- (2016) Volume 17, Issue 2
Dattatray Solanke*, Chetan Rathi, Nirav Pipaliya, Prateik Poddar, Vikas Pandey, Meghraj Ingle, Prabha Sawant
Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai- 400022
*Corresponding Author:
Dattatray Solanke
Lokmanya Tilak Municipal Medical College and General Hospital
Sion, Mumbai, India 400022
Phone: +918879447889
Fax: +912224076100
E-mail: dattatraybs@gmail.com
Received: September 26th, 2015 Accepted: December 1st, 2015
Objectives Gastrointestinal visceral artery pseudoaneurysms are rare. This study was carried out in a tertiary health care center in Mumbai to study the patients with gastrointestinal visceral artery pseudoaneurysms due to chronic pancreatitis presenting as gastrointestinal bleed. Methods Patients with chronic pancreatitis presenting with gastrointestinal bleeding due to visceral artery pseudoaneurysms were studied in this prospective study for a period of two years from August 2013 to July 2015. Patients’ demographic data, symptoms at presentation, risk factors, comorbid conditions, laboratory investigations, imaging characteristics were studied. The patients underwent interventions either radiological or surgical. All patients were followed up for three months post-procedure. Results The incidence of pseudoaneurysms in chronic pancreatitis was 7.7%. Twelve patients with chronic pancreatitis had gastrointestinal visceral artery pseudoaneurysms who presented as gastrointestinal bleed. Splenic artery was the most common artery involved (six of twelve patients), followed by gastroduodenal artery (four patients), right gastroepiploic artery (two patients) and short gastric artery (one patient). The size of pseudoaneurysm ranged from 6 mm to 6.3 cm. All patients underwent interventions; transcatheter embolization of pseudoaneurysms in 11 patients and surgical management in the form of splenectomy in one patient. All patients tolerated radiological interventions well without major complications and did not have recurrent bleeding in three months of follow up. Conclusions Pseudoaneurysms of gastrointestinal visceral arteries due to chronic pancreatitis are rare and need prompt intervention either surgical or endovascular. Endovascular therapy in the form of transcatheter embolization is effective in achieving hemostasis. More prospective studies are needed to compare endovascular therapy versus surgical therapy as the treatment modality of gastrointestinal visceral artery pseudoaneurysms.
Keywords
Endoscopy; Pancreatitis, Chronic
Abbreviation
NBCA N Butyl Cyanoacrylate
INTRODUCTION
Vascular complications of pancreatitis are dangerous and can be life threatening. Alarming episodes of bleeding can occur in up to 14.5% of patients with acute pancreatitis and acute on chronic pancreatitis [1].
Pseudoaneurysms are relatively rare complications of pancreatitis. Pseudoaneurysms most commonly affect the splenic artery, gastroduodenal, pancreaticoduodenal, gastric, and hepatic arteries (in that order) [2, 3].
Pseudoaneurysm may rupture into the gastrointestinal tract or other adjacent anatomic structures causing fatal hemorrhage. Bleeding pseudoaneurysms when untreated have mortality of 90-100% and even after aggressive management, the mortality ranges between 18 and 29% [4, 5].
Hence, early diagnosis and prompt treatment is necessary. Endovascular therapy of the pseudoaneurysms is an effective measure to achieve hemostasis. Here, we report a study of 12 patients with visceral artery pseudoaneurysms complicating chronic pancreatitis.
CASE SERIES
Materials and Methods
This prospective clinical study was carried out in the Department of Gastroenterology for a period of 2 years from August 2013 to July 2015. One hundred and fifty five patients with chronic pancreatitis were screened. A total of 12 Patients with chronic pancreatitis presenting with gastrointestinal bleeding in the form of hematemesis or melena and diagnosed with pseudoaneurysm formation of visceral artery on imaging were included. Prior well informed written consent was taken from each of them. Approval from the institutional ethics committee was taken.
