Research Paper - (2004) Volume 12, Issue 1
Prescribing Advisor (North Locality), Northumberland Care Trust, Morpeth, Northumberland, UK
Sheila Woolfrey BSc PhD FCPP MRPharmS
Principal Pharmacist, Northumbria Healthcare NHS Trust, Ashington, Northumberland, UK
Richard Copeland MPhil MRPharmS
Consultant Pharmacist in Public Health
David Gill MBBS MRCGP DRCOG Dip Med Ed
Prescribing Lead (North Locality)
Gordon Dennett BA IHSM
Head of Strategy Northumberland Care Trust, Morpeth, Northumberland, UK
Accepted date: 22 August 2003
As part of a baseline clinical governance assessment, each pharmacy in Northumberland was asked to record prescription or over-the-counter (OTC) interventions in a one-week period of their choosing between January and March 2002. Twenty-one pharmacies returned a total of 191 intervention forms. Sixty-four documented potential changes to OTC treatments and 81 documented potential changes to prescribed treatments, with 46 relating to prescription clariŽ cation or requests foradvice.Interventions were reviewed by two of theauthors and classiŽ ed according to the type andlevel of impact on patient care.The majority of the prescription interventionsrelated to safety (64%) and most were classiŽ ed aseither signiŽ cant or very signiŽ cant (90%). Fiftypercent of the OTC interventions related to safetyand 45% related to quality of life for the patient.Seventy-seven percent were either signiŽ cant orvery signiŽ cant.The level of contact between pharmacists andgeneral practitioners (GPs) or other prescribers wasassessed and in many cases (49/55, 89%) thereviewers considered that the pharmacist couldhave made changes to treatment without the needto contact the prescriber Ž rst, as is standard practicein hospital pharmacy. If regulations were changedto permit pharmacists to make amendments toprescriptions, and to accept more responsibilityfor patients’ treatments, much GP and pharmacisttime could be saved.
community, patient care, pharmacy
Northumberland is a mixed urban and rural county with a population of 316 000. Northumberland Care Trust was established in April 2002, incorporating primary healthcare and adult social services; it is responsible for the provision of services via 52 medical practices and 63 community pharmacies. Several studies have looked at pharmacists’ interventions in primary care and as a new organisation the care trust was keen to find out what type of interventions were being made routinely by pharmacists in Northumber-land both in terms of quality and quantity.[1–3] This study formed part of a baseline clinical governance assessment for the community pharmacies in North-umberland carried out between January and March 2002.
Pharmacists were asked to record all interventions (defined as any activity to change a patient’s treat-ment) made during a one-week period of their choos-ing in the month following the visit. The interventions in both over-the-counter (OTC) treatments and pre-scribed treatments were included. Data collected included date, initiator of the intervention, problem, solution, relevant history and outcome if known.
The interventions were categorised as ‘OTC’ or ‘prescribing’ by SG. Two reviewers (SG and SW) then classified the interventions in terms of safety, value for money, quality of life and compliance with taking medicines. Interventions were then graded ‘very significant’, ‘significant’, ‘not significant’ or ‘potentially harmful’, as described in a previous paper, according to the expected benefit for the patient.[4] The reviewers also analysed when interventions resulted in either a referral or telephone call to a general practi-tioner (GP) surgery.
Altogether, 61 of the 63 pharmacies took part in the survey and of these 61 pharmacies, 21 submitted intervention forms (response rate 34%).
One-hundred-and-ninety-one intervention forms were returned by the participating pharmacies. On average the pharmacies recorded nine interventions per week. There were 81 interventions recorded in prescribed treatment and 64 recorded in OTC treatment (this intervention rate equates to approxi-mately 0.3% of prescriptions dispensed by community pharmacies). A further 46 recorded events were related to either enquiries for product information or product availability.
As can be seen from Table 1, most interventions were made on the basis of safety (52/81, 64%). Of these, 47 (58%) were classified as potentially having a significant or very significant impact on the patient.
