Research Paper - (2009) Volume 17, Issue 5
Research Assistant, Department of Family Medicine, University of Medical Sciences, Poznan, Poland
Dirk Avonts MD PhD
Professor, Centre for General Practice, University of Antwerp, Belgium
Wanda Horst-Sikorska MD PhD
Professor, Head of Department, Department of Family Medicine, University of Medical Sciences, Poznan, Poland
Magdalena Ignaszak-Szczepaniak MD PhD
Research Assistant, Department of Family Medicine, University of Medical Sciences, Poznan, Poland
Michal Michalak
Master of Science, Research Assistant, Department of Computer Science and Statistics, University of Medical Sciences, Poznan, Poland
Received date: 17 May 2009; Accepted date: 30 August 2009
Objective General practitioners’ (GPs’) time and resources for preventive services needs to be delivered equitably. We aimed to study the effect of patients’ gender on the delivery of preventive procedures to adult patients aged 40 years and over. Method An observational study was performed in primary care surgeries in Wielkopolska (Poland) as a part of the Improving Quality in Primary Care (PIUPOZ) programme carried out by Family Medicine Department of the University of Medical Sciences, Poznan. Trained observers directly observed GPs in their office, to register preventive procedures performed during the consultation and in the previous year (via the medical record) in patients aged 40 years and over. Results A total of 1073 preventive procedures were registered among 450 patients (267 women and 183 men) by 113 doctors in one year. The most common were serum glucose, blood pressure and total cholesterol measurements. Six procedures were offered to less than 10% of patients: dietary advice, tobacco use and alcohol screening, exercise counselling, body mass index (BMI) recording, and waist measurement. Men were more likely to receive tobacco use and alcohol screening and BMI measurement, while more women were offered a total cholesterol screen. Conclusions The annual delivery rate of preventive procedures in patients aged 40 years and above is below the recommended level set by the Polish Ministry of Health. Procedures based on clinical examinations or laboratory tests were offered and performed more frequently than lifestyle advice. More men than women received preventive services for tobacco use or alcohol screening and BMI measurements. Patients’ gender and physicians’ engagement may influence GPs’ preventive attitude and performance. These elements should be incorporated in the development of guidelines concerning prevention in primary care.
health education, prevention, primary care
Primary prevention includes any intervention designed to reduce the risk of diseases occurring. It aims to promote wellbeing and to prevent the onset of disease by reducing risk factors in the population, either through changes in behaviour and lifestyle, or through changes in the environment supported by appropriate health education and public policies. Secondary pre-vention targets established disease, with the aim of avoiding recurrence or alleviating consequences by early detection and risk factor modification.[1] It is often not easy to evaluate the effectiveness of preven-tive services, especially lifestyle counselling, as part of primary prevention. Maciosek et al performed a systematic assessment of the value of preventive pro-cedures, based on two dimensions: burden of disease prevented by each procedure and cost-effectiveness.[2] The most efficient preventive interventions were screen-ing for tobacco use and alcohol consumption, followed by lipid profile measurement. Counselling about phys-ical activity and healthy diet were less efficient at reducing outcomes.
Although prevention may be effective, it is not as widely used as it should be. The Polish Ministry of Health suggests offering preventive procedures relat-ing to physical activity, alcohol consumption, tobacco use, diet, body weight and blood glucose and lipid measurement, to all patients aged 40 years or over, on an annual basis. Lack of time is one of the most cited barriers towards the delivery of prevention in primary care. A few studies have examined the actual time physicians spend on preventive services. Yarnall et al estimated that counselling and screening could be accomplished in 20 to 30 minutes and it would take 7.8 hours per working day for a physician to deliver recommended preventive services.[3] A discussion around prevention often requires 5 to 10 minutes; an average consultation in primary care lasts 10 minutes.
As a consequence, general practitioners (GPs) have to establish priorities on which preventive interven-tions to deliver and to whom. We were interested, especially for patients aged 40 years and over, in which preventive procedures were offered during routine primary care consultations. Women are more frequent attendees to primary care than men.[4] Do they receive more prevention procedures, compared to men? Is there a difference between the categories of preventive procedures offered to male and female patients?
This study was designed to investigate the effect of patients’ gender on annual delivery of preventive procedures in patients aged 40 years and over.