Details of patients’ history were noted including demographic data, presentation, comorbid conditions, predisposing factors etc. The patients underwent biochemical investigations; upper gastrointestinal endoscopy, colonoscopy, side viewing duodenoscopy. The diagnosis of chronic pancreatitis was made with clinical features and imaging characteristics. The site of aneurysm was detected with either ultrasonography or CT abdomen or CT angiography and was confirmed with conventional angiography which also served for therapeutic purpose.
All patients diagnosed with gastrointestinal visceral artery pseudoaneurysm were treated with either radiological management with transcatheter embolization or surgical management. No fixed therapeutic protocol was followed and the treatment modality was decided on the basis of individual aneurysm characteristics and hemodynamic condition of the patients.
The patients were kept under observation for 7 days post procedure to see for improvement in clinical symptoms and signs and development of procedure related complications and were monitored for fall in hemoglobin with frequent hemograms. All patients were followed up for 3 months with clinical reevaluation and Doppler ultrasound of the abdomen every two weeks. Repeat computed tomography of abdomen was done after three months.
Successful hemostasis was determined on the following findings: 1) Pseudoaneurysm was excluded from the circulation after embolization and final angiogram did not show extravasation of contrast media; 2) Follow-up of the clinical features demonstrating symptomatic resolution, restoration of blood pressure, stabilization of laboratory findings, and the absence of recurrence and procedurerelated complications; 3) Follow-up CT images showing resolution of hemorrhage or pseudoaneurysm.
OBSERVATIONS AND RESULTS
Patient Characteristics
The incidence of pseudoaneurysms in chronic pancreatitis was 7.7% (12 out of 155 patients screened). The patients’ age ranged from 30 years to 66 years (mean 43 years), nine of the twelve patients were males (75%) and three were females (25%).
Demographic and medical history of the study patients are summarized in Table 1.
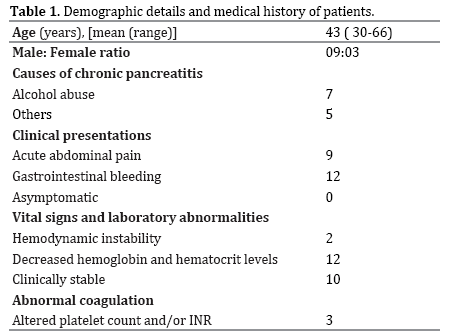
Clinical presentations of the patients included acute abdominal pain in nine patients (75%), gastrointestinal bleed in all of the 12 patients ( hematemesis in seven patients, melena in ten patients, five patients had both hematemesis as well as melena, three patients (25%) had hemosuccus pancreaticus diagnosed on side viewing endoscopy as blood oozing from papilla). A definite source of bleeding could not be found on upper gastrointestinal endoscopy and colonoscopy in these patients, however fresh blood was seen in 5 patients (41.6 %) in duodenum.
All patients had progressively dropping hemoglobin and hematocrit and two patients were hemodynamically unstable.
The causes of chronic pancreatitis were alcohol related in seven patients (58.3%), idiopathic in four patients (33.3%) and postsurgical in one patient (8.3%) who had undergone peptic ulcer surgery in the past.
The table (Table 2) showing the site of pseudoaneurysm formation in individual cases. The splenic artery was most commonly involved vessel in 6 patients (50%), followed by the gastroduodenal (33.3%) and gastroepiploic (16.6%) arteries in 4 & 2 cases respectively. One patient had pseudoaneurysms of both gastroduodenal artery as well as right gastroepiploic artery. One patient had pseudoaneurysm of short gastric artery.
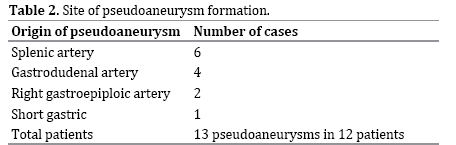
The table (Table 3) shows the individual case details in the form of the arterial site of involvement, the size and number of pseudoaneurysms in each case and management done. The size of pseudoaneurysms ranged from 0.6 cm to 6.3 cm (mean 1.8 cm). One patient had a giant pseudoaneurysm (6.3 cm).
