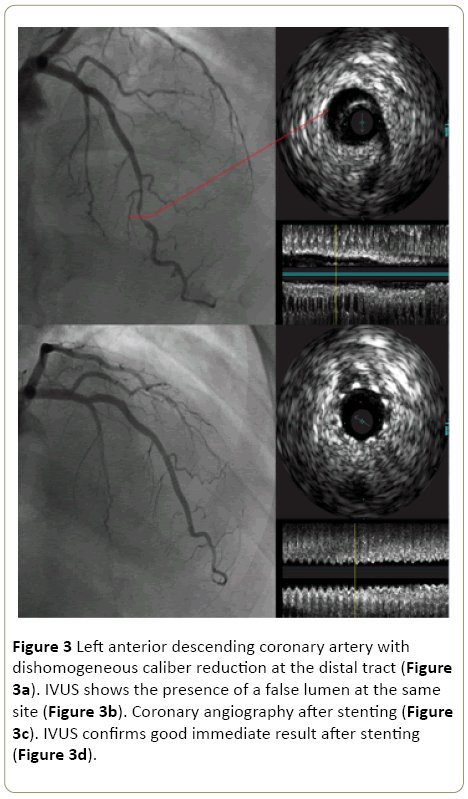
Figure 3: Left anterior descending coronary artery with dishomogeneous caliber reduction at the distal tract (Figure 3a). IVUS shows the presence of a false lumen at the same site (Figure 3b). Coronary angiography after stenting (Figure 3c). IVUS confirms good immediate result after stenting (Figure 3d).
Non-invasive imaging: Coronary computed tomography angiography (CCTA) is the only non-invasive diagnostic exam for coronary arteries evaluation [54,55]. In SCAD setting CCTA may demonstrate the spreading of contrast within the false lumen, coronary stenosis, and presence of IMH. However, in consideration of the low diagnostic power of this test in evaluating distal and small-caliber coronary arteries (diameter <2.5 mm) and of the high prevalence of SCAD in this type of vessels, often occurring without extraluminal contrast spreading, the diagnostic usefulness of CCTA in SCAD setting appears limited. For this reason, CCTA is not recommended as first-choice examination in patients with SCAD; conversely CCTA may be useful in the non-invasive follow-up of patients with proximal-to-middle tracts SCAD, as recently demonstrated by Roura [56,57].
Treatment
Randomized trials comparing different treatment strategies have not been carried out and the optimal treatment of SCAD is still uncertain. In general, the first-line approach consists of a conservative medical therapy [1]. This widespread opinion depends on the evidence that angiographic healing occurs in the majority of cases, varying from 73% to 90% and reaching 100% if the control angiography is performed 26 days after SCAD onset [42,58].
The preference for medical therapy is also motivated by the low procedural success rate and long-term results of both percutaneous coronary intervention (PCI) and cardiac artery bypass grafting (CABG) [11]. The need for revascularization is driven by angiographic and clinical aspects: in case of ongoing myocardial ischemia, persistent ST elevation, hemodynamic instability, complicated ventricular arrhythmias, an invasive approach is advocated, particularly when left main or the proximal tracts of the major coronary arteries are involved [1]. On the basis of observational studies only 17% to 20% of patients with a definite diagnosis of SCAD are treated invasively, including the 3.5% to 10% of patients initially treated conservatively and subsequently undergoing an invasive in-hospital revascularization for recurrent ischemia [41,58,59].
Medical therapy: As stated above there is no full consensus about medical therapy and current recommendations derive from observational studies, cause therapy for ACS (SCAD most frequent presentation) has not been specifically tested in the subset of patients with SCAD [19,56].
Despite the lack of evidence, beta-blockers (BBs) are considered a cornerstone of medical treatment. Similarly, to aortic dissection, BBs could lessen the risk of propagation of the dissection by reducing systemic arterial pressure and heart rate; several studies have indeed demonstrated that BBs reduce arterial shear stress. Moreover, BBs reduce myocardial oxygen consumption, exert an important anti-arrhythmic action and are known to be associated to a significant reduction in mortality in the setting of AMI [60].
