Research Paper - (2015) Volume 23, Issue 1
School of Psychology, Cardiff University, Park Place, Cardiff, CF10 3AT, UK
Adrian Edwards
Cardiff University, School of Medicine, Cochrane Institute of Primary Care and Public Health, Cardiff, CF14 4XN UK
Background and objective Cardiff and Vale out-of-hours
service (Wales, UK) adopted the ‘expert triage’ service model in
April 2013. The purpose of the model was to train and support
General Practitioners (GPs) to provide high quality triage in
terms of process and outcomes. The aim of this study was to
analyse effects on triage outcomes and to examine patient and
GP experiences of the ‘expert triage’ service model.
Method Triage outcomes of telephone advice, primary care
centre appointments, home visits, and Accident & Emergency
referrals were analysed as a ‘run chart’; a graph used to depict
changes across time. Telephone interviews were conducted with
samples of participating GPs and patients, which considered
patient understanding and use of triage information and GP
perception of the changes adopted by the new model. Interview
responses were coded and analysed thematically as themes and
subthemes.
Results Primary Care Centre appointments and referrals
to A&E departments declined after introduction of the
expert triage model. Patient understanding and use of triage
information was similar for previous model and expert triage
patients. There appeared to be greater intention to use in-hours
GP surgeries but more disagreement with the recommended
treatment pathway for expert triage patients. Expert triage GPs
perceived that there was improved triage quality, enhanced
capacity and fewer delays to assessment. Both patients’ and
expert triage GPs’ responses indicated awareness of the need
to improve patient knowledge and to enhance appropriate use
of the service.
Conclusions Triage outcomes and interview responses
provide a positive account of the ‘expert triage’ model, although
some limitations were apparent from patient responses. Further
improvements in this GP out-of-hours service may also be
possible from implementing suggestions from participants’
responses in light of their experiences.
Out-of-hours medical care, quality improvement, general practice, health services research, primary health care
How this fits in with quality in primary care
What do we know?
There has been emphasis on evaluating service models prior to implementation and training to provide skills and knowledge necessary for telephone consultations. The organisation and delivery of out-of-hours services have received extensive attention, however, the impact of using an expert triage system on service quality and user and provider experience has received little attention.
What does this paper add?
Cardiff and Vale out-of-hours service (Wales, UK) adopted an ‘expert triage’ model of care, which implemented a number of strategies, such as training workshops, revised prioritisation algorithms, and triage targets. Improved outcome targets, and positive user and provider experience were found from evaluating this service model. Implementation by other out-of-hours services may improve service quality and patient and clinician experience further afield.
There is increasing pressure on all unscheduled care services and provider interest in how such services can be improved. In GP out-of-hours services there is particular interest in whether experienced triage staff can achieve greater quality of care, whilst also managing demand.
Ensuring that new service models are evaluated before they are introduced is fundamental. This is particularly so for out-of-hours services as they are associated with greater risk due to clinicians and patients not knowing each other and the condition often being urgent.[1] Cross-cultural analysis of out-of-hours care has revealed that several different models exist alongside each other in most Western countries, with the Accident and Emergency department being the most frequently used model, and countries differing in the provision of Primary care centres and telephone triage services.[2] Importantly, a significant proportion of the countries who took part in the survey had plans to alter the provision of out-of-hours care to large scale organizations, reflecting a prevalent measure for managing demand for out-of-hours primary care.[2] A previous survey regarded telephone triage favourably for accessibility and patient satisfaction but negatively for satisfaction of out-of-hours physicians. ² Emphasis has been placed on training courses to enhance appropriate attitudes, skills and knowledge necessary for telephone triage to aid patient and physician satisfaction. Improving awareness of when telephone consultations are inappropriate, training in verbal sensitivity and guidance on managing patient expectations were found to be important content of training. [3] In addition to service provider and user satisfaction, higher quality of telephone triage has been shown to be positively related to appropriateness of decisions and accuracy in estimation of urgency.[4]Such findings illustrate the importance of targeting consultation quality in training and supporting triage providers.
Triage models adopted in other primary care services have provided mixed results. The out-of-hours provider NHS 111 adopted a telephone triage intervention for non-emergency health problems operating 24 hours 7 days a week.[5] The intervention was operated by non-clinical call handlers using decision algorithms. Emergency service use remained constant immediately after the intervention but there was an increase in emergency care use with each month following implementation. [5] However, Kelly et al. conducted a survey of out-of-hours primary care models in Wales and found telephone advice to be associated with increased patient satisfaction and enablement compared to consultations in a treatment centre.[6] An expert triage model has been adopted by some out-of-hours services in the Netherlands, although this triage system received mixed opinions as to whether the quality of triage would be sufficiently enhanced.[6] The service using the expert triage system had significantly longer mean call duration but call decisions resulted in less contact with a GP either through telephone or face-to-face consultation.[7] The authors recognised that the differences may arise from comparing different services rather than different triage systems; therefore, it cannot be proven that these differences were a result of the expert system.[7] The present study rectified this problem; analysing patient and GP experiences and triage outcomes before and after implementation within the same service.