The study was performed during a baseline audit in surgeries in 2008 as a part of the PIUPOZ programme carried out by the Family Medicine Department of University of Medical Sciences, Poznan, Poland. The acronym PIUPOZ stands for Poprawa Iakosci Uslug w Podstawowej Opiece Zdrowotnej which means ‘im-proving quality in primary care’. The aim of the PIUPOZ is to improve the quality of primary care in Poland by offering training in preventive medicine for GPs. In the PIUPOZ programme, lectures and inter-active workshops were undertaken with groups of 15 people, lasting 25 hours during two weekends. The main topics were prevention, diagnosis and treatment of coronary heart disease (CHD) and chronic obstruc-tive pulmonary disease (COPD), and breast and colon cancer screening. Participation, accommodation and course materials were provided free of charge. After completing the course, participants received a certifi-cate and educational credits. Data presented in this paper were collected prior to participation of phys-icians in the programme.
The study population consisted of all GPs working in the Wielkopolska region recruited to the PIUPOZ programme. Doctors working or training in family medicine or those in internal medicine working in primary care settings were included as GPs invited to take part in the project. Invitations were sent by mail and email. Recruitment to the programme was ex-tended through personal contacts, at medical confer-ences or with the aid of adverts in the medical press. Candidates were registered through the family medi-cine department until the sample size of 120 GPs was achieved. Of the120 doctors who volunteered to partici-pate, 113 were included in the present study; seven were excluded because of subsequent withdrawal.
Observers (two men and two women) were recruited from final-year medical students with an interest in family medicine. They received a four-hour training session on preventive guidelines from a member of the research team. They were also instructed about the study registration form and how to perform an audit regarding confidentiality rules. The observers were exclusively involved in collecting data in the offices (surgeries) of participating GPs. They monitored GPs during consultations and observed each GP for pre-ventive procedures undertaken with four consecutive patients aged 40 years and over. The observers had access to patients’ medical records and recorded, in addition to the observed preventive procedures dur-ing the consultation, all preventive procedures noted in the patient’s medical record during the previous year.
The recording form used by the observers collected information on 11 preventive procedures: screening for tobacco use, alcohol consumption, body weight, body mass index (BMI), waist measurement, physical activity, diet (fat or fruits and vegetables intake), blood pressure, blood glucose and lipid profile. For each procedure, the observer recorded whether it was per-formed (or not) during the observed consultation or recorded in the previous year. The physician identity was not recorded on the study form and the observed doctors did not have access to the forms.
Descriptive statistics were used to characterise the observed patients. The analysis focused on delivery rates of different preventive procedures and the differ-ences between female and male patients. Chi-square tests were used to compare quantitative data. All tests were analysed at the significance level of 0.05, and analyses were performed using STATISTICA v.7.1 (StatSoft Inc, www.statsoft.com).
Study sample
A total of 450 patient consultations and medical records (from 113 GPs) were collected and analysed. For each patient only one consultation was registered. There were 267 (59.3%) women and 183 (40.7%) men observed. The GPs had a similar mixed patient popu-lation of men and women. The proportion of men and women on the patient lists of the doctors was com-parable. All study patients were aged 40 years or over; the mean age was 59.5 (standard deviation (SD) = 11.23): 60.2 years (SD = 11.25) for women and 58.6 years for men (SD = 11.14); P = 0.13.