A recent observational study in the specific setting of SCAD patients has suggested that BBs is associated with a significant reduction of recurrent AMI [61].
Though in absence of data, antiplatelet therapy is commonly used for management of SCAD: the rationale for single or dual antiplatelet therapy is the risk of thrombosis of the compressed true lumen; on the other hand, antiplatelet therapy increases the bleeding risk and could theoretically determine the expansion of the IMH and extension of the dissection [56,62]. Aspirin is commonly used, while clopidogrel seems to be the preferred choice when a dual antiplatelet therapy (DAPT) regimen is chosen [61]. The duration of DAPT usually varies from 1 month to 1 year [56]. The role of ticagrelor and prasugrel has not been evaluated and is probably restrained to the cases of stent implantation [1]. There are no data supporting the use of glycoprotein IIb/IIIa inhibitors.
Anticoagulant therapy is mandatory in the setting of ACS but the clinical benefit in SCAD is uncertain; similarly, to antiplatelet agents, the positive anti-thrombotic effect is antagonized by the risk of propagation of the IMH so that the majority of evidences discourage heparin continuation once SCAD diagnosis is assessed [19].
Thrombolysis is potentially harmful because of a significant risk of extension of IMH and has to be avoided when clinical and anamnestic data suggest a SCAD [63]. In a retrospective study Shamloo pointed out as, among 87 patients with SCAD treated with thrombolysis, about 60% required a subsequent urgent revascularization [64].
The use of calcium channel blockers (CCB) and nitrates could be beneficial in alleviating symptoms related to a concomitant coronary spasm, but could contribute to increase the arterial wall stress; the use of CCB has been also recently associated to a higher recurrence of myocardial infarction at long term follow-up in patients admitted for SCAD [32,61].
The role of statins in the setting of SCAD is poorly evaluated and controversial. A small retrospective study pointed out safety concerns in a higher SCAD recurrence associated with the use of statins. This finding has not been confirmed by subsequent evidences and a small ongoing randomized study (SAFER-SCAD) is currently investigating the hypotheses of beneficial effects of statins and angiotensin-converting enzyme inhibitors in SCAD [11,36,65].
Percutaneous coronary intervention: In the setting of SCAD, the rate of procedural success of PCI is low: in a large retrospective analysis of 189 patients presented with SCAD a 53% of technical failure of PCI was reported and 13% of patients initially treated with PCI underwent an emergent CABG [58]. In this cohort, PCI failed to protect against repeated revascularization or recurrent SCAD. On the basis of, these findings, a conservative approach and a prolonged observation is currently recommended [58].
In a prospective observational study, Saw described a 64% procedural success rate for PCI; among the patients facing unsuccessful PCI 57% had extension of SCAD, 6% definite stent thrombosis, and 12% underwent urgent CABG [42].
Lettieri described a more encouraging PCI success rate of 73%, but also in this series the conservative approach was characterized by a lower rate of in-hospital cardiac adverse events, when compared to the invasive strategy; moreover 9% of PCI patients required an urgent CABG and 5% of them experienced a stent thrombosis [33].
The poor results of PCI recognize several reasons that make the setting of SCAD nowadays still challenging.
Firstly, in most cases a predisposing pathology of arterial wall tissues is present and can favor a iatrogenic coronary dissection during intracoronary devices maneuvering; in a recent report a 3.4% rate of catheter-induced dissection was observed in patients with SCAD who underwent coronary angiography [66].
Coronary wiring is probably the most crucial procedural threat: the guide wire may fail to enter the true lumen and the false lumen engagement can potentially extend the dissection and worsening the arterial flow; the collateral vessels wiring distally to the stenosis probably represents the only “trick” to confirm the correct position of the guidewire.
