- (2010) Volume 11, Issue 3
Somanath Padhi1, Ravikanth Kongara2, Shantveer G Uppin1, Megha S Uppin1, Aruna K Prayaga1, Sundaram Challa1, Bheerappa Nagari2, Shastry A Regulagadda2
Departments of 1Pathology and 2Surgical Gastroenterology, Nizam’s Institute of Medical Sciences. Panjagutta, Hyderabad, Andhra Pradesh, India
Received: 13 January 2010 Accepted: 01 March 2010
Context Extragastrointestinal stromal tumors arising in the pancreas are extremely rare. To date, only eight cases have been reported in the literature. Case report A 42-year-old female patient presented with gradually increasing abdominal pain of 6-month duration. Computerized tomography scan of the abdomen demonstrated a solid cystic mass in the body and tail of the pancreas. En-block R0 resection of the mass with distal pancreatectomy, splenectomy and left hemicolectomy was carried out following a radiological diagnosis of a malignant cystic neoplasm of the pancreas. Histopathological and immunohistochemical findings of the lesion were consistent with a gastrointestinal stromal tumor. Conclusion Extragastrointestinal stromal tumor of the pancreas, though rare, should be considered in the differential diagnosis of the more common cystic lesions at this site.
Gastrointestinal Stromal Tumors; Pancreas; Proto- Oncogene Proteins c-kit
Extragastrointestinal stromal tumors, by definition, originate from the soft tissues of the abdomen and retroperitoneum but display no connection to the wall or the serosal surface of the viscera [1]. These are known to arise from various anatomic sites such as the omentum, mesentery, retroperitoneum and gall bladder [1, 2]. Extragastrointestinal stromal tumors arising in the pancreas are extremely rare and only eight cases have been reported in the literature [3, 4, 5, 6, 7, 8, 9, 10]. We report a case of a pancreatic extragastrointestinal stromal tumor in a 42-year-old female patient together with a review of the literature.
A 42-year-old female patient presented with vague abdominal pain which had gradually increased in severity over a six month period. It was associated with loss of appetite and weight. The abdominal examination revealed an ill defined, large lobulated, firm mass of approximately 30x25 cm in the epigastrium, left hypochondrium and extending up to left iliac fossa. The mass was non-ballotable and did not move with respiration.
Routine laboratory investigations were within normal limits except for anemia (hemoglobin: 8 g/dL; reference range: 12-15 g/dL). A contrast-enhanced computerized tomogram of the abdomen (Figure 1) revealed a large heterogeneously enhancing mass of mixed echogenicity (mostly cystic with a few solid areas), measuring 35x30x25 cm, in the region of the body and the tail of the pancreas. The mass did not communicate with the main pancreatic duct. There were no ascites or lymphadenopathy. On magnetic resonance imaging, the mass was hypointense on T1- weighted imaging and hyperintense (cystic) on T2- weighted imaging with hemorrhagic and calcific foci (Figure 2). The possibility of a malignant cystic neoplasm of the pancreas was considered. Upper gastrointestinal endoscopy and colonoscopy showed no abnormalities. At laparotomy, a large mass was found to arise from the body and tail region of the pancreas. There was no attachment to the stomach, and the colon was stretched over the mass. There was no evidence of peritoneal dissemination. To achieve a R0 resection, a distal pancreatectomy, splenectomy and left hemicolectomy were performed.
A large lobulated solid and cystic mass measuring 35x30x25 cm with compressed pancreatic tissue at the periphery was seen at gross examination (Figure 3a). The mass was easily separated from colon. The cut section revealed areas of cystic degeneration with a blood clot (Figure 3b). Cystic fluid analysis for carcinoembryonic antigen (CEA) was within the normal range.
Histopathological examination of the specimen revealed a cellular lesion with compressed pancreatic tissue at the periphery. The cells showed both spindle and epithelioid morphology alternating with acellular hyalinized and myxoid stroma with thick-walled blood vessels. Cellular areas showed spindle cells arranged in fascicles. They had elongated nuclei with tapered ends and moderate amount of cytoplasm (Figure 4). Mitotic figures were 6-8/50 high power field (HPF). Immunohistochemistry with CD117 (prediluted; BioGenex, Cherlapally, Hyderabad, India) showed intense membrane and cytoplasmatic positivity in the cells (Figure 5a). The lesional cells were also positive for CD34 (prediluted, BioGenex, Cherlapally, Hyderabad, India) (Figure 5b) but negative for smooth muscle actin (SMA) (dilution: 1:75; BioGenex, Cherlapally, Hyderabad, India) and S-100 (Figure 5cd). There was no infiltration into the omentum, colon or spleen. The large size (greater than 10 cm), location and mitotic activity of the 6-8/50 HPF classified the lesion as high risk [11]. The patient was kept on close follow-up without any postoperative chemotherapy.
The concept of a gastrointestinal stromal tumor (GIST) has recently been established, due to progress in methods of immunohistochemical analysis. These tumors express CD117 (c-KIT protein) which is expressed in the interstitial cells of Cajal and, thus, in animal investigations, the cells of origin of stromal tumors were recently suggested to be the interstitial cells of Cajal [12, 13]. In 2004, Yamamoto et al. [14] reported that extragastrointestinal stromal tumors share similar KIT mutations to typical GISTs which suggest that these tumors have a similar origin. The origin of stromal tumors in the pancreas with a similar expression of c-KIT protein is extremely rare and has been a matter of recent research.
