Research Article - (2025) Volume 33, Issue 1
Received: 10-May-2024, Manuscript No. IPQPC-24-19857; Editor assigned: 13-May-2024, Pre QC No. IPQPC-24-19857 (PQ); Reviewed: 27-May-2024, QC No. IPQPC-24-19857; Revised: 05-Feb-2025, Manuscript No. IPQPC-24-19857 (R); Published: 12-Feb-2025, DOI: 10.36648/1479-1064.33.1.50
Introduction: The U.S. healthcare sector is characterized by a diverse mix of public and private funding and provision, resulting in a lack of a singular governing philosophy. Both the public and private sectors are known for providing high-quality medical services. However, since 1980, healthcare spending in the U.S. has substantially increased. The immense size and financial resources of the healthcare sector make it a prominent target for fraudulent activities.
Aim: This study investigated the impact of collaborative efforts between Managed Care Organizations (MCOs) and oversight agencies on the detection and reduction of healthcare fraud within the Illinois Medicaid program.
Method: This study examines how collaboration between MCOs and oversight agencies impacts healthcare fraud in Illinois Medicaid. A FOIA request for complaint data was sent to the Illinois department of healthcare and family services. The Illinois Medicaid office of the inspector general oversees program integrity and maintains e database to prevent the enrollment of excluded providers.
Results: As of September 20, 2023, 2,741 providers were sanctioned, including 857 physicians, 679 waiver service providers, 159 pharmacies and 157 medicare providers. Over the period from September 2022 to August 2023, 1,059 fraud referrals were recorded, with internal data mining contributing the most (448) and county care being the top-referring MCO (260 cases). The collaborative efforts between MCOs and the Medicaid-office of inspector general led to the identification of $23,830,110 in questioned costs, resulting in a recovery of $13,441,726 in fiscal year 2021.
Conclusion: The findings emphasize the significance of data sharing and transparency in the fight against fraud. The imposition of sanctions on errant healthcare providers has emerged as a key deterrent against fraudulent activities. To combat fraud and information gaps, a comprehensive strategy is needed. This includes empowering patients, improving communication, using advanced analytics and enforcing regulations. User-friendly digital platforms provide reliable information, enabling informed decisions and reducing disparities. Strengthened collaboration and advanced analytics are crucial for early fraud detection, preserving healthcare integrity and preventing financial losses.
There is too much fraud committed in the healthcare system. Since 1980, healthcare expenditures in the US have increased significantly. The sheer magnitude of both the healthcare sector's scale and the substantial financial resources involved render it a prime target for fraudulent activities. Fraud involves intentional deception or misrepresentation intended to result in an unauthorized benefit. Fraud is widespread and very costly to the healthcare. Therefore, prioritizing robust fraud detection measures is imperative for mitigating the overall cost of healthcare services [1].
Kenneth J. Arrow coined the phrase "asymmetric information" to refer to a situation in which there is an imbalance in knowledge among providers of medical services because only a select few have access to pertinent knowledge while the majority does not. Informational asymmetries among economic agents have received a great deal of attention since Akerlof's groundbreaking study in 1970. Akerlof’s “lemon” theory applies in all markets where asymmetric information exchange exists between buyers and sellers. A sick person knows more about their medical needs, giving them an advantage when buying health insurance. They are willing to pay more for coverage due to higher expected medical costs. In response, private insurers screen out high-risk clients, set coverage limits and increase prices [2]. This makes insurance more expensive for healthy people, causing some people to leave. This information gap adds to the high costs, administrative expenses and uninsured population in the U.S. healthcare system. Many Americans struggle to afford necessary care as a result.
In 1971, before the advent of the internet and social media, the prominent Nobel Prize-winning economist Herbert A. Simon, PhD, noted that “information consumes the attention of its recipients” a wealth of information creates a poverty of attention and a need to allocate that attention efficiently among the overabundance of information sources that might consume it. The problem of information asymmetry is exacerbated by ever-growing information overload. The healthcare industry is a trust industry since patients rely on doctors to provide them with good sound advice to stay healthy [3].