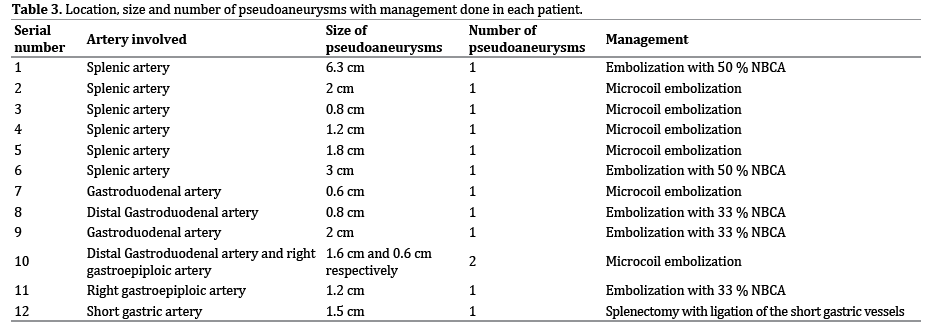
Management
A total of twelve interventional radiological procedures in the form of transcatheter embolization were performed on 12 visceral arteries in eleven patients. The embolization material and procedure was decided by interventional radiologist according to the anatomy of individual pseudoaneurysm and feasibility of the procedure. Transcatheter embolization of the pseudoaneurysms was done using microcoils in six patients (Figure 1) and with N butyl cyanoacrylate glue (NBCA) in five patients. The patient with giant splenic artery pseudoaneurysm (6.3 cm), underwent transcatheter embolization because of hemodynamic instability instead of surgical management which would be preferable in such cases (Figure 2). Final angiograms did not show misplaced coils in nontarget arteries in any of the patients and also there were no cases with unintentional migration of N butyl cyanoacrylate glue into any of the terminal end-organs. One patient underwent surgical management in the form of splenectomy with ligation of the short gastric artery aneurysm (Figure 3).
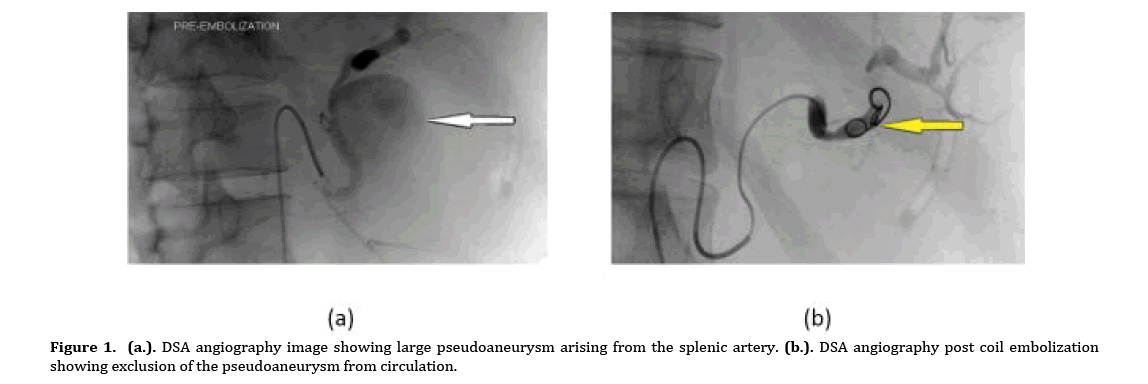
Figure 1. (a.). DSA angiography image showing large pseudoaneurysm arising from the splenic artery. (b.). DSA angiography post coil embolization showing exclusion of the pseudoaneurysm from circulation.