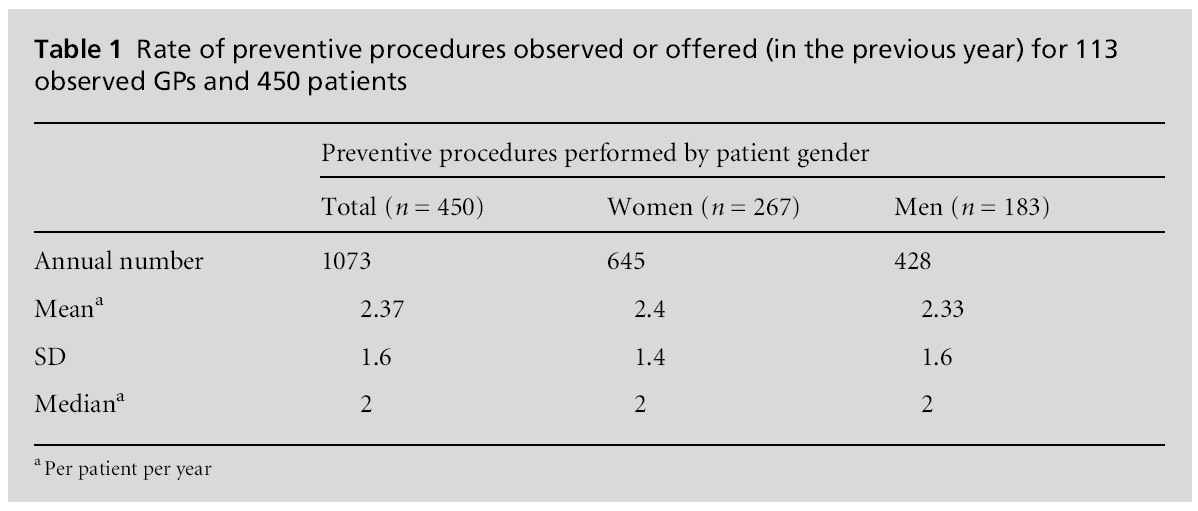
During the observed consultations, 1073 preventive procedures were performed, 645 (60.1%) in women and 428 (39.9%) in men. This difference was not statistically significant. The mean number of pro-cedures per patient was 2.37 (SD = 1.6): 2.4 (SD = 1.4) for women and 2.33 (SD = 1.6) for men. The numbers of procedures performed in women and men are presented in Table 1 and the rates of specific preventive procedures are presented in Table 2. The most frequently recorded procedures were serum glucose in 68.0% of the patients, blood pressure in 58.4% and total cholesterol measurement in 55.6% of the patients. In 81 (18%) patients who received only one preventive procedure at the observed consultation or during the previous year, 35.8% had serum glucose measured and 34.6% had blood pressure checked. A high number of preventive procedures (six out of 11) were offered to less than 10% of patients: dietary, tobacco use and alcohol drinking screening, exercise counselling, BMI and waist measurement.

The correlation between gender and the delivery of preventive procedures is presented in Table 3. There was a statistically significant difference between patients’ gender and some preventive procedures. Men were more likely to receive screening for tobacco use, alcohol consumption, and BMI measurement, whereas women had their blood cholesterol checked more frequently.
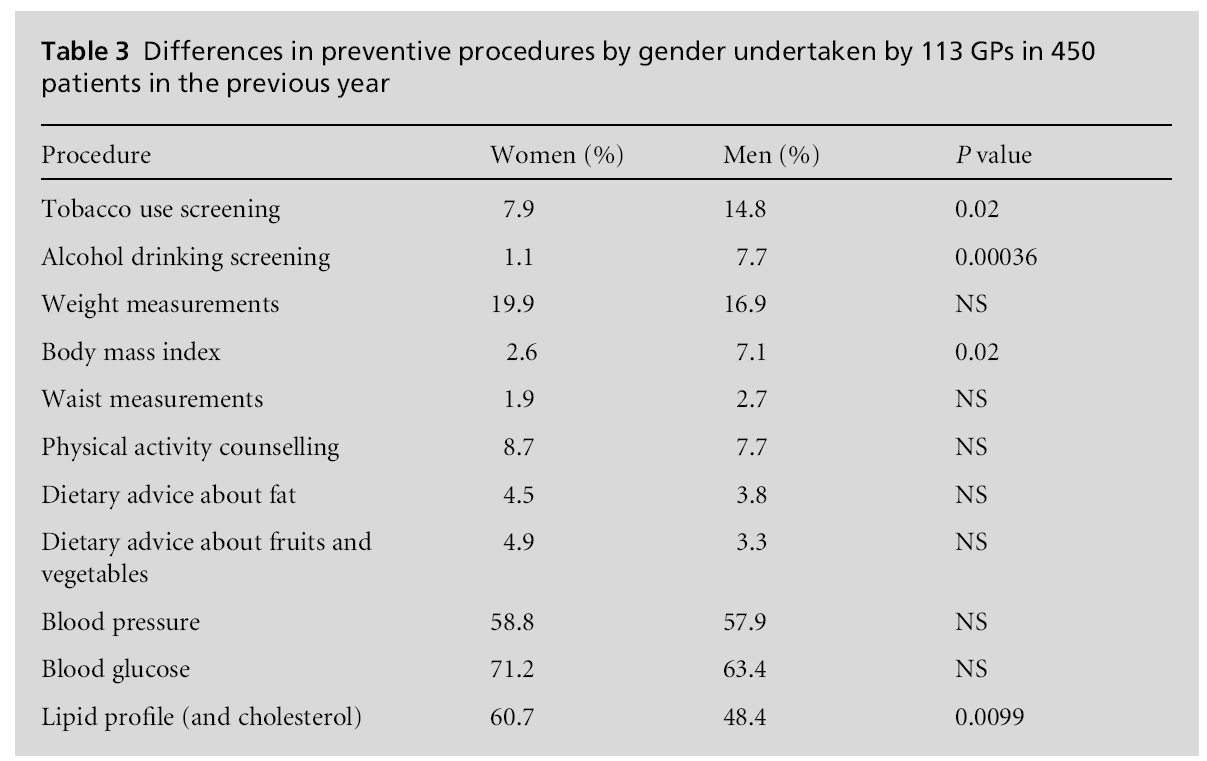
During the observed consultations, screening for alcohol consumption, tobacco use and BMI was more fre-quently offered to men than to women, while women were more likely to have a laboratory test for choles-terol.