Information imbalance among the various actors in the healthcare industry can leave room for fraud to occur. If patients fail to check or request their Explanation of Benefits (EOBs) from their healthcare providers, it opens the door for healthcare providers to bill for services they did not render to that patient. Managed Care Organizations (MCOs) are mandated by federal code 42. The CFR was 438.608 for tackling fraud, waste and abuse in healthcare. MCOs are mandated to have Special Investigative Units (SIUs) that act as the first line of defense for fraud prevention and detection. Considering a situation where a healthcare provider is enrolled with multiple MCOs, there is need for these MCOs to share information on this provider to bridge any information gap they might have with this provider. It is the work of regulators (usually the Office of Inspectors Generals (OIG) to ensure that they bridge the information asymmetry gap between their contracting MCOs through strategies such as focus groups, round table discussions, tag calls and information sharing sessions. MCOs might not be the only source of allegations of healthcare fraud. Other sources of allegation include patients, law enforcement and other external agencies. Healthcare laws such as false claims anti kickback statues and physician self-referral seek to ensure that physicians are making the best decisions for patients and not making decisions on monetary incentives [4]. Regulators such as the Drug Endorsement Administration (DEA0) need to monitor doctors for the prescription of controlled substances such as opioids and ADHD medications (Figure 1).
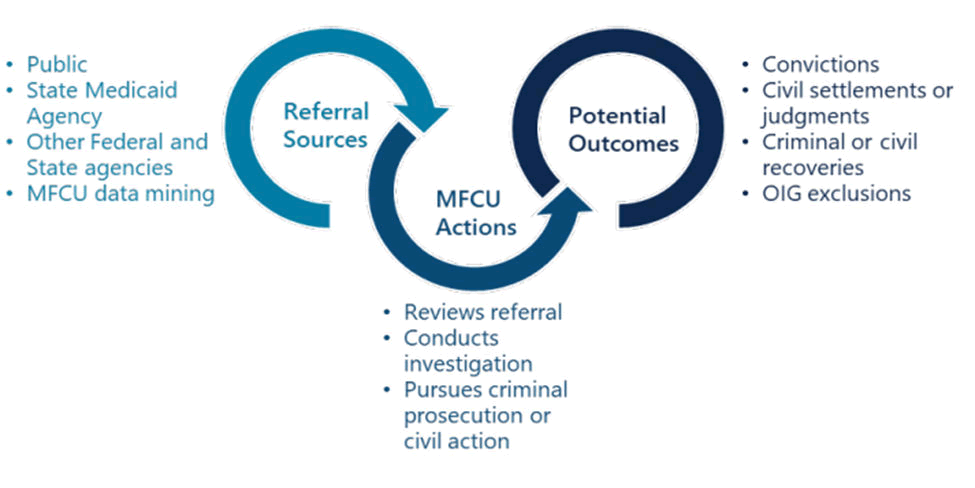
Figure 1: Typical life cycle of a Medicaid Fraud Control Unit (MFCU) case.
Figure 1 above shows how the Medical Fraud Control Unit (MFCU) processes referrals received from the public, internal data mining and from state and federal agencies into potential outcomes such as convictions, settlements, recoveries, terminations and exclusions of providers from State Medicaid Programs. This emphasizes the importance of information sharing among various actors in the healthcare industry in bridging the gap in information asymmetry.
Research question and hypothesis development
• How does the collaborative approach between MCOs and oversight agencies impact the detection and reduction of healthcare fraud in the Illinois Medicaid program?
• How can the medicaid inspector general help prevent healthcare fraud in the wake of information asymmetry?
Information Asymmetry in Healthcare
Information asymmetry occurs in healthcare because patients lack the medical expertise that healthcare providers possess. Patients rely on health providers to work in their best interests without conflict because of this information asymmetry. Numerous authors have studied the effects of asymmetric information on the value and cost of medical care since Kenneth Arrow introduced the topic of asymmetric information in health insurance.
There is a plethora of intricate relationships between individuals who receive, provide, and finance health care in the United States. Everyone is impacted by health care, whether they are well, occasionally ill or suffering from a serious illness. Childbirth, cosmetic surgery, help managing a chronic disease and hospice care at the end of life are all included in the field of medicine. Although the American health care system some of the most cutting-edge options available in the world, it is not the most offers effective. Inequalities in health care costs, availability and quality also exist among the population, mainly due to information asymmetry [5].