The choice of stent dimension could represent a further issue; interventional cardiologists usually prefer long and/or overlapped stents to be sure to cover the whole dissected segment, but this strategy predisposes to stent thrombosis and restenosis. The device diameter choice may also be problematic, as the real arterial caliber, especially in case of type 2 and 3 SCAD, could be difficult to perceived at angiography. Nevertheless, an optimal sizing of stent diameter is crucial because after IMH reabsorption an undersized stent strongly favors late or very late malapposition and the related increased risk of stent thrombosis [67]. Intravascular imaging could be in this scenario extremely helpful though the use of IVUS and OCT, as described before, is potentially harmful and a routine utilization is currently not recommended [48].
Other reasons for high PCI failure rate are the prevalent involvement of distal coronary segments and the more tortuous pathway of coronary arteries in patients with SCAD, as compared with non-SCAD patients [41,68]. Distal sites and tortuosity are well-known unfavorable factors during PCI because of higher risk of arterial wall damage and the difficulties to reach the target segments with stents or balloons [42].
In the last years, several strategies and tricks have been proposed to reduce PCI complications and improve long-term results (Table 1); for example, unlike general ACS recommendations, the femoral access should be preferred, even though associated with an increased bleeding risk, because the rate of radial access site failure is significantly higher in patients with SCAD [42,66]. In order to avoid IMH extension and eventual stent malapposition, many authors suggest to carefully assess the length of dissected segment and the true caliber of the vessel with intravascular imaging support (OCT or IVUS) [67].
| Tendency to vascular access artery dissection |
Femoral approach |
| Catheter-induced coronary dissection |
Careful manipulation of guide catheter |
| Wiring the false lumen |
Check for collateral vessel engagement |
| Risk of extension of IMH |
Length of stent exceeding 5 mm to 10 mm the dissection |
| Multiple stents |
| SES |
| DEB |
| Risk of late/very late malapposition |
Adequate stent diameter selection (IVUS, OCT) |
| BRS |
| SES |
| OCT/IVUS confirmation of good immediate apposition |
| Continuing DAPT to prevent stent thrombosis |
BRS: Bio-resorbable scaffold; DAPT: Dual antiplatelet therapy; DEB: drug eluting balloons; IMH:Intramural hematoma; IVUS: Intravascular ultrasound; OCT: Optical Coherence Tomography; SES: Self-expandable stent
Table 1: Percutaneous interventions in SCAD: issues and corresponding helpful strategies.
To adequately cover the edges of IMH, the stent borders should exceed by 5-10 mm the dissection edges. In case multiple stents are needed, it is preferable to start covering the two edges of the dissection (the distal first) and to finally implant a third overlapped stent in the mid-segment; this approach reduces the risk of a “squeezing-induced” propagation of IMH [1]. An alternative and “more minimalist” procedure consists in stenting only the intimal tear [67].
As regards device selection in PCI, drug eluting stents (DES) have dramatically improved patients outcome; despite in ACS treatment DES are considered the standard of care, no data are available in the specific setting of SCAD. The main issues of DES are the risk of late malapposition after IMH reabsorption and the theoretical harm for IMH propagation if accurate sizing of the dissected segment is lacking [19].
Bio-resorbable scaffolds (BRS) are recently introduced devices for percutaneous treatment of coronary artery disease; BRS provide a temporary support to the arterial wall, release an anti-proliferative drug to limit the inflammatory reaction and the restenosis phenomenon, and allow vessel healing and its physiological function restoration. BRS probably represent the most revolutionary approach of the last two decades, born to overcome the limitations of DES, especially the long-term risk of neo-atherosclerosis [69]. In the setting of SCAD, BRS would eliminate the issue related to late or very late malapposition after IMH reabsorption because the scaffold completely reabsorbs. Moreover, the complete long-term anatomical and functional healing is a further major advantage as SCAD usually affect young patients. It has been reported the successful use of BRS for treatment of SCAD even for treatment of very long dissected segments [70-72].
