Kazuaki Matsumoto1*, Futaba Inoue2, Saori Amano1, Yumie Tamura1, Miho Ashiarai1, Keiko Onda1, Mari Okada1, Masako Imai1, Natsuko Suzuki1, Masayuki Nagasawa1 and Akihiro Oshiba1
1Department of Pediatrics, Musashino Red Cross Hospital, Japan
2Department of Obstetrics and Gynecology, Musashino Red Cross Hospital, Japan
*Corresponding Author:
Kazuaki Matsumoto
Department of Pediatrics, Musashino
Red Cross Hospital, 1-26-1, Kyonan-cho
Musashino City, Tokyo, Japan
Tel: +81-422-32-3111
E-mail: jumbleworks@gmail.com
Received Date: December 18, 2017 Accepted Date: January 15, 2018 Published Date: January 17, 2018
Citation: Matsumoto K, Inoue F, Amano S, Tamura Y, Ashiarai M, et al. (2018) Fitz-Hugh-Curtis Syndrome Preceded by Constipation in a 14-Year- Old Girl. Gynecol Obstet Case Rep Vol.4: No.1:57.doi: 10.21767/2471-8165.1000057
Keywords
Fitz-Hugh-Curtis syndrome; Chlamydia trachomatis; Constipation
Introduction
Pelvic inflammatory disease (PID) is caused by microbes that colonize in the cervix or vagina and spontaneously ascend to endometrium, fallopian tubes and adjacent peritoneum. Majority of the cases are sexually transmitted infections with mostly Chlamydia trachomatis and Neisseria gonorrhea. Occasionally the pathogens reach at the liver capsule and subsequently cause inflammation, which results in adhesion formation between liver capsule and adjacent structures, diaphragm or parietal peritoneum (Fitz-Hugh-Curtis syndrome) [1]. Fitz-Hugh-Curtis syndrome (FHCS) was found in 14% of patients with all PID but more prevalent, nearly 40% in PID with chlamydia [2]. But pediatricians hardly consider Fitz- Hugh-Curtis syndrome in differential diagnosis because it is extremely rare in the pediatric population. Here we present a case of FHCS in a 14-year-old girl whose initial symptom was Pelvic inflammatory disease (PID) is caused by microbes that colonize in the cervix or vagina and spontaneously ascend to endometrium, fallopian tubes and adjacent peritoneum. Majority of the cases are sexually transmitted infections with mostly Chlamydia trachomatis and Neisseria gonorrhea. Occasionally the pathogens reach at the liver capsule and subsequently cause inflammation, which results in adhesion formation between liver capsule and adjacent structures, diaphragm or parietal peritoneum (Fitz-Hugh-Curtis syndrome) [1]. Fitz-Hugh-Curtis syndrome (FHCS) was found in 14% of patients with all PID but more prevalent, nearly 40% in PID with chlamydia [2]. But pediatricians hardly consider Fitz- Hugh-Curtis syndrome in differential diagnosis because it is extremely rare in the pediatric population. Here we present a case of FHCS in a 14-year-old girl whose initial symptom was3
Case Report
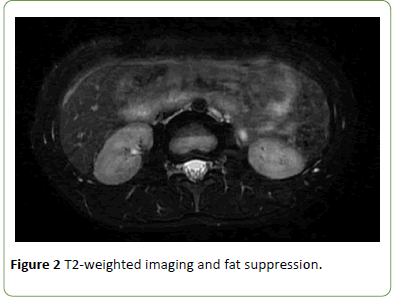
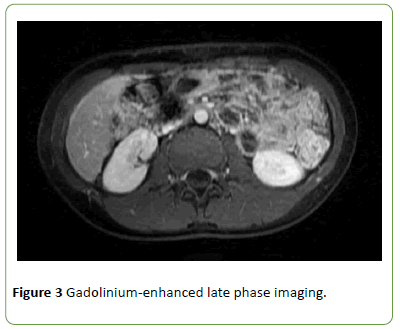
A 14-year-old girl with a prior history of newly-onset constipation and subsequent acute left lower abdominal pain presented to our tertiary care center 10 days before admission. She had no remarkable past medical history or family history. Physical examination revealed soft but distended abdomen. An ultrasonography and X-ray for the abdomen revealed stool accumulation in the entire colon and gestational sac was not found in the uterus. Functional constipation was the leading diagnosis and hard faeces passed after administration of glycerin enema. She was prescribed with laxatives and went home. Her abdominal pain temporarily resolved but the pain subsequently exacerbated and moved to the right flank and finally to the right upper quadrant. She presented to our hospital again and was hospitalized for further evaluation of her abdominal pain. She confessed that she had sexual intercourse with unspecified men and we suspected that she had sexually transmitted diseases. On admission, the vital signs were as follows: body temperature 97.9°F (36.6°C), blood pressure 95/51 mmHg and pulse rate 91 beats per minute. General appearance was good. On physical examination, abdomen was distended with decreased bowel sounds and severe tenderness was located on the surface of the liver. Of note, Valsalva maneuver strongly induced the pain. Her chest was clear to auscultation bilaterally and no heart murmur or gallops were detected. Her genitourinary examination revealed that the vaginal discharge was milky white and