- (2013) Volume 14, Issue 2
Nishi Kothari1, Muhammad Wasif Saif2, Richard Kim1
1H. Lee Moffitt Cancer Center. Tampa, FL, USA. 2Tufts University. Boston, MA, USA
Metastatic pancreatic cancer is a rapidly fatal disease with few therapeutic options. The authors summarize four abstracts (#148,#233, #158, #291) presented at the 2013 ASCO Gastrointestinal Cancers Symposium which were focused on novel agents for metastatic pancreatic cancer.
albumin-bound paclitaxel; Drug Therapy; Pancreatic Neoplasms
ACCORD: Actions Concertées dans les Cancers Colo-Rectaux et Digestifs; FOLFIRINOX: 5-fluorouracil, oxaliplatin, irinotecan, leucovorin; SPARC: secreted protein acidic and rich in cysteine
Pancreatic cancer is a relatively common malignancy, with around 43,000 new cases diagnosed in the U.S. in 2012 [1]. It is also a lethal disease, as evidenced by the rate of death almost matching the incidence.
Gemcitabine has been considered standard of care for treatment of advanced pancreatic cancer since 1997 [2]. Multiple phase III trials have been attempted to improve outcome using gemcitbine as a backbone chemotherapy. However, most of these phase III trials have failed to show improvement in overall survival, with the exception of two studies. A phase III trial using combination of erlotinib plus gemcitabine showed very modest improvement over gemcitabine alone [3]. More impressive results were seen using FOLFIRINOX chemotherapy (5-fluorouracil, oxaliplatin, irinotecan, leucovorin) in the Actions Concertées dans les Cancers Colo-Rectaux et Digestifs (ACCORD) 11 trial [4]. In this study, FOLFIRINOX was shown to improve overall survival by 4 months (from 6.8 months to 11.1 months) compared to the gemcitabine arm. However, significant toxicity was a limiting issue with this multi-drug regimen.
In the first line setting, the National Comprehensive Cancer Network (NCCN) currently recommends single agent gemcitabine in metastatic pancreatic cancer patients with poor performance status and FOLFIRINOX, gemcitabine/erlotinib, or gemcitabine alone for those with good performance status [5]. A phase I/II data has suggested a role for nab-paclitaxel in addition to gemcitabine in the metastatic setting [6], but is still considered category 2B evidence.
Randomized Phase III Study of Weekly Nab-Paclitaxel Plus Gemcitabine Versus Gemcitabine Alone in Patients with Metastatic Adenocarcinoma of the Pancreas (Abstract #148) [7]
Van Hoff et al. conducted a phase III study based on their phase I/II data showing antitumor activity of the combination of gemcitabine plus nab-paclitaxel. Eighthundred and sixty-one patients were randomized to receive the combination regimen versus gemcitabine alone. The combination regimen was comprised of 125 mg/m2 of nab-paclitaxel and 1,000 mg/m2 of gemcitabine on day 1, 8, and 15 every 28 days. The control arm included 1,000 mg/m2 weekly of gemcitabine for 4 weeks and then on days 1, 8, and 15 every 28 days starting with cycle 2. The primary endpoint of the trial was overall survival and secondary endpoints included progression free survival, time to treatment failure, and overall response rate. The results are summarized in Table 1.

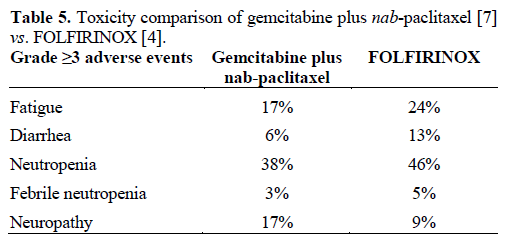
Grade ≥3 adverse events were more common in the combination arm compared to single agent gemcitabine and included neutropenia (38% vs. 27%), fatigue (17% vs. 7%), and neuropathy (17% vs. 1%). However, the grade ≥3 neuropathy improved to grade1 or less within 29 days.
Masitinib in Nonresectable Pancreatic Cancer: Results of a Phase III Randomized Placebo-Controlled Trial (Abstract #158) [8]
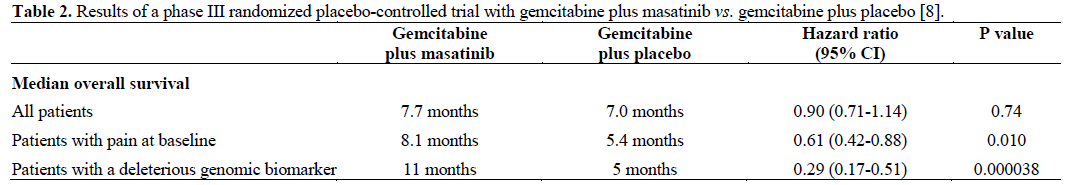
Deplanque et al. conducted a phase III trial randomizing treatment naïve patients to masitinib (a ckit inhibitor of mast cell function) plus gemcitabine versus gemcitabine plus placebo. Increased mast cell activity has been associated with worse prognosis in pancreatic cancer. The primary endpoint for this trial was overall survival and no difference was seen between the two groups. However, two subsets of patients did show improvement in overall survival: those with “pain” at baseline, which was defined as greater than 20/100 on the visual analog score (data was available on 44% of patients), and those with a deleterious genomic biomarker. Sixty-six percent of patients had this latter datum available. Results of the data are presented in Table 2.
Phase II Study of Induction Therapy with Gemcitabine and Nab-Paclitaxel Followed by Consolidation with mFOLFIRINOX in Patients with Metastatic Pancreatic Cancer (Abstract #233) [9]
Ramanathan et al. conducted a phase II study which evaluated patients with a new combination regimen of nab-paclitaxel/gemcitabine induction followed by FOLFIRINOX consolidation (with the omission of bolus 5-FU). This was a very small study with 26 patients accrued thus far. The primary endpoint is to increase 1-year survival to more than 70%. Among the 20 patients treated with the induction phase, 75% have had a significant decrease in CA 19-9 levels and there has been a 50% partial response rate. However, grade 3 or greater adverse events have included neutropenia, fatigue, thromboembolic events, and peripheral neuropathy. This has necessitated several dose reductions or dose delays. To this date, 11 patients have begun the consolidation regimen.
A Randomized, Double-Blind Placebo-Controlled Trial of Trametinib, a MEK Inhibitor, in Combination with Gemcitabine for Patients with Untreated Metastatic Adenocarcinoma of the Pancreas (Abstract #291) [10]
In this study, Jeffrey et al. randomized patients to trametinib plus gemcitabine versus gemcitabine plus placebo in patients with advanced pancreatic cancer. Trametinib inhibits the MEK pathway which is often activated in RAS mutated pancreatic cancers [11]. Primary endpoint was overall survival and secondary endpoints included progression free survival, overall response rate, and duration of response. One-hundred and sixty patients were enrolled and treated. There was no improvement in overall survival, progression free survival, or response rate in patients in the treatment arm. Table 3 summarizes the results.