However, the use of BRS presents nonetheless some limitations: Procedural success and long-term results strictly depend on an accurate evaluation of the coronary lesion based on the systematic use of IVUS or OCT to determine length of the SCAD and caliber of the vessel, but also to check the correct expansion and apposition of the scaffold after deployment [73]. The risk of early thrombosis after BRS implantation is strongly related to insufficient lesion preparation and post-dilatation, nevertheless the routinely use of intravascular imaging techniques is conversely known to be harmful [1,74]. In the setting of SCAD it is often necessary to stent long coronary segments and overlap 2 or more BRS with a consequent additional theoretical risk of thrombosis and restenosis [75]. Furthermore, BRS should be avoided when the vessel diameter is less than 2.5 mm because of an increased risk of device thrombosis [76] and we know that, mostly in young female patients, SCAD affects mid-distal segments; another limit is the frequent coronary tortuosity that could challenge BRS deliverability, because of higher profile and worse trackability of BRS when compared to conventional stents.
The use of cutting balloon for treatment of SCAD is even less evaluated and is limited to case reports [77]. The rationale of the use of cutting balloon is the attempt to reduce the pressure of false lumen by fenestrating the IMH, avoiding propagation of dissection and facilitating the healing. However, the use of cutting balloon is associated to the risk of coronary rupture, especially in SCAD patients who have high probability of arterial wall disease [1,77].
A recent Italian registry suggests the intriguing possibility to avoid any stent or scaffold implantation and to achieve a TIMI 3 flow using drug eluting balloons, allowing a spontaneous delayed healing [78]. In contrast with this hypothesis, there is a concrete risk of extension of IMH for the increase of pressure in the false lumen during balloon inflation. Moreover, even if coronary arteries in SCAD patients are often not atherosclerotic, an acute recoil cannot be ruled out.
The use of sirolimus self-expandable stent (SES) has been also proposed [79]. The theoretical advantage of SES, known that post-dilation is not required, is driven by its ability to adapt softly to the arterial wall, avoiding the risk of IMH propagation and minimizing struts malapposition due to underestimation of vessel caliber.
Coronary artery bypass graft (CABG): Emergent CABG is an option after PCI failure, or when coronary anatomy is not favourable to PCI or if left main is involved. Procedural success is high because of the relatively young age of patients, the usual absence of comorbidity and of coronary atherosclerosis and calcification. In a small cohort of patients Tweet et al. observed only a 6% unsuccessful grafting in the setting of SCAD [58]. The long-term results are less encouraging, as at a median 3.5 years follow-up a consistent part of grafts were closed and CABG did not demonstrate to protect against recurrent SCAD or target vessel revascularization [58]. In general, CABG should be considered an invasive alternative to restore coronary flow in urgent/emergent settings when PCI is not feasible or fails. The poor long-term patency of grafts can be clinical silent and prognostically irrelevant because of the extremely frequent spontaneous healing of SCAD and it is also allowed to assume that the latter could also favor grafts occlusion itself.
Conclusions
Diagnostic and therapeutic approach to SCAD remains nowadays challenging. SCAD presents a unique pathophysiology that deeply differs from atherosclerotic plaques; the latter conversely represent the most frequent cause of both ACSs and stable coronary disease and thus the best studied setting. Nevertheless, the latest diagnostic innovations, such as intravascular imaging systems, currently provide an extremely helpful support to coronary angiography in order to reach a definite diagnosis. Medical-conservative treatment still represents the first line approach, nevertheless the beneficial effects of the two cornerstone therapies of atherosclerotic coronary arteries disease, antiplatelet and antithrombotic drugs, are still controversial.
In the last years, innovative devices and techniques succeeded in improving the firstly disappointing procedural success and long-term results of PCI; randomized studies and dedicated multicenter registries are anyway advocated to define a standardized approach for both diagnostic and therapeutic strategies.
References
- Saw J, Mancini GB, Humphries KH (2016) Contemporary review on spontaneous coronary artery dissection. J Am Coll Cardiol 68: 297-312.
- Pretty HC (1931) Dissecting aneurysm of coronary artery in a woman aged 42. BMJ i: 667.
- Mortensen KH, Thuesen L, Kristensen IB, Christiansen EH (2009) Spontaneous coronary artery dissection: A Western Denmark Heart Registry study. Catheter Cardiovasc Interv 74: 710-717.