Information asymmetries exist in two forms. When important information is dispersed across entities that are close to each other, there is horizontal information asymmetry. Even if some of the entities might have access to more information than others, none of them possesses all the information. When one type of entity has information while another does not and when an aggregated collection of information-poor entities does not, there is vertical information asymmetry. Asymmetrical information between two parties might result in ineffective exchanges and even health consequences. Concerns regarding information asymmetry are crucial when one party is unaware of the caliber of another party or when that party is worried about the behavioral propensity of the other party.
Consumers have limited control over healthcare service choices, leading to inefficiency in the United States due to information asymmetry [6]. This unequal distribution of information among stakeholders is a major issue. The interactions between patients and other healthcare professionals, as well as those between patients and doctors, are governed by professional ethics, which includes both individual and organizational standards of conduct. Among them are moral standards or bioethics, which non maleficence, autonomy and fairness. In their capacity as professionals, doctors are in charge of all patient medical care. Patients who are also consumers are unable to fully comprehend the efficacy of medical interventions because they are more concerned with finding a cure for their illness or a way to achieve pain relief. Therefore, it is particularly challenging for consumers to understand and assess the quality of healthcare services.
Patients with low medical and health literacy may find it difficult to comprehend and communicate their health needs to healthcare professionals, which may lead to higher healthcare costs and subpar health outcomes. However, due to the internet, technological improvements have provided people with a platform for obtaining health-related information that is crucial for managing medical issues. For many, it has become standard practice to access medical information from websites, medical publications, doctors, health plans, family and friends. Often, patients question doctors about treatment plans, forcing them to respond in a considerate manner.
Many economists believe that information asymmetry is a primary cause of market failure. As information overload, continues to worsen, information asymmetry becomes more severe. The COVID-19 epidemic and tightening budgets have heightened the need for cost-effective healthcare worldwide. The evidence implies that practitioners have a low level of cost awareness. According to a systematic review by, only 33% of physicians reported that pharmaceutical companies searched databases for appropriate treatments, and medical device manufacturers struggled to handle requests as demand for their products increased exponentially, highlighting the importance of effective information and knowledge management within healthcare organizations.
Information asymmetry is also a social scenario in which some members of the system have access to information while others do not. The evidence suggests that the health care system has radical information asymmetry. In terms of the development of medical research, the availability of highly qualified physicians and nurses and access to the most recent medications have made the American health care system among the best in the world. However, it is by no means the most fruitful. For instance, the United States was ranked first by the WHO for health spending per person, but only 37th for overall health system performance. It is clear that a doctor does not work in a vacuum and does not independently make judgments; instead, they compete with other doctors inside the facility for better roles, reputation and ultimately for greater pay and cost reimbursement. Currently, without full patient access, medical information is commonly maintained by individual clinicians or private data collectors. To completely describe a patient’s medical history, patients are unable to fully explore alternatives, contribute to and fix inaccuracies in their own data or share their information with new practitioners [7]. By ensuring that accurate health information is made available to appropriate individuals at the appropriate time, patient-centered information exchange should provide patients with more control and better results.
Less documented is the impact that information asymmetry has on healthcare delivery once patients enter the system. Information asymmetry helps cause “lemon-like” outcomes in the following three ways: Doctors and other caregivers overwhelm patients with information and deliver unnecessary treatments; doctors and other caregivers do not engage patients sufficiently and fail to provide necessary care; and uniformed patients demand unnecessary treatments.
Fraud in the US Healthcare Industry
Ai et al., define fraud as “An intentional deception or misrepresentation made by a person with the knowledge that the deception could result in some unauthorized benefit to himself or to some other person.”
In particular, in the United States, fraud occurs frequently and has an impact on a variety of businesses and organizations. One specific form of fraud that has become a major issue for many citizens is healthcare fraud. The American government and its private sector organizations have battled healthcare fraud for decades and the war continues. People often cheat for a variety of reasons, one being pressure. This could be internal or external pressure. Family problems, financial or the drive to advance professionally might put someone under internal pressure. External factors may include a faltering economy. Because healthcare fraud can be caused by a variety of parties, including the patient, the health care professional and any intermediates, fraud identification is difficult, especially in claims involving medical services [8].
Healthcare fraud includes actions taken by a diverse group of people. It encompasses fraud committed by and against medical staff, medical facilities, health insurers, MCOs, producers of prescription medications and other medical supplies and even patients. Health insurance fraud is the deliberate deception of a health insurance company that causes unauthorized payment of healthcare benefits to a person or organization. Billing for services that were not given, up-coding of services, up-coding of products, duplicate claims and unnecessary services are the major categories used to describe claims of health insurance fraud.