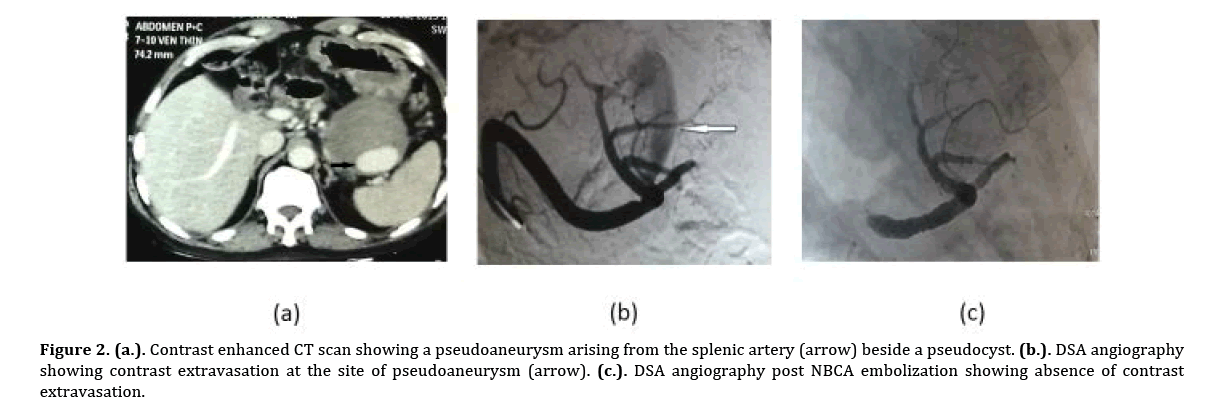
Figure 2. (a.). Contrast enhanced CT scan showing a pseudoaneurysm arising from the splenic artery (arrow) beside a pseudocyst. (b.). DSA angiography showing contrast extravasation at the site of pseudoaneurysm (arrow). (c.). DSA angiography post NBCA embolization showing absence of contrast extravasation.

Figure 3. (a.). Contrast enhanced CT scan showing pseudoaneurysm arising from the short gastric branch of the splenic artery (arrow). (b.). CT angiography showing the pseudoaneurysm (arrow). (c.). Post splenectomy CT abdomen showing resolution of the pseudoaneurysm.
Outcome and Follow up
Successful hemostasis without rebleeding was achieved in all 12 patients. Minor complication in the form of focal splenic infarction occurred in 2 patients, which resolved with conservative management. No major complication or procedure related mortality occurred. No recurrent bleeding was observed on three months of follow up and no mortality was noted. Computed tomography of abdomen after three months showed absence of pseudoaneurysms in all patients.
DISCUSSION
Gastrointestinal visceral artery pseudoaneurysms are rare and are usually consequences of pancreatitis, more commonly associated with chronic pancreatitis (46%) than with acute pancreatitis (6%) [6]. Four percent to ten percent of chronic pancreatitis patients can be complicated by bleeding due to pseudoaneurysms. The bleeding can be fatal at times [7].
The mechanisms of the formation of pseudoaneurysms in pancreatitis include severe inflammation with enzymatic autodigestion of the pancreatic or peripancreatic artery producing arterial disruption, an established pseudocyst eroding into a visceral artery and pseudocyst eroding the bowel wall and intramural artery [8].
Other causes of visceral artery pseudoaneurysms can be peptic ulcer disease, iatrogenic causes (e.g. prior abdominal surgery or endovascular interventions), or blunt abdominal trauma etc. Rapid deceleration in cases of abdominal trauma or road traffic accidents may cause damage to the intima and elastic lamina which may lead to the formation of pseudoaneurysm [9].
Most of the pseudoaneurysms are symptomatic at presentation; however up to 2.5% of cases can be asymptomatic [6]. The presentation of gastrointestinal visceral artery pseudoaneurysms most commonly is with abdominal pain or with bleeding into the gut which can be life threatening or with mass effects on the adjacent neurovascular structures [10, 11].
The pseudoaneurysms can rupture into gut, peritoneum, retroperitoneal spaces, biliary tree, pseudocysts, thoracic, pelvic spaces etc. causing massive bleeding [12]. These may present clinically as sentinel bleed from the drain, hematemesis, malena, splenic rupture or subcapsular hepatic hematoma [11]. Large or giant pseudoaneurysms (5 cm or more in size) can also present with an abdominal lump. One of the patients in this case series had giant pseudoaneurysm of splenic artery measuring 6.3 cm.