No benefit was seen even in the KRAS mutant subpopulation. However, there were an increased number of adverse events in the trametinib arm including skin problems, diarrhea, stomatitis, and thrombocytopenia. In addition, the trametinib arm required an increased amount of dose reduction or interruption. Based on this work, there is currently no role for trametinib in the treatment of metastatic pancreatic cancer.
In patients with good performance status FOLFIRINOX has now emerged as a standard regimen [4]. However, the toxicity profile of the regimen remains a concern. At the 2013 ASCO Gastrointestinal Cancers Symposium weekly nab-paclitaxel plus gemcitabine data was finally presented [7]. The rationale behind this combination was established when it was found that the albumin-binding protein secreted protein acidic and rich in cysteine (SPARC) was overexpressed in molecular profiling done on pancreatic adenocarcinoma samples. This protein is not unique to pancreatic cancer and has been noted to be overexpressed in breast and lung malignancies as well as melanoma. Nab-paclitaxel has shown activity in these tumors and is currently approved for relapsed or refractory breast cancer and in the first-line setting for non-small cell lung cancer. Based on this pre-clinical data, a phase I/II study was conducted using the combination of nab-paclitaxel and gemcitabine in patients with pancreatic adenocarcinoma. The results were impressive with response rate of 48%, median progression free survival of 7.9 months and median overall survival of 12.2 months [6].
Therefore at the 2013 ASCO Gastrointestinal Cancers Symposium, the phase III study by Von Hoff et al. [7] was eagerly anticipated. However, even though the trial met its endpoints, the phase III data were somewhat disappointing. Response rate and overall survival were much lower in the phase III study as compared to the phase I/II trial. Also, the results seem to be slightly inferior to the FOLFIRINOX data which showed an overall survival of 11.1 months in the study group versus 6.8 months in the single agent gemcitabine control arm (Tables 4 and 5) [4]. However, the inclusion criteria between the two trials were slightly different. In the Von Hoff study [7] 60% of the patients had Karnofsky score of 90-100 and 40% less than 80%. ACCORD 11 trial only included performance status of 0-1. However, cross comparison of different studies must be undertaken very cautiously.

Based on these data, physicians could potentially offer the gemcitabine plus nab-paclitaxel combination regimen to patients who would not be able to tolerate FOLFIRINOX because of poor performance status. Also gemcitabine plus nab-paclitaxel does not require central access and maybe convenient to some patients. But in the future, selection of chemotherapy regimens should be done using pharmacogenetic testing. As discussed above, high SPARC expression has been associated with improved response to nab-paclitaxel [6]. We are waiting for analysis in the subset of population with high SPARC expression which will be presented sometime this year.
The other two randomized trials discussed here (Abstract #158 [8] and Abstract #291 [10]) did not meet their primary endpoints. Masitinib, a c-kit inhibitor targeting mast cells, and trametinib, a MEK inhibitor, did not improve outcome when added to gemcitabine. However, subset of patients with baseline pain and with an unspecified genomic biomarker did seem to benefit from masitinib and future trials should be conducted is those subset of patients. On the other hand, trametinib did not show improvement even in patients with KRAS mutation. Therefore, this MEK inhibitor as a single agent in combination with gemcitabine should not be used in advanced pancreatic cancer.
Another small trial presented by Ramanathan et al. (Abstract #233) [9] attempted to use the combination of nab-paclitaxel/gemcitabine induction followed by FOLFIRINOX consolidation. Early results seem to be promising but the data has to mature before any conclusion can be drawn.
Overall at the 2013 ASCO Gastrointestinal Cancers Symposium, there was progress made in the treatment for advanced pancreatic cancer. We now have another drug, nab-paclitaxel, which has shown improvement in overall survival. In the future, we hope to continue testing novel targeted agent based on molecular markers with potential therapeutic implications.
None