- Hering D, Piper C, Hohmann C, Schultheiss HP, Horstkotte D (1998) Prospective study of the incidence, pathogenesis and therapy of spontaneous, by coronary angiography diagnosed coronary artery dissection. Z Kardiol 87: 961-970.
- Rashid HN, Wong DT, Wijesekera H, Gutman SJ, Shanmugam VB, et al. (2016) Incidence and characterisation of spontaneous coronary artery dissection as a cause of acute coronary syndrome: A single-centre Australian experience. Int J Cardiol 202: 336-338.
- Nishiguchi T, Tanaka A, Ozaki Y, Taruya A, Fukuda S, et al. (2016) Prevalence of spontaneous coronary artery dissection in patients with acute coronary syndrome. Eur Heart J Acute Cardiovasc Care 5: 263-270.
- Vanzetto G, Berger Coz E, Barone-Rochette G, Chavanon O, Bouvaist H, et al. (2009) Prevalence, therapeutic management and medium-term prognosis of spontaneous coronary artery dissection: results from a database of 11.605 patients. Eur J Cardiothorac Surg 35: 250-254.
- Saw J, Aymong E, Mancini GBJ, Sedlak T, Starovoytov A, et al. (2014) Non-atherosclerotic coronary artery disease in young women. Can J Cardiol 30: 814-819.
- Nakashima T, Noguchi T, Haruta S, Yamamoto Y, Oshima S, et al. (2016) Prognostic impact of spontaneous coronary artery dissection in young female patients with acute myocardial infarction: A report from the angina pectoris-myocardial infarction multicenter investigators in Japan. Int J Cardiol 207: 341-348.
- Elkayam U, Jalnapurkar S, Barakkat MN, Khatri N, Kealey AJ, et al. (2014) Pregnancy-associated acute myocardial infarction: A review of contemporary experience in 150 cases between 2006 and 2011. Circulation 129: 1695-1702.
- Rogowski S, Maeder MT, Weilenmann D, Haager PK, Ammann P, et al. (2015) Spontaneous coronary artery dissection: Angiographic follow-up and long-term clinical outcome in a predominantly medically treated population. Catheter Cardiovasc Interv.
- Maehara A, Mintz GS, Castagna MT, Pichard AD, Satler LF, et al. (2002) Intravascular ultrasound assessment of spontaneous coronary artery dissection. Am J Cardiol 89: 466-468.
- Tokura M, Taguchi I, Kageyama M, Nasuno T, Nishiyama Y, et al. (2014) Clinical features of spontaneous coronary artery dissection. J Cardiol 63: 119-122.
- Saw J, Poulter R, Fung A, Wood D, Hamburger J, et al. (2012) Spontaneous coronary artery dissection in patients with fibromuscular dysplasia: A case series. Circ Cardiovasc Interv 5: 134-137.
- Saw J, Ricci D, Starovoytov A, Fox R, Buller CE (2013) Spontaneous coronary artery dissection: Prevalence of predisposing conditions including fibromuscular dysplasia in a tertiary center cohort. J Am Coll Cardiol Intv 6: 44-52.
- Prasad M, Tweet MS, Hayes SN, Leng S, Liang JJ, et al. (2015) Prevalence of extracoronary vascular abnormalities and fibromuscular dysplasia in patients with spontaneous coronary artery dissection. Am J Cardiol 115: 1672-1677.
- Vijayaraghavan R, Verma S, Gupta N, Saw J (2014) Pregnancy-related spontaneous coronary artery dissection. Circulation 130:1915-1920.
- Manalo-Estrella P, Barker AE (1967) Histopathologic findings in human aortic media associated with pregnancy. Archiv Pathol 83:336-341.
- Yip A, Saw J (2015) Spontaneous coronary artery dissection:A review. Cardiovasc Diagn Ther 5: 37-48.
- Sheikh AS, O’Sullivan M (2012) Pregnancy-related spontaneous coronary artery dissection: Two case reports and a comprehensive review of literature. Heart Views 13: 53-65.