Fraud in the healthcare insurance market is a pressing concern, as fraudulent healthcare activities are costly. The ordering of treatments or diagnostic tests that are not required is one of the many scams that are carried out on unwary patients. Aside from actual health concerns, testing and billing are the two areas where there is the greatest danger, notably fraud risk. Up coding is one of the most common fraudulent practices in healthcare coding and billing. Up coding is the practice of invoicing for higher-priced services than those that are actually rendered. This occurs when medical professionals or claimants enter codes that denote either incomplete or un-received treatment. Utilizing patient ignorance to create supplier-induced demand and technology imperatives may indicate that the principle of patient autonomy has been violated. It is never simple to acknowledge healthcare fraud because of its immediate, detrimental effects on human lives. To cease denying losses, however, is the first step toward lowering them. How can a company apply the best solution and lessen losses if it is unaware of the size or type of those losses? Since the advent of electronic medical records, emergency physicians have been shown to adjust their billing codes upward. Although fraudulent billing has always occurred, the era of electronic medical records has made it more blatant [9]. Doctors’ handwritten notes were considerably less likely to contain descriptions of actions that the doctor had not taken. Some people do not seem to be able to resist the desire to employ a few clicks
Approximately one-third of all healthcare costs in the US are attributable to fraud, waste and abuse. Fraud can take many different forms, including being perpetrated by dishonest service providers, organized crimes, complicating patients and falsely stating eligibility for health insurance coverage. Due to its patient demographics and less rigorous payer supervision than commercial insurers, Medicaid, a state-run healthcare program funded by the federal government, is particularly vulnerable. Because the Medicaid system is operated separately and has no coordination between the states, it is particularly vulnerable to fraud and abuse. Because the insurer, beneficiary and provider have asymmetrical information, insurance fraud and abuse are typically difficult to detect. Given that states spend more than a fourth of their annual budget on the Medicaid program, which competes with financing for other crucial services, fraud control enforcement is crucial for the sustainability of states' medical insurance programs.
Individuals' and communities' rights are violated by corruption. Health systems, people, and health outcomes are all significantly impacted by corruption in regard to health. In addition to worsening antibiotic resistance and undermining all our attempts to manage infectious and non communicable diseases, it is estimated that corruption kills at least 140000 children per year. A pandemic that is neglected is corruption [10]. Health-related corruption can range from low-level local corruption to high-level national or even international corruption. It manifests in a variety of ways, including extortion, theft, embezzlement, nepotism and improper influence. Legislation alone cannot stop medicare fraud. Medicare fraud has been acknowledged as a concern since the Clinton administration and partnerships across government organizations have been formed as a preventative measure. Medicare fraud has been a recurring offense and laws and procedures alone have not been sufficient to stop it. Medicare fraud can be reduced but will likely not be completely eradicated with additional investments in governmental collaborations and improved detection tools. To ''keep a lid on'' the issue, continued attention is necessary.
Healthcare fraud continues to pose a serious threat to the American economy and public despite increasing financing and prosecution efforts on the part of the government. Even though healthcare fraud cannot be completely eradicated, particular measures can be used to control these sophisticated fraudulent operations. Drugs that are being sold as counterfeits are those that have been made fraudulently or intentionally or that have had their source, manufacturer, or identity incorrectly identified. Both branded medications and their less expensive generic analogs are subject to counterfeiting. Common counterfeiting targets include expensive high-demand medications such as chemotherapeutic agents, antibiotics, vaccinations, erectile dysfunction medications, weight loss aids, hormones, analgesics, steroids, antihistamines, antivirals and antianxiety medications.
In the United States and throughout the world, the sale of fake pharmaceuticals is on the rise. Since most complaints of fake pharmaceuticals are anecdotal, it is challenging to determine the actual scope of the issue. Additionally, some people may never suspect or recognize that they are taking a product that may be fake or have altered chemicals. The classes of pharmaceuticals that are most frequently found to be fake are antibiotics and anti-parasitics. The prevalence of market-place counterfeit drugs has increased during the last ten years. In regard to the identification, legitimacy and/or effectiveness of the product, counterfeit pharmaceutical products can be defined as the manufacture and distribution of dishonestly labeled drugs. The widespread use of fake drugs has had life-threatening effects on populations, including an increased risk of chronic illness, inadequate treatment results, severe drug responses and fatality [11].
