- (2011) Volume 12, Issue 2
Hasan Gucer1*, Pelin Bagci1, Esra Zeynep Coskunoglu2, Cetin Karadag3
1Department of Pathology, Rize University Medical School. Rize, Turkey
2Department of Pathology, Rize Education and Research Hospital. Rize, Turkey
3Department of General Surgery, Unye State Hospital. Ordu, Turkey
Received December 31st, 2010 Accepted January 5th, 2011
Context Heterotopia of the pancreas can be defined as the presence of pancreatic tissue in an abnormal location without any continuity with the main body of the pancreas. Heterotopic pancreatic tissue located in the gallbladder is a rare entity. Despite being a congenital condition, it takes years for heterotopic pancreas to become symptomatic. Case report An 80-year-old male patient presented to our hospital with a two-week history of abdominal pain, nausea and vomiting aggravated after meals. Abdominal ultrasonography revealed minimal wall edema and small grain-sized gallstones in the gallbladder. The patient was hospitalized and laparoscopic cholecystectomy was performed for acute cholecystitis. Pathologic examination showed a 6 mm nodular mass of pancreatic tissue in the gallbladder wall, comprised mainly of ductal and acinic structures and a few endocrine cells. Conclusion We found this case of pancreatic heterotopia worth reporting because of its rare incidence.
Choristoma; Gallbladder; Pancreas
Heterotopia of the pancreas, also called pancreatic choristoma, is defined as pancreatic tissue in an abnormal location without any vascular, neuronal or anatomical continuity with the main body of the pancreas [1]. Heterotopic pancreas tissue is commonly found in the stomach, duodenum, proximal jejunum and Meckel’s diverticulum, but is rarely seen in the ileum, gallbladder, bile ducts, splenic hilum, umbilicus and liver [2, 3, 4].
In this report, we present a case of heterotopic pancreas located in the gallbladder with clinical findings of acute cholecystitis.
An eighty-year-old male presented to the Department of General Surgery with nausea, vomiting, abdominal distension and abdominal pain of 2 months duration which was aggravated after meals. On physical examination, the right upper abdomen was tender with a positive Murphy’s sign, but there was no defense or rebound. Abdominal ultrasound revealed biliary sludge in the lumen of the gallbladder and minimal wall edema. His laboratory data revealed a total bilirubin of 4 mg/dL (reference range: 0.2-1.2 mg/dL), a direct bilirubin of 3.5 mg/dL (reference range: 0-0.5 mg/dL), alkaline phosphatase equal to 425 U/L (reference range: 40-150 U/L), AST equal to 389 U/L (reference range: 5-34 U/L), ALT equal to 489 U/L (reference range: 0-55 U/L), GGT equal to 682 U/L (reference range: 9-64 U/L) and amylase equal to 166 U/L (reference range: 25-125 U/L). Laparoscopic cholecystectomy was carried out with a preoperative diagnosis of acute cholecystitis.
At macroscopic examination, the gallbladder was 25 g in weight and 7.5x5.5x0.3 cm in diameter. A 6 mm, solid intramural nodule was seen at the corpus. The cut section of the nodule was straw-colored, hard and had focal hemorrhagic areas (Figure 1). Thick biliary sludge was seen in the lumen, but there were no stones. Microscopic examination revealed aberrant pancreatic tissue consisting of acini, intra and interlobular ducts and some chromogranin A and few synaptophysin expressing islet cells (Figures 2, 3, and 4). No direct connection with the gallbladder lumen was observed. A chronic inflammatory reaction with some eosinophils was also seen at subepithelial areas.
All symptoms disappeared following cholecystectomy and the patient recovered completely.
As stated by Beltran and Barria [1], Schultz first described heterotopic pancreas in 1727 and Klob reported the first histopathological confirmation of heterotopic pancreas in 1859 [5]. About 30 cases of heterotopic pancreas in the gallbladder have been reported worldwide in a review of the literature up to the present [6].
The reported incidence of heterotopic pancreas in the gastrointestinal tract ranged from 0.55% to 13.7% in autoptic series, and 0.2% in laparotomy [2, 7, 8]. Heterotopic pancreas can affect all ages, and men are usually affected three times more than women [6]. However, there is a higher incidence of female patients in heterotopic pancreas of the gallbladder cases [8]. In our case, the patient was a male.
The majority of cases are asymptomatic; but it can be associated with obstruction of the bile duct, cholelithiasis, acute or chronic pancreatitis, hyperinsulinism, intussusception and gastrointestinal hemorrhage. In addition, heterotopic pancreatic tissue is prone to different pathologic changes, such as cyst or abscess formation, acute pancreatitis and calcification [1, 2, 3, 6, 7, 8]. In our case, the ectopic tissue caused chronic cholecystitis. Most cases of pancreatic heterotopia have biologically benign behavior; however, only a few reports have described benign and malignant neoplastic changes [9, 10]. There were no metaplastic or neoplastic changes in our case.
Preoperative diagnosis is rarely possible because it is a very uncommon pathologic entity and is therefore not considered in the differential diagnosis, either clinically or radiologically [11].
Macroscopically, these lesions are usually detected incidentally as well-circumscribed, firm, round, single, yellow nodules. Their size can vary from several millimeters to centimeters [1, 2, 3, 6, 7, 8]. Fifty percent of heterotopic pancreatic tissue found in the gallbladder is located in the neck [7]. The lesion was located at the corpus in our case. It can be located in the submucosa, muscularis propria or subserosa [1, 2, 3, 6, 7, 8].
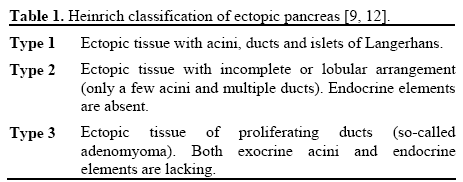
Microscopically, ectopic pancreas has been classified into three types by von Heinrich (Table 1) [9, 12]. Our case was considered to be a type 1 ectopic pancreas, based on Heinrich classification.
The origin of heterotopic pancreatic tissue is controversial but two theories have been proposed. The most widely accepted theory is that heterotopic pancreas is formed from a lateral budding of the rudimentary pancreatic duct while penetrating the intestinal wall and is carried by the longitudinal growth of the intestines. The other theory suggests that the pancreatic tissue is separated from the main pancreas during embryonic rotation [7, 8]. A recent theory states that abnormalities in the notch signaling system during embryogenesis may contribute to heterotopic pancreatic tissue in the gallbladder [7].
Heterotopic pancreas located in the gallbladder wall is an uncommon lesion which is most often detected incidentally and may be associated with gallbladder symptomatology. Although not proven, this rare condition may have the potential of developing into a malignancy.
We found this case of pancreatic heterotopia worth reporting because of its rarity and its association with cholecystitis symptomatology.
The authors have no potential conflicts of interest