- Evangelou D, Letsas KP, Korantzopoulos P, Antonellis I, Sioras E, et al. (2006) Spontaneous coronary artery dissection associated with oral contraceptive use: A case report and review of the literature. Int J Cardiol 112: 380-382.
- Koller PT, Cliffe CM, Ridley DJ (1998) Immunosuppressive therapy for peripartum-type spontaneous coronary artery dissection: Case report and review. Clin Cardiol 21: 40-46.
- Kamran M, Guptan A, Bogal M (2008) Spontaneous coronary artery dissection: Case series and review. J Invasive Cardiol 20: 553-559.
- Chu KH, Menapace FJ, Blankenship JC, Hausch R, Harrington T (1998). Polyarteritis nodosa presenting as acute myocardial infarction with coronary dissection. Cathet Cardiovasc Diagn 44: 320-324.
- Hampole C, Philip F, Shafii A, Pettersson G, Anesi GL, et al. (2011) Spontaneous coronary artery dissection in Ehlers-Danlos syndrome. Ann Thorac Surg 92: 1883-1884.
- Aldoboni AH, Hamza EA, Majdi K, Ngibzadhe M, Palasaidi S, et al. (2002) Spontaneous dissection of coronary artery treated by primary stenting as the first presentation of systemic lupus erythematosus. J Invasive Cardiol 14: 694-696.
- Yiangou K, Papadopoulos K, Azina C (2016) Heavy lifting causing spontaneous coronary artery dissection with anterior myocardial infarction in a 54-Year-old woman. Tex Heart Inst J 43: 189-191.
- Lempereur M, Grewal J, Saw J (2014) Spontaneous coronary artery dissection associated with b-HCG injections and fibromuscular dysplasia. Can J Cardiol 30: 464.
- Sivam S, Yozghatlian V, Dentice R, McGrady M, Moriarty C, et al. (2014) Spontaneous coronary artery dissection associated with coughing. J Cyst Fibros 13: 235-237.
- Keir ML, Dehghani P (2016) Corticosteroids and spontaneous coronary artery dissection: A new predisposing factor?. Can J Cardiol 32: 395.
- El-Sherief K, Rashidan A, Srikanth S (2011) Spontaneous coronary artery dissection after intense weightlifting: UCSF Fresno department of cardiology. Catheter Cardiovasc Interv 78: 223-227.
- Al Emam AR, Almomani A, Gilani SA, Khalife WI (2016) Spontaneous coronary artery dissection: One disease, variable presentations, and different management approaches. Int J Angiol 25: 139-147.
- Lettieri C, Zavalloni D, Rossini R, Morici N, Ettori F, et al. (2015) Management and long-term prognosis of spontaneous coronary artery dissection. Am J Cardiol 116: 66-73.
- Hill SF, Sheppard MN (2010) Non-atherosclerotic coronary artery disease associated with sudden cardiac death. Heart 96: 1119-1125.
- Lindor RA, Tweet MS, Goyal KA, Lohse CM, Gulati R, et al. (2016) Emergency department presentation of patients with spontaneous coronary artery dissection. J Emerg Med.
- Tweet MS, Hayes SN, Pitta SR, Simari RD, Lerman A, et al. (2012) Clinical features, management and prognosis of spontaneous coronary artery dissection. Circulation 126: 579-588.
- Giacoppo D, Capodanno D, Dangas G, Tamburino C (2014) Spontaneous coronary artery dissection. Int J Cardiol 175: 8-20.
- Alfonso F, Bastante T, Cuesta J, Rodríguez D, Benedicto A, et al. (2015) Spontaneous coronary artery dissection: Novel insights on diagnosis and management. Cardiovasc Diagn Ther 5: 133-140.
- Vrints CJ (2010) Spontaneous coronary artery dissection. Heart 96: 801-808.
- Rogers JH, Lasala JM (2004) Coronary artery dissection and perforation complicating percutaneous coronary intervention. J Invasive Cardiol 16: 493-499.
- Saw J (2014) Coronary angiogram classification of spontaneous coronary artery dissection. Catheter Cardiovasc Interv 84: 1115-1122.