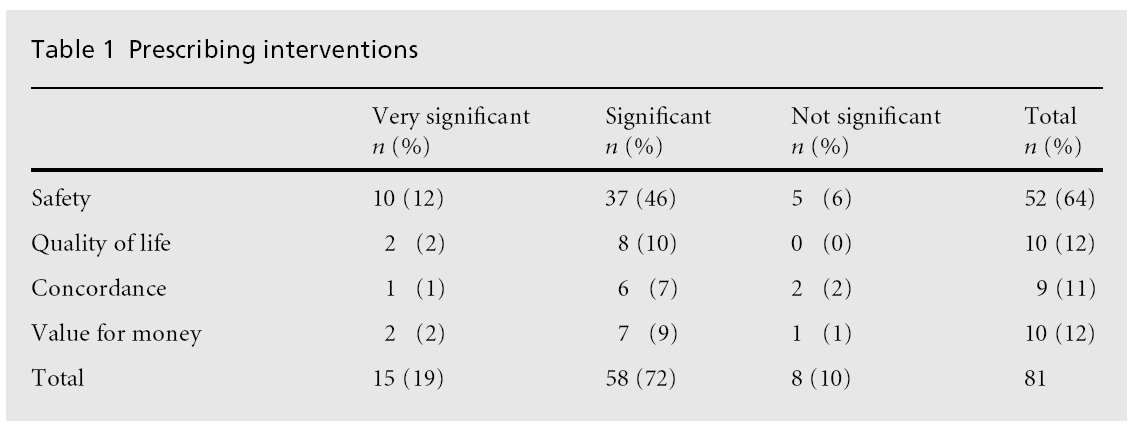
There were relatively few interventions regarding quality of life, concordance and value for money.
Examples of prescribing interventions classed as highly significant
Examples of prescribing interventions classed as highly significant, as defined in the British National Formulary, are shown below.[5]
• A patient with rheumatoid arthritis was prescribed methotrexate 2.5 mg with a dose of ‘take 8 daily’. Methotrexate should be taken once a week in arthritis. This is a potentially fatal overdose if taken for more than a few days. The pharmacist labelled this as a weekly dose but contacted the surgery to correct the error. This caused some friction and the practice receptionist refused to allow the pharma-cist to speak to the GP.
• A four-month repeat prescription was issued to a patient for high-dose proton pump inhibitor (PPI) treatment (ulcer healing drugs) after their two-month course was finished. The pharmacist ensured this was not dispensed, preventing un-necessary treatment with PPIs, which are high-cost medicines.
• A five-fold increase in the dose of haloperidol (an antipsychotic) for an elderly patient in residential care, was prescribed in error. The elderly can be very sensitive to antipsychotics and the dose pre-scribed can induce excessive sedation and postural hypotension leading to a risk of falls.
• Flucloxicillin (a type of penicillin) was prescribed for a patient allergic to penicillins
When OTC interventions were considered (see Table 2), almost all interventions were classified as having a potential impact on either safety or quality of life, with almost equal numbers in each group (32/64 and 29/64 respectively). The most common level of impact was significant, with 13/64 (20%) classified as very significant and 36/64 (56%) as significant in terms of safety. Only two interventions were for compliance or value for money.