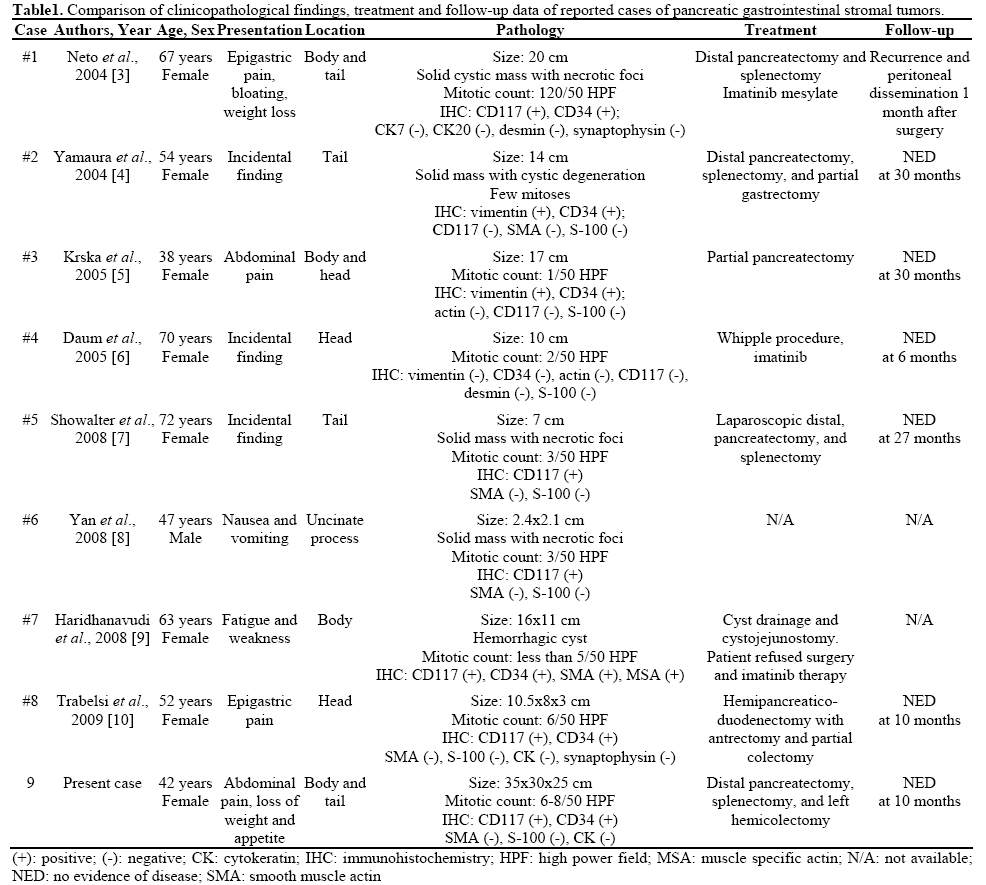
The clinicopathological features and treatment outcomes of previously described pancreatic GISTs, including the present case, are presented in Table 1. There was a distinct female predominance with age ranging from 38 to 72 years (mean age 55 years). The majority occurred in the body and tail of the pancreas with an average size of 12 cm. Five of the eight cases had symptoms of abdominal pain with or without fatigue and weight loss. The mitotic rate in most of these tumors was low except in case 1 (120/50 HPF). This patient had rapid recurrence of the disease with peritoneal and nodal metastasis following surgery and imatinib therapy. For the first time, Yan et al. [8] and Harindhanavudhi T et al. [9] diagnosed two cases of pancreatic GISTs by means of endoscopic ultrasound guided fine needle aspiration cytology (EUS-FNA). On immunohistochemistry, five of the eight cases (cases #1, #5, #6, #7 and #8) demonstrated intense immunoreactivity for CD117 and CD34 whereas three cases (case #2, #3 and #4) showed negative staining for CD117. Reactivity for S-100 and SMA were variable in the lesional cells. Our patient had a relatively large tumor in comparison to other cases. Characteristic CD117 positivity was consistent with a diagnosis of GIST. The follow-up period was uneventful following definitive surgery without any evidence of metastasis. The existence of interstitial cells of Cajal in the pancreas is difficult to explain. Popescu et al. [15] have recently demonstrated the existence of interstitial cells of Cajal in the human exocrine pancreas which have a phenotype similar to the enteric interstitial cells of Cajal. Moreover, Yamaura et al. [4] have shown the presence of c-KIT positive interstitial cells surrounding the intercalated ducts and acinus in the pancreas. Although the exact function of these cells is not clear, the discovery of pancreatic interstitial cells of Cajal supports the diagnosis of an extragastrointestinal stromal tumor arising solely from the pancreas.
The cytologic differential diagnoses of spindle cell proliferation in the pancreas include leiomyoma, leiomyosarcoma, GIST, fibromatosis, inflammatory fibrid polyp, schwannoma and gastrointestinal muscle sampling [8]. Immunohistochemical positivity of CD117 confirms the diagnosis of GIST. Cases of fibromatosis reported in the literature have been shown to react with an antibody directed against CD117, although this does not typically involve the pancreas [16].
The follow-up data of the previous case reports of pancreatic GISTs, including the present one, suggest that pancreatic stromal tumors may follow a benign course following definitive surgery as compared to extragastrointestinal stromal tumors arising from other sites.
To conclude, we presented a rare case of pancreatic GIST. The patient has been followed up postoperatively for ten months and there is no evidence of recurrence or dissemination to date. Although rare, GISTs should be considered in the differential diagnosis of the more common cystic neoplasms of the pancreas. To clarify the relationship between pancreatic stromal tumors and the expression of c-KIT protein, additional research with a large number of cases of pancreatic stromal tumors having c-KIT protein expression is needed.
Conflict of interest The authors have no potential conflict of interest