- Saw J, Aymong E, Sedlak T, Buller CE, Starovoytov A, et al. (2014) Spontaneous coronary artery dissection: Association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv 7: 645-655.
- Virmani R, Forman MB, Rabinowitz M, McAllister Jr HA (1984) Coronary artery dissections. Cardiol Clin 4: 633-646.
- Verma PK, Sandhu MS, Mittal BR, Aggarwal N, Kumar A, et al. (2004) Large spontaneous coronary artery dissections: A study of three cases, literature review, and possible therapeutic strategies. Angiology 55: 309-318.
- Jorgensen MB, Aharonian V, Mansukhani P, Mahrer PR (1994) Spontaneous coronary dissection: A cluster of cases with this rare finding. Am Heart J 127: 1382-1387.
- Kearney P, Singh H, Hutter J, Khan S, Lee G, et al. (1993) Spontaneous coronary artery dissection: A report of three cases and review of the literature. Postgrad Med J 69: 940-945.
- Buccheri D, Piraino D, Cortese B (2016) Spontaneous coronary artery dissection: A hint into its diagnosis and therapy. Int J Cardiol 215: 545.
- Mahmood MM, Austin D (2016) IVUS and OCT guided primary percutaneous coronary intervention for spontaneous coronary artery dissection with bioresorbable vascular scaffolds. Cardiovasc Revasc Med.
- Paulo M, Sandoval J, Lennie V, Dutary J, Medina M, et al. (2013) Combined use of OCT and IVUS in spontaneous coronary artery dissection. JACC Cardiovasc Imaging 6: 830-832.
- Sengottuvelu G, Rajendran R, Majumdar D (2014) Optical coherence tomogram of spontaneous coronary artery dissection managed with drug eluting stent. Indian Heart J 66: 247-248.
- Alfonso F, Paulo M, Gonzalo N, Dutary J, Jimenez-Quevedo P, et al. (2012) Diagnosis of spontaneous coronary artery dissection by optical coherence tomography. J Am Coll Cardiol 59: 1073-1079.
- Johnson PM, Patel J, Yeung M, Kaul P (2014) Intra-coronary imaging modalities. Curr Treat Options Cardiovasc Med 16: 304.
- Buccheri D, Piraino D, Cortese B (2016) Intravascular imaging as a tool for definite diagnosis of acute coronary syndrome caused by spontaneous coronary artery dissection. Int J Cardiol 214: 43-45.
- Russo V, Marrozzini C, Zompatori M (2013) Spontaneous coronary artery dissection: Role of coronary CT angiography. Heart 99: 672-673.
- Tweet MS, Gulati R, Hayes SN (2016) Spontaneous coronary artery dissection. Curr Cardiol Rep 18: 60.
- Saw J (2013) Spontaneous coronary artery dissection. Can J Cardiol 29: 1027-1033.
- Roura G, Ariza-Solé A, Rodriguez-Caballero IF, Gomez-Lara J, Ferreiro JL, et al. (2016). Noninvasive follow-up of patients with spontaneous coronary artery dissection with CT angiography. JACC Cardiovasc Imaging 9: 896-897.
- Tweet MS, Eleid MF, Best PJ, Lennon RJ, Lerman A, et al. (2014) Spontaneous coronary artery dissection: Revascularization versus conservative therapy. Circ Cardiovasc Interv 7: 777-786.
- Saw J, Prakash R, Starovoytov A, Aymong E, Sedlak T, et al. (2016) Cardiovascular outcomes in a large prospectively followed single-center cohort of spontaneous coronary artery dissection patients. J Am Coll Cardiol 67: 457.
- Li JZ, Eagle KA, Vaishnava P (2013) Hypertensive and acute aortic syndromes. Cardiol Clin 31: 493-501.
- Eng LK, Starovoytov A, Humphries K, Mancini J, Saw J (2016) Medical therapy and clinical out-comes with spontaneous coronary artery dissection. J Am Coll Cardiol 68: B20.