A study by Taleb and Madadha, confirmed that drug fraud is a significant public health issue that affects governments, pharmaceutical firms and the general population globally. It also highlights the need for new statistical databases and national studies on the prevalence of drug counterfeiting to assess and make it easier to monitor the scope of the issue.
Impacts of Information Asymmetry and Fraud
The fraudulent use of health insurance results in annual costs of hundreds of billions of dollars. In particular, the US healthcare sector accounted for approximately one-sixth of the US economy in 2017 (or $3.5 trillion; 18% of GDP). Therefore, it is critical to reduce fraud, waste, and abuse to increase the effectiveness of the healthcare system. High degree of knowledge asymmetry is one of the main causes of greater costs and lower quality. Worldwide, fraud costs the economy more than $4.5 trillion annually. As long as one does not become overtly blatant or arrogant, healthcare providers can cheat because it is simple to do so and generally risk-free. It may be said that lying is a side job. High pay has always been an important factor in choosing to pursue a career in medicine, but today's demand is greater than ever [12].
Healthcare fraud jeopardizes patient safety, lowers the standard of service and wastes limited resources. Untrue knowledge about medicine is one of the greatest threats to world health. By escalating already existing societal injustices, stigmas, gender discrepancies and generational chasms, misinformation can make societies less cohesive. Patient harm can result from taking advantage of patients' ignorance or convincing them to use additional health services during a consultation or prescription. This can be accomplished utilizing the technological imperative, in which doctors push patients to submit to a variety of laboratory tests or offer to employ cutting-edge technology that may not be essential so that they can quickly determine the type of medical care that is needed. Additionally, because of their collaboration with pharmaceutical firms, doctors can also recommend more expensive medications to their patients. Patients may incur increased costs to buy products as a result.
Healthcare fraud is a major issue that costs the American government billions of dollars annually. Fraud, waste and abuse account for approximately one-third of all healthcare costs in the US. The US healthcare system loses between $600 and $850 billion yearly to fraud, waste and abuse, with $125 to $175 billion of this coming from fraudulent behavior. More than US$7 trillion is thought to be spent globally on healthcare services and at least 10% to 25% of that amount hundreds of billions of dollars annually is lost directly to corruption. The amount of corruption wasted by these billions is greater than what the WHO estimates will be required each year to close the gap and provide universal health care globally by 2030. Due to the significant financial repercussions, fraud, especially up coding, is a major concern. To decrease the number of fraudulent instances and associated cost consequences, fraud detection is essential.
The most straightforward form of harm to identify is probably f inancial harm to patients, partly because it reflects economic cost to the government. The cost-sharing nature of the healthcare reimbursement system means that patients are frequently financially impacted by fraud. Fraudulent acts can also affect patients physically, albeit financial harm may be the easiest kind of harm to spot. When unneeded medical operations are carried out just to be reimbursed by the federal health care program, individuals are at risk of physical harm. Patients may suffer less obvious harm from healthcare fraud in addition to financial and bodily loss. Information, primarily patient information, is one of the main commodities in the healthcare system. At its foundation, information is the record of our individual health histories; it will be used to make judgments about future medical treatments as well as for a variety of other things, such as insurance underwriting and job applications.
The health of a patient may suffer from using counterfeit drugs. Adverse side effects, treatment failure, resistance, toxicity and even mortality can occur as a result of the use of subpar medications [13]. Pharmaceutical firms, healthcare workers, pharmacists and patients must all be informed about fake drugs and the laws that are being implemented to stop them.
Drug counterfeiting endangers the public's health, wastes consumer money and lessens incentives for innovation and research. Better state licensing oversight of the medicine vendors would be beneficial prevent patients from losing faith in the value of pharmaceuticals and failing to adhere to their treatments, it is crucial to find a solution to counterfeit drug problems. Consumer purchases of counterfeit pharmaceuticals have significantly increased as a result of the growth of the internet and the challenges in regulating drug sellers via the internet.
Information Asymmetry between Managed Care Organizations and Providers: Implications for Healthcare Fraud in the USA
There are complex and diverse relationships between healthcare fraud and information asymmetry among healthcare providers in the U.S. information asymmetry occurs when one side of a transaction or connection has more information than the other, and it can lead to opportunities for exploitation or unethical behavior.