The overall delivery of preventive procedures (2.4 per patient per year) in primary care fell below the levels recommended by the Polish Ministry of Health for people aged 40 years in the target group to have the listed preventive procedures each year. The finding of a low rate of preventive interventions in primary care is consistent with previous studies in other European countries.[5] The need to improve prevention is of par-ticular interest to primary care. According to American, European, Australian and World Health Organization (WHO) guidelines, preventive activities such as tobacco use screening, alcohol screening, weight measurement, BMI, waist circumference, blood pressure, diet and physical activity counselling should be offered to all adult patients.[6–9] Lipid profile and blood glucose should be checked in older patients, but cut-off points are different in different countries. According to Polish guidelines they should be checked annually in patients aged 40 years and older. Women or men should be offered prevention in the same way.
In our study, five primary prevention procedures represented 13% of all reported interventions, and together with blood pressure measurements, lipid profile and blood glucose comprised 76.3% of all procedures. According to the literature, the secondary–tertiary prevention model leads to primary prevention being undervalued.[10] It is a challenge for educational pro-grammes to target GPs to focus on the real priorities in prevention efforts for adults aged 40 years and over.
Although women are more frequent attendees than men in primary care, this is not always reflected in their receiving more preventive interventions.[11,12] Some studies show that women receive less prevention, whereas others conclude the opposite. Most investi-gators agree that women receive less lifestyle advice.[4,13] Compared with men, more women had their total serum cholesterol measured. For laboratory-based procedures, not only is a physician’s action involved but so also is a patient’s co-operation. If doctors offer these tests with-out patients’ agreement, they will not be performed. The difference between clinically based preventive pro-cedures and lifestyle advice may be partly explained by the doctor–patients interaction. Brotons et al, in a study among GPs in 11 European countries, observed that more than half of GPs were sceptical of helping patients to reduce tobacco use, decrease alcohol con-sumption, achieve or maintain normal weight, and practise regular physical exercise.[14] It is unusual for patients to ask for lifestyle advice as a specific reason for a consultation, but many will ask doctors for laboratory tests. Many GPs experience pressure from patients who demand unnecessary tests or medical treatment. According to van Steenkiste et al, patients often perceive cholesterol as a very important risk factor, even more important than smoking.[15] Women are often more concerned about their health and may insist on their GP performing laboratory tests to prevent disease or to maintain their healthy state.[13]
It is widely accepted that brief advice against smoking can be effective. For every 50 smokers who receive advice to stop from their GP, one or two will do so.[16] Anti-smoking advice is one of the three most highly ranked preventive interventions.[2] According to Aus-tralian guidelines, smoking status should be checked annually in all patients older than 12 years of age.[8] In our study only 11% of patients were asked about smoking in the previous year. According to the literature, GPs use few opportunities for discussing smoking with patients, advising only a minority of those who consult.[17] In our study, a higher proportion of men received anti-smoking advice, but GPs need to be aware that the number of women smoking is increasing. In Poland, 33.9% of adult men and 19.3% of women are current smokers.[4] As a consequence, the incidence of lung cancer in women is also increasing. Research suggests that patients can become irritated by GPs’ questions about tobacco use.[17] The anticipation of patients’ irritation may explain why GPs are more likely to discuss smoking with patients who have smoking-related problems.[18]
A concern about patient irritation may also explain other missed opportunities for health promotion by GPs. Counselling about obesity is not well received by patients.[19] Obese persons and those who are over-weight are often self-conscious about their weight,[20] which may explain why doctors are not keen to discuss body weight, waist circumference, BMI or dietary advice. It is estimated that in Poland, despite 27% of women and 33% of men being obese, BMI is not frequently measured. In our study it accounted for only 1.9 % of the performed preventive procedures (see Table 2). Discussing obesity, in particular with female patients, may be very difficult and lead to GPs avoiding such uncomfortable situations by simply not discussing them.