slightly increased. Laboratory examinations showed total leukocyte count 11700/mm3 with absolute neutrophil count 8900/mm3 and C-reactive protein (CRP) was 2.26 mg/dL. Liver function tests were within normal limits. A rapid plasma regain test, hepatitis B virus surface antigen, anti-hepatitis C virus antibody, anti-HIV antibody were all negative. A plain computed tomography (CT) scan (data not shown) and gadolinium-enhanced magnetic resonance imaging (MRI) (Figures 1-3) of the abdomen demonstrated perihepatitis, and the diagnosis of Fitz-Hugh-Curtis syndrome was made. We conducted contraceptive education and started ceftriaxone 1 g intravenously every 12 hours and doxycycline 100 mg orally twice daily. We switched doxycycline to clindamycin 300 mg three times daily due to its gastrointestinal adverse effect of emesis. Her vaginal discharge was negative for rRNA of Neisseria gonorrhea and positive for that of Chlamydia trachomatis, which were demonstrated by transcription-mediated amplification. We stopped ceftriaxone and planned to continue clindamycin with the entire treatment course of 14 days. Soon after the antibiotic treatment was started, her abdominal pain was ameliorated and spontaneous bowel movement was observed without laxatives. On the 9th hospital day she was discharged.

Figure 1: Diffusion-weighted imaging.
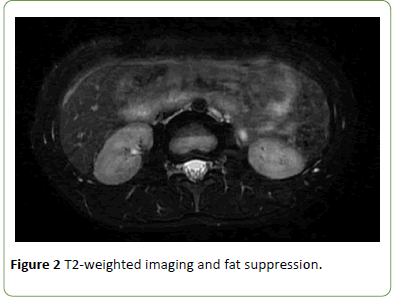
Figure 2: T2-weighted imaging and fat suppression.
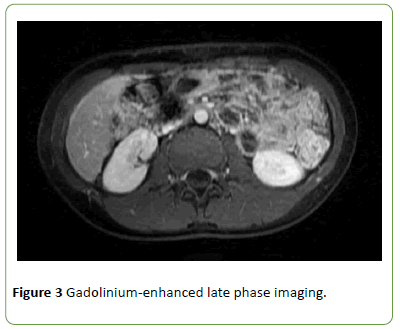
Figure 3: Gadolinium-enhanced late phase imaging.
Discussion
We presented a case of pediatric FHCS with an initial symptom mimicking functional constipation which is the most common cause of abdominal pain among children presenting to the emergency department [3]. Physicians have to consider sexually transmitted infections including pelvic inflammatory disease (PID) and FHCS in differential diagnosis of abdominal pain in sexually active females but pediatricians hardly do so because children are thought to be sexually inactive in general.It is difficult to confirm girls’ history of sexual intercourse because they may tend to conceal the fact.
FHCS was firstly reported in 1920 as gonococcal perihepatitis by Carlos Stajano and and established in the 1930s by Thomas Fitz-Hugh and Arthur Curtis [4]. Subsequently some cases of Chlamydia trachomatis–induced perihepatitis was also reported and the pathogen is widely known to be the leading cause of FHCS [4,5].
The major symptom of PID is lower abdominal pain but the variation in clinical manifestations makes the diagnosis difficult and some cases of PID without clinical synmptoms have been reported [6]. Patients with subclinical PID, defined as inflammation of the upper reproductive tract without overt clinical signs, are asymptomatic whereas severe PID requires surgical management [7]. According to Centers for Disease Control and Prevention 2015 Sexually Transmitted Diseases Treatment Guidelines [8], the diagnostic criteria includes unexplained lower abdominal or pelvic pain and at least one of the following signs: cervical motion tenderness, uterine tenderness and adnexal tenderness. In patients with FHCS, laparoscopy shows adhesion bands on the surface of the liver, violin string appearance and the incidental diagnosis was sometimes made through investigations for abdominal pain [9]. However, as less invasive diagnostic modalities, contrastenhanced computed tomography and ultrasonography are the most commonly used imaging modalities [10], especially in the emergency setting but the sensitivity of ultrasonography for detecting mild FHCS would be low and depend on the clinician’s technic, and exposure to radiation is itself harmful especially for children. Gadolinium-enhanced magnetic resonance imaging is also considered to be useful for detecting FHCS [11]. Prompt broad-spectrum antibiotic treatment covering Neisseria gonorrhea, Chlamydia tracomatis, enteric gram-negative rods, Streptococcus agalactiae, Ureaplasma urealyticum, and Mycoplasma genitalium, Gardneralla vaginalis, and Haemophilus influenza, is necessary to ameliorate damage to female reproductive tract and the standard regimen consists of a third-generation cephalosporin and doxycycline or clindamycin, and the efficacy of parenteral and oral regimens is considered to be similar [12].