MCOs frequently rely on healthcare organizations to submit complete and correct claims for payment. Nevertheless, if there is substantial information asymmetry and providers know more about the precise services provided, the coding systems or the medical necessity of the procedures, it may present opportunities for fraudulent billing. Providers may take advantage of this knowledge imbalance by up coding, unbundling or purposefully misrepresenting services.
Due to information asymmetry, it may be difficult for MCOs to properly monitor and identify provider fraud. By filing false claims or participating in actions that are not in the patients' best interests, providers may take advantage of the absence of scrutiny. MCOs may have trouble spotting patterns of dishonest behavior or determining the medical necessity of the services rendered without access to complete and accurate information regarding the services rendered.
Information asymmetry can also be caused by MCOs not having access to complete patient data. Providers may have critical patient-specific data, such as past diagnoses, treatments or prescriptions, those are not disclosed to MCOs. Due to the potential incomplete knowledge of the medical history and current treatments of MCOs, this information gap may result in fraudulent behaviors, including double billing, needless surgeries or prescription fraud.
Addressing information asymmetry between MCOs and providers is crucial in combating healthcare fraud in the USA [14]. Efforts to improve transparency, enhance communication channels and promote data sharing can help reduce the information gap. Implementing robust fraud detection systems, conducting audits and investigations and promoting provider education and compliance programs are additional strategies for mitigating the risk of fraud.
How can the Offices of Inspectors Generally Help Prevent Healthcare Fraud in the Wake of Information Asymmetry?
In light of information asymmetry, regulators such as the Federal and State Offices of the Inspector General (OIG) are essential for avoiding healthcare fraud. The U.S. Department of Health and Human Services (HHS), which functions as an independent oversight body, is in charge of maintaining the integrity of all federal healthcare programs, including Medicare and Medicaid. The HHS-OIG works in collaboration with sister agencies such as the Federal Bureau of Investigations (FBI), Department of Justice (DOJ), Medicaid Fraud Control Units, Medicaid Inspector General Offices and Drug Enforcement Administration (DEA).
To find instances of fraud, waste and abuse within the healthcare system, the OIG primarily conducts audits and investigations. Through these initiatives, the OIG reveals fraudulent schemes, investigates billing procedures and pinpoints fraud-prone locations. The OIG can help resolve information asymmetry by obtaining crucial data and exposing fraudulent acts by using its jurisdiction to access information and investigate suspicious actions. To identify patterns of fraud, the OIG also employs advanced data analytics strategies such as predictive modeling, link analysis, improbable billing hours and time dependent billing [15]. The OIG can find outliers, anomalies, interrelated providers and potential fraud schemes by examining claims data and other pertinent information they receive from the public, law enforcement and MCOs. The OIG can help prioritize investigations and reduce information asymmetry by concentrating on high-risk providers and practices using these data-driven methodologies, which also enhances fraud prevention efforts.
To encourage adherence to federal healthcare rules and regulations, the OIG also offers advice and instruction to healthcare professionals, organizations and beneficiaries. The OIG offers guidelines for preventing fraud, identifies prevalent fraud schemes and assists stakeholders in better understanding their responsibilities through publications, fraud briefs, press releases, public and provider notices and training programs. OIG helps to reduce information asymmetry and promote transparency in the healthcare system by distributing knowledge and encouraging a culture of compliance. State regulators such as the Illinois Department of Healthcare and Family Services release provider’s notices from time to time to keep providers abreast of change policies as well as fee-for-service payment schedules, as does the federal Center for Medicare and Medicaid Services (CMS). These are the ways in which regulators try to reduce information asymmetry. Notably, the Public Health Emergency (PHE) declared in March 2020 raises concerns about how difficult it might be for providers to keep up with changing policies and notices issued by regulators. The uncertainty surrounding public health emergencies has led to constant changes in policies making it difficult for healthcare providers to catch up [16].
To improve fraud prevention efforts, the various Medicaid OIGs work with a variety of stakeholders, including law enforcement agencies, state Medicaid Fraud Control Units (MFCUs), and commercial organizations. This cooperation makes it easier to share information, conduct joint investigations and plan enforcement measures. These organizations can overcome information asymmetries, combine resources and create strategies to prevent healthcare fraud more successfully by cooperating.