GPs’ desire for harmonious relationships with patients also appears to influence the way they discuss alcohol drinking with patients. In general, only 3.8% of the observed patients were asked about alcohol consump-tion, and the gender difference is remarkable: 1.1% of the women, compared to 7.7% of the men (P = 0.0004). Although Poland belongs to countries with a large average alcohol consumption and men drink on average 4.5 times more than women, the rate of annual alcohol screening in primary care is five times less than that in the UK.[4,21] It is clear that educational programmes for GPs to ameliorate preventive counselling needs to pay attention to discussion of alcohol consumption, espe-cially in female patients.
There are several weaknesses in our study. The study sample of doctors was not randomly selected, but based on active recruitment of interested volunteers for a training programme. Recruited physicians may have been more motivated than the average doctor to incorporate prevention in their consultations. The real preventive performance of the average GP in Poland may therefore be lower than that in the current study.
Reported rates of delivered procedures may have been influenced by the presence of an observer. We assumed that doctors performed and offered preventive procedures unaffected by the observer. The recording of preventive procedures in the medical records may vary between physicians, but when a particular inter-vention was observed we assumed that this was effect-ively performed. We believe that direct observation in combination with inspection of the patient record gave fairly reliable estimates of the preventive activities of GPs with any particular patient.
Although we performed our study in one region, many of the factors identified are not unique to Poland and are probably seen in different primary care set-tings in Europe.
In this study we did not explore the effect of doctors’ gender on the delivery of preventive procedures be-cause participating physicians were anonymous. This will be studied during the second phase of the PIUPOZ programme. In the literature, there is evidence that doctors’ gender may affect their performance in pre-vention activities. Bertakis and Rahman found that female physicians were slightly more likely to check patients’ blood pressure, but no significant differences were seen in other non-gender-specific prevention procedures.[22] According to Frank and Harvey, female physicians were reported to undertake systematic patient counselling more often than male physicians.[23]
A strength of the present study was the direct observation of doctors’ preventive behaviour by trained observers. Many previous estimates of the delivery of preventive procedures are based on doctors’ self-assessment or on patients’ medical records, particu-larly electronic records. In Poland, electronic patient records are not common. Direct observation of the doctor and inspection of the patient record was the most appropriate way to study doctors’ behaviour in real life. The healthcare system in Poland is organised by registering patients in a specific primary care setting. Patients cannot follow their personal preference for a particular doctor, which means that every GP has a variety of patients of different ages and gender and limits the possibility of a gender bias whereby female patients register preferentially with female doctors, or male patients with male doctors.
This study is based on direct observation of doctors’ behaviour in combination with the patient record and demonstrated that the annual delivery of preventive interventions in primary care fell below recommended levels. Limited time and resources encourage GPs to perform certain preventive procedures in preference to others. In particular, preventive procedures based on clinical examinations and laboratory tests were performed more often than lifestyle advice.
Education and lifestyle counselling need doctors’ personal engagement and specific communication skills. Preventive guidelines should take into account that patients’ gender and personal attitude to health advice may influence GPs’ performance in preventive pro-cedures. Men are more likely to receive preventive procedures such as tobacco screening, drinking screen-ing and BMI measurement.
Changing beliefs and attitudes of GPs about giving lifestyle advice during routine consultations remains a challenge. Effort made to introduce lifestyle advice and education into the consultation may bring about long-term health benefits and it is planned to encourage this change in doctors’ behaviour through interactive work-shops as part of the PIUPOZ programme.
The study was supported by a grant from Iceland, Lichtenstein and Norway through the EEA Financial Mechanism.
The PIUPOZ programme was approved by the Bioethics Committee of the Poznan University of Medical Sciences, Poland. Informed patient consent was obtained from all patients. All patient/personal identifiers were removed or disguised so the patient/ person(s) described are not identifiable and cannot be identified thorough the details of the story.
Not commissioned; externally peer reviewed.
None.