FHCS is defined as perihepatitis and usually associated with PID but patients with FHCS often lack lower abdominal pain [13]. Absence of preceding lower abdominal pain does not rule out PID or FHCS. In our case, the patient initially developed left lower quadrant pain presumably due to constipation, which was resolved by glycerin enema. Major differential diagnosis of right upper quadrant tenderness includes cholecystitis, colicky pain caused by gallstone and cholangitis, all of which are extremely rare in children. Newly-onset constipation followed by right upper quadrant tenderness, even though a patient denies preceding signs of PID, strongly suggests FHCS.
Conclusion
Newly developed constipation preceding right upper quadrant pain in a sexually active girl is the important clue to suspect of Fitz-Hugh-Curtis syndrome.
Conflicts of Interest
The authors declare no conflict of interest.
Acknowledgement
Dr. Matsumoto conceptualized and drafted the initial manuscript; Dr. Inoue, Dr. Amano, Dr. Tamura, Dr. Nakatani, Dr Ashiarai, Dr Onda, Dr. Okada, Dr. Imai and Dr. Suzuki collected data and revised the manuscript; Dr. Nagasawa and Dr. Oshiba coordinated and supervised the data collection and critically reviewed the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
References
- Brunham RC, Gottlieb SL, Paavonen J (2015) Pelvic inflammatory disease. N Engl J Med 372: 2039-2048.
- Park ST, Lee SW, Kim MJ, Kang YM, Moon HM, et al. (2017) Clinical characteristics of genital chlamydia infection in pelvic inflammatory disease. BMC Women's Health 17.
- Caperell K, Pitetti R, Cross KP (2013) Race and acute abdominal pain in a pediatric emergency department. Pediatrics 131: 1098-1106.
- Peter NG, Clark LR, Jaeger JR (2004) Fitz-Hugh-Curtis syndrome: A diagnosis to consider in women with right upper quadrant pain. Cleve Clin J Med 71: 233-239.
- Muller-Schoop JW, Wang SP, Munzinger J, Schlapfer HU, Knoblauch M, et al. (1978) Chlamydia trachomatis as possible cause of peritonitis and perihepatitis in young women. BMJ 1: 1022-1024.
- Rueda DA, Aballay L, Orbea L, Carrozza AD, Finocchietto P, et al. (2017) Fitz-Hugh-Curtis syndrome caused by gonococcal infection in a patient with systemic lupus erythematous: A case report and literature review. Am J Case Rep 18: 1396-1400.
- Wiesenfeld HC, Hillier SL, Krohn MA, Amortegui AJ, Heine RP, et al. (2002) Lower genital tract infection and endometritis: Insight into subclinical pelvic inflammatory disease. Obstet Gynecol 100: 456-463.
- CDC (2015) Sexually transmitted diseases: Summary of 2015 CDC treatment guidelines. J Miss State Med Assoc 56: 372-375.
- Onoh RC, Mgbafuru CC, Onubuogu SE, Ugwuoke I (2016) Fitz-Hugh-Curtis syndrome: An incidental diagnostic finding in an infertility workup. Nigerian J Clin Pract 19: 834-836.
- Revzin MV, Mathur M, Dave HB, Macer ML, Spektor M (2016) Pelvic inflammatory disease: Multimodality imaging approach with clinical-pathologic correlation. Radiographics: A review publication of the Radiological Society of North America Inc 36:1579-1596.
- Czeyda-Pommersheim F, Kalb B, Costello J, Liau J, Meshksar A, et al. (2017) MRI in pelvic inflammatory disease: A pictorial review. Abdom Radiol (NY) 42: 935-950.
- Das BB, Ronda J, Trent M (2016) Pelvic inflammatory disease: Improving awareness, prevention, and treatment. Infect Drug Resist 9:191-197.
- Yang HW, Jung SH, Han HY, Kim A, Lee YJ, et al. (2008) Clinical feature of Fitz-Hugh-Curtis syndrome: Analysis of 25 cases. Korean J Hepatol 14: 178-184.