To strengthen program integrity and prevent healthcare fraud, the OIG makes policy recommendations. These suggestions might be made in the form of new laws, revised regulations or better program management (Figure 2). The OIG helps to resolve information asymmetry and boost fraud prevention efforts at both the systemic and organizational levels by lobbying for regulatory reforms and exchanging best practices.
Figure 2: OIG analysis of annual statistical reports for FYs 2018 through 2022.
Various Medicaid and Medicare OIG offices also work with other state agencies when they establish from investigations that other agencies are needed to address the original allegation [17]. For example, if a Medicaid OIG office receives an allegation from a patient concerning quality of care concerns, the Medicaid OIG office might refer it to the Department of Public Health to also investigate and address the quality-of-care concerns expressed by the patient in his allegation. For criminal allegations, the Medicaid OIG can also choose to refer to the Federal Bureau of Investigations (FBI).
To answer my research question on how the collaborative approach between MCOs and oversight agencies impacts the detection and reduction of healthcare fraud in the Illinois Medicaid program, I sent a Freedom of Information Act (FOIA) request, pursuant to the FOIA Act, 5 ILCS 140/1 et seq., to the Illinois department of healthcare and family service through its privacy officer for a monthly count of complaint referrals received by the Medicaid office of inspector general from MCOs from 1st September 2022-31st August 2023, organized by an allegation source. The Illinois Medicaid office of the inspector general is the agency that has oversight responsibility for ensuring integrity in the state Medicaid program. The Illinois Medicaid-OIG among other duties maintains a public facing sanction database that keeps track of all healthcare providers who have been excluded, suspended, terminated or barred from the Illinois Medicaid program. These sanctions prevent any MCO from enrolling a sanctioned provider in the Medicaid program.
Illinois Medicaid-OIG Sanctions List Based on Provider Type as at 20th September 2023
Analysis with an excel pivot Table revealed that as of 20th September 2023, 2741 providers had been suspended, excluded or terminated from the Illinois Medicaid program. This list of sanctions is available to the general public including the MCOs who receive sanction alerts firsthand from the Illinois Medicaid-OIG. The sanctions list (which is similar to the federal LEIE database maintained by the HHS OIG) prevents any MCO that has a Medicaid contract with the Illinois state from enrolling a barred provider. The Medicaid OIG might also sanction recipients (patients using strategies including but not limited to locking them to a particular physician or provider . This prevents the recipient from doctor shopping if there is credible allegation of the intent to commit healthcare fraud by the recipient. Of the 2741 sanctioned providers, 857 were physicians, 657 were on waiver service program (usually from other agencies such as the Department of Aging and Department of Revenue Services), 159 were pharmacies and 157 were medical providers (Table 1).
| Provider type | Count of providers |
| Physician | 857 |
| Waiver service provider | 679 |
| (Blank) | 516 |
| Pharmacy | 159 |
| Medicar provider | 157 |
| Dentist | 94 |
| Podiatrist | 42 |
| Chiropractor | 39 |
| Taxicab livery co | 36 |
| Physicians | 29 |
| Oth prov mes-non-reg | 18 |
| Independent lab | 14 |
| Nurse practitioner | 13 |
| Optometrist | 11 |
| Ambulance serv prov | 7 |
| Oth tran prov-no-reg | 6 |
| Rural health clinic | 6 |
| Nursing facilities | 6 |
| Psychologist | 5 |
| Advanced practice nurse | 5 |
| Group | 4 |
| Transportation - AA | 4 |
| Home health agency | 4 |
| Audiologist | 3 |
| Occupational thrpst | 3 |
| Oth prov mes-non-re | 3 |
| Laboratory | 3 |
| Physical therapist | 3 |
| Fed qlfy health cntr | 2 |
| Mentally retrd fclty | 2 |
| Dme/supplies | 2 |
| Nursing | 2 |
| Clinical social | 2 |
| Oth bhvr hlth prfsnl | 1 |
| Registered nurse | 1 |
| Speech therapist | 1 |
| DMHDD-OBRA | 1 |
| Hospice | 1 |
| Grand total | 2741 |
Table 1: Distribution of sanctioned providers in the Illinois Medicaid program as of 20th September 2023.