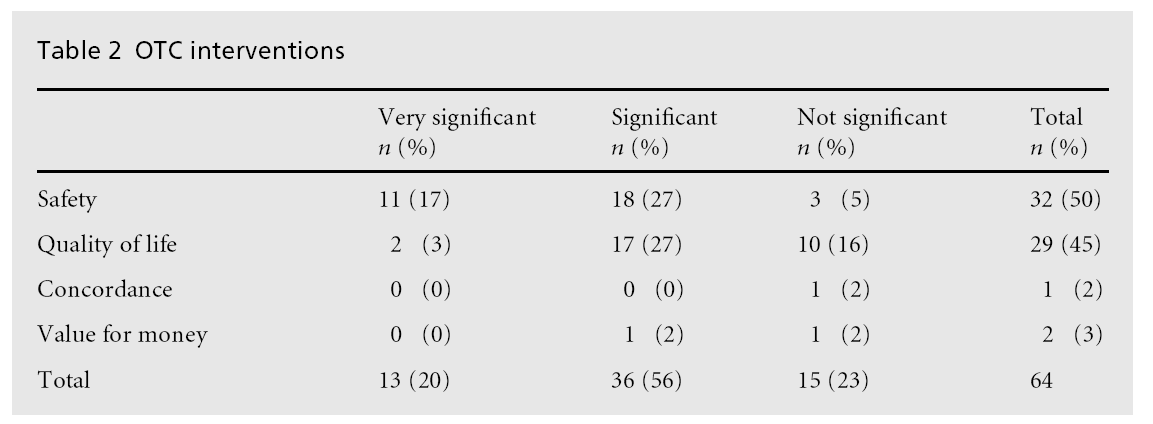
None of the OTC interventions were assessed as having a negative e¡ect on the patient, however, two were classified as inappropriate. On both occasions patients with self-limiting diseases were advised to go and wait until they were seen by a GP and to get specific treatments, one of which was an antibiotic for a sore throat.
Examples of OTC interventions classed as highly significant
• A patient taking the oral contraceptive pill wished to purchase St John’s Wort. Drug interaction would lead to reduced e¡ectiveness of contraception.
• A patient with epilepsy attempted to purchase evening primrose oil (gamolenic acid). Gamolenic acid should be used with caution in epilepsy because it can cause a worsening of the condition.
• A request was made for indigestion treatment for a patient who had had a myocardial infarction two weeks previously. Symptoms of dyspepsia can mimic those of a myocardial infarction or angina.
This study was set up as a pragmatic review of clinical interventions undertaken by community pharmacies in Northumberland. While there are limitations to the study, these data do provide an indication of the types and quality of interventions undertaken by pharma-cists. The majority of interventions were assessed as having a significant or very significant impact on patient care, yet there is no formal mechanism for recording or reporting such clinical activity, either within community pharmacies or via GP practice systems. If all pharmacists in Northumberland made the same level of interventions as the respondents in this study, approximately 600 patients per week would benefit from this activity.
Certainly this type of work is neither remunerated nor explicitly recognised within the NHS. Indeed, since remuneration for community pharmacists is based upon the volume of prescriptions dispensed, there is often a financial disincentive for pharmacists to make clinical interventions; this disincentive becomes more apparent if pharmacists recommend cessation of a particular treatment following a medi-cation review. The fact that one-third of pharmacies returned intervention forms implies that a process of medication review is already taking place in these pharmacies. There is an opportunity for primary care trusts to make use of this in order to meet targets for medication review highlighted within the National Service Framework for Older People.[6]However, to dothis there will need to be incentives introduced for community pharmacists and formal processes put in place between practices and pharmacies to facilitate recording of reviews and implementation of the resulting interventions in treatment.
One of the potential mechanisms to facilitate this is the development of local pharmaceutical services (LPS) pilots. Northumberland Care Trust has had two LPS pilots approved by the Department of Health, and it is pertinent that a key component of both contracts is that the community pharmacist involved under-takes full medication reviews for patients. There is also a degree of optimism that a new national contract for community pharmacies might include remuneration for clinical activity, but details are awaited.
When classifying the interventions, the reviewers noted that many of the interventions required a telephone call to the prescriber although the pharma-cist already knew the solution to the problem. In some instances this was documented as causing some dis-ruption to the doctor’s surgery and pharmacy. An unnecessary call was defined as one where the phar-macist knew the solution but was unable to change treatment without the agreement of a GP. This included adjusting incorrect doses and changes to the dosage form of medication (e.g. tablets for a young child).
For the 79 interventions recorded, 55 (70%) tele-phone calls or referrals were made to the patient’s GP or surgery. In 49 (89%) of these cases the reviewers felt patient care could have been improved without the requirement of a call to the prescriber.