- Choi JW, Davidson CJ (2002) Spontaneous multivessel coronary artery dissection in a long-distance runner successfully treated with oral antiplatelet therapy. J Invasive Cardiol 14: 675.
- Zupan I, Noc M, Trinkaus D, Popovic M (2001) Double vessel extension of spontaneous left main coronary artery dissection in young women treated with thrombolytics. Catheter Cardiovasc Interv 52: 226-230.
- Shamloo BK, Chintala RS, Nasur A, Ghazvini M, Shariat P, et al. (2010) Spontaneous coronary artery dissection: Aggressive vs. conservative therapy. J Invasive Cardiol 22: 222-228.
- https://clinicaltrials.gov/ct2/show/NCT02008786
- Prakash R, Starovoytov A, Heydari M, Mancini GB, Saw J (2016) Catheter-induced iatrogenic coronary artery dissection in patients with spontaneous coronary artery dissection. JACC Cardiovasc Interv 9: 1851-1853.
- Lempereur M, Fung A, Saw J (2015) Stent malapposition with resorption of intramural hematoma with spontaneous coronary artery dissection. Cardiovasc Diagn Ther 5: 323-329.
- Eleid MF, Guddeti RR, Tweet MS, Lerman A, Singh M, et al. (2014) Coronary artery tortuosity in spontaneous coronary artery dissection: Angiographic characteristics and clinical implications. Circ Cardiovasc Interv 7: 656-662.
- Tenekecioglu E, Farooq V, Bourantas CV, Silva RC, Onuma Y, et al. (2016) Bioresorbable scaffolds: A new paradigm in percutaneous coronary intervention. BMC Cardiovasc Disord 16: 38.
- Cockburn J, Yan W, Bhindi R, Hansen P (2014) Spontaneous coronary artery dissection treated with bioresorbable vascular scaffolds guided by optical coherence tomography. Can J Cardiol 30: 1461.
- Sengottuvelu G, Rajendran R (2014) Full polymer jacketing for long-segment spontaneous coronary artery dissection using bioresorbable vascular scaffolds. JACC Cardiovasc Interv 7: 820-821.
- Sengottuvelu G, Rajendran R, Majumdar D (2015) Capping spontaneous coronary artery dissection with overlapping bioabsorbable scaffolds. Heart Lung Circ 24: e39-40.
- Karanasos A, Simsek C, Gnanadesigan M, van Ditzhuijzen NS, Freire R, et al. (2014) OCT assessment of the long-term vascular healing response 5 years after everolimus-eluting bioresorbable vascular scaffold. J Am Coll Cardiol 64: 2343-2356.
- Lipinski MJ, Escarcega RO, Baker NC, Benn HA, Gaglia MA Jr, et al. (2016) Scaffold thrombosis after percutaneous coronary intervention with ABSORB bioresorbable vascular scaffold: A systematic review and meta-analysis. JACC Cardiovasc Interv 9: 12-24.
- Karim Galougahi K, Ben-Yehuda O, Maehara A, Mintz GS, Stone GW, et al. (2016) "The scaffolding must be removed once the house is built"-spontaneous coronary artery dissection and the potential of bioresorbable scaffolds. J Thorac Dis 8: E1398-E1403.
- Stone GW, Granada JF (2015) Very late thrombosis after bioresorbable scaffolds: Cause for concern? J Am Coll Cardiol 66: 1915-1917.
- Ito T, Shintani Y, Ichihashi T, Fujita H, Ohte N (2016) Non-atherosclerotic spontaneous coronary artery dissection revascularized by intravascular ultrasonography-guided fenestration with cutting balloon angioplasty. Cardiovasc Interv Ther.
- Cortese B, Silva Orrego P, Agostoni P, Buccheri D, Piraino D, et al. (2015) Effect of drug-coated balloons in native coronary artery disease left with a dissection. JACC Cardiovasc Interv 8: 2003-2009.
- Mele M, Langialonga T, Maggi A, Villella M, Villella A (2016) Self-expanding stent for spontaneous coronary artery dissection: A rational choice. J Cardiovasc Med (Hagerstown).