Managed Care Organizations Healthcare Fraud Allegation Sources between 1st September 2022 to 31st August 2023 through the Illinois Medicaid-OIG Fraud Reporting Portal
The approval to my FOIA request from Illinois Medicaid-OIG came in the form of an Excel file with the various allegation sources, the MCO who submitted it and the record date or time range. I used Microsoft Excel pivot table to analyze and present the table above (Table 2).
| Allegation source | MCO | ||||||
| Aetna | Blue cross blue shield | County care | Humana | Meridian | Molina | Total | |
| Data mining | 89 | 34 | 135 | 10 | 137 | 43 | 448 |
| Customer | 4 | 83 | 46 | 17 | 33 | 22 | 205 |
| OIG subcommittee | 30 | 26 | 48 | 3 | 23 | 33 | 163 |
| Care coordinator | 25 | 65 | 6 | 2 | 22 | 23 | 143 |
| Provider network | 2 | 1 | 13 | 1 | 30 | 2 | 49 |
| Law enforcement | 7 | 5 | 4 | 2 | 1 | 19 | |
| (blank) | 3 | 10 | 1 | 4 | 18 | ||
| HFPP/NHCAA | 6 | 1 | 7 | ||||
| Trade association | 3 | 2 | 5 | ||||
| Service broker | 1 | 1 | 2 | ||||
| Total | 160 | 227 | 260 | 34 | 249 | 129 | 1059 |
Table 2: Healthcare fraud allegation sources submitted by managed care organizations through the Illinois Medicaid-OIG fraud reporting portal between 1st September 2022 and 31st August 2023.
From the above table, we observe that between September 1, 2022 and August 31, 2023, there were 1059 fraud referrals to the Illinois Medicaid-OIG healthcare fraud reporting portal. These 1059 referrals are shared among 6 MCOs who have a Medicaid contract with Illinois State. Of these 1059 referrals, 448 were discovered or found based on internal data mining by the MCO’s. Among these referrals, 205 were customers. Illinois Medicaid OIG-MCO subcommittee meetings accounted for 163 of the referrals. The OIG subcommittee meeting is a periodic meeting that the Illinois Medicaid-OIG has put in place to allow the sharing of information to help reduce healthcare fraud in the Medicaid program. Participants in this focus group include law enforcement agencies, MCOs and representatives from the Medicaid inspector general office, among other sister organizations.
Other sources of allegations include care coordinators, law enforcement agencies and external agencies, the Healthcare Fraud Prevention Partnership (HFPP) and the National Healthcare Anti-Fraud Association (NHCAA). County care (260)made the most referrals through the portal within the time frame. The HFPP and NHCAA are private-public partner organizations committed to combating healthcare fraud.
Illinois Department of Healthcare and Family Service Annual Report 2021
Analysis of the Illinois Medicaid-OIG 2021 annual report shows that the collaboration between the MCOs and Medicaid-OIG led to $23,830,110 in questioned costs. This figure represents total overpayments identified by the collaborative effort of the Medicaid-OIG, MCOs and other external actors. Out of the total $23,830,110 questioned costs, the Medicaid-OIG recovered $13,441,726 in fiscal year 2021 (Figures 3 and 4)
Figure 3: Questioned costs.
Figure 4: Dollars recovered.
The results from the study showed that the collaborative approach between MCOs and regulators such as Illinois Medicaid-OIG in fraud referral reporting plays a crucial role in the detection and reduction of healthcare fraud within the Illinois Medicaid program. The results underscore the critical role of data sharing and transparency in the fight against healthcare fraud. Furthermore, sanctions meted out to healthcare providers who found guilty of misconduct to play a vital role in combating fraud within the healthcare sector.
Addressing information asymmetry and fraud requires a comprehensive approach, including patient empowerment, improved communication, data analytics and stringent regulatory oversight, ultimately contributing to a more transparent, accountable and patient-centered healthcare system. The implementation of user-friendly digital platforms for patients and the provision of reliable and accessible medical information can help individuals make informed healthcare decisions and mitigate the risks associated with information asymmetry. Additionally, strengthening collaborative efforts for information sharing among stakeholders and leveraging advanced data analytics tools are crucial strategies for proactively detecting and preventing healthcare fraud, ensuring the integrity of the healthcare system and safeguarding against financial losses.
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Amponsah AI (2025) From Allegations to Actions: Examining the Impact of Fraud Reporting Mechanisms in Healthcare. Qual Prim Care. 33:50.
Copyright: © 2025 Amponsah AI. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.