Allowing pharmacists to make some changes to prescriptions would free up GPs’ and pharmacists’ time for more meaningful communication and would probably increase the numbers of interventions made, particularly for reasons other than safety. There was some evidence in the intervention forms that these telephone calls were the source of some antagonism between pharmacists and practices. This work sug-gests that many interventions made by a pharma-cist did not require a telephone call or referral to the GP.
The interventions could be classified into two types, firstly those that are possible with a change in the regulations to allow pharmacists to amend prescrip-tions, and secondly those that would require changes in working practice such as access to medical notes and increased responsibility on the part of pharma-cists. Both are considered routine practice in hospital pharmacy. In all cases pharmacists would require communication channels that allowed records to be made in the patient record in order to prevent the interventions recurring.
Examples requiring a change in regulations
• Heliclear[1] , a combination product used for treat-ing H. pylori infection containing two antibiotics and an ulcer-healing drug was prescribed. The pharmacist wanted to dispense the individual components, since the combination product was not stocked, but had to contact the GP practice in order to e¡ect this.
• Breath-actuated salbutamol was prescribed when the patient wanted a metered dose inhaler for use with a spacer device (the inhaler prescribed was not compatible with the spacer device). The pharmacist phoned the surgery to get the pre-scription changed. To get the prescription changed the patient needed to re-attend the surgery. Then the wrong quantity was prescribed.
The pharmacist phoned the surgery receptionist, who refused to get the quantity changed. The patient then needed to revisit surgery to get the prescription amended.
Examples requiring a change in working practice
• Aciclovir 500 mg tablets were prescribed on a home visit (this strength of tablet does not exist and does not correspond with any known treatment dose). The pharmacist phoned the GP to find out what strength to dispense.
• Celebrex (celecoxib) was prescribed to a patient already receiving lithium. Celecoxib interacts with lithium to increase plasma levels and this can potentially lead to lithium toxicity. The pharmacist phoned the patient’s GP with these concerns. The prescription was not stopped or the lithium dose reduced.
Barriers to communication between pharmacists and GPs have been identified in several studies as:[7–9]
• practical di¤culties in synchronising calls with work practices between professionals
• lack of training
• GPs’ reluctance to cede professional territory
• pharmacists’ deference to GPs
• geographical separation of pharmacies and GP surgeries
• requirements for community pharmacists to be on the premises during working hours
• lack of feedback from GPs to community pharma-cists
• uncertainty about how the GP will receive inter-ventions.
These barriers to communication, in conjunction with the requirements for pharmacists to obtain permis-sion from prescribers for even the most minor changes to prescribed treatments, make it very di¤cult to resolve problems within the prescribing and dis-pensing process. The Prescription Pricing Authority (PPA) requires community pharmacists to obtain GPs’ signatures for any change made to a prescription before they will authorise payments to reimburse the cost of medicines dispensed. In addition, community pharmacists are required by the PPA to make a declaration that the medicines dispensed in any month are exactly as prescribed on the prescriptions submitted. If this is not the case, pharmacists run the risk of breaking their terms of service and being either under-reimbursed for medicines dispensed or accused of fraud.
This study has received enthusiastic backing from GP clinical governance and prescribing leads in the Northumberland Care Trust, and its implications were the subject of debate at the Professional Execu-tive Committee (PEC). The PEC has endorsed the following actions:
• hold discussions with the PPA, to develop mechan-isms for community pharmacists to alter prescrip-tions when there is the need to supply medicines in an alternative form, without the need for a GP to amend or re-issue the prescription
• determine a range of interventions which may be acted upon by community pharmacists without the need to contact a GP each time
• develop pilots incorporating IT links between community pharmacists and general practices.
Community pharmacists already contribute to the clinical care of patients. Progress on the above actions will enable community pharmacists to increase their contribution to patient care, and will enhance their development as integral members of the primary healthcare team.
None.