Prompt diagnosis of gastrointestinal visceral artery pseudoaneurysms can be challenging because of rarity of the lesions. Radiological imaging is essential to establish the diagnosis. Ultrasound has little diagnostic value for a bleeding pseudoaneurysm. However, duplex Doppler scanning and color flow studies may be helpful in confirmation of neck of pseudoaneurysms. Diagnosis is usually made from noninvasive multiphase computed tomography (including CT angiography) or conventional angiography; however, small pseudoaneurysms can escape detection [10, 13]. According to Marshall et al. dynamic contrast enhanced abdominal computed tomography (CT) should be the first choice of investigation for chronic pancreatitis complicated with a pseudoaneurysm, as the anatomy and location of the pseudoaneurysms can be delineated precisely [14]. They can also be detected on magnetic resonance angiography.
Transcatheter angiography is considered the gold standard for diagnosis as it a reliable test and also has therapeutic potential [15]. Several studies have shown the importance of transcatheter angiography, with sensitivity rates exceeding 90% in localizing bleeding pseudoaneurysms [16, 17]. Hence, it should be done in all patients if tolerable.
For the treatment of both ruptured and intact pseudoaneurysms, various interventions either radiological or surgical can be performed. Transcatheter embolization provides effective treatment of the pseudoaneurysms with good success rates and low complication rates. Tulsyan et al. reported a success rate of 98% for endovascular treatment of visceral artery aneurysms and pseudoaneurysms, with a low 30 day mortality rate of 8.3% [18].
In the study of Udd et al. 33 patients with chronic pancreatitis complicated with pseudoaneurysm bleeding were included; out of which, 22 patients underwent angioembolization successfully. The success rate was related the site of bleeding. For bleeder arteries around the pancreatic head, the success rate was 80% and it was 50% in case of the splenic artery [7]. When transcatheter embolization of pseudoaneurysm is contemplated, most authors suggest embolization of only the feeding vessels, which will result in thrombosis of the pseudoaneurysm [19].
Complications reported after transcatheter embolization include minor complications like pain, pancreatic abscess, splenic infarction or major complications like splenic abscess, and death, all of which are rare.
Surgical management is preferred to transcatheter embolization in cases with pseudoaneurysm related to pseudocyst formation, because of the difficulty of embolizing large pseudocyst cavities and in cases with infected pseudoaneurysms [20, 21]. For the treatment of bleeding pseudoaneurysms located in the distal body and tail of the pancreas, distal pancreatectomy and splenectomy should be preferred [7]. It can serve as a combined treatment in cases where chronic pancreatitis changes are limited to the body and tail of the pancreas.
Size of pseudoaneurysms does not predict their rupture. Even the smallest pseudoaneurysm reported (3 mm) in literature was ruptured at presentation. In addition, incidental diagnosis pseudoaneurysms is less common (2.5%) [6]. Hence, all pseudoaneurysms should be treated irrespective of their size. This more holds true for chronic pancreatitis as it is an ongoing inflammatory process [22].
CONCLUSION
Gastrointestinal visceral artery pseudoaneurysms due to chronic pancreatitis are uncommon vascular lesions. They can present with rupture and massive gastrointestinal bleeding. The size of pseudoaneurysms does not correlate with the risk of rupture, so, repair of all visceral artery pseudoaneurysms is recommended. Conventional angiography provides accurate anatomical details of the pseudoaneurysms and can be used for therapeutic management, hence should be preferred. This limited prospective study highlights the importance of endovascular therapy of gastrointestinal visceral artery pseudoaneurysms which has low failure rates and low complication rates. There is a dearth of prospective studies in literature about this subject and more prospective studies are needed to compare endovascular therapy versus surgical therapy as the treatment modality of gastrointestinal visceral artery pseudoaneurysms.
Conflict of Interest
The authors declare that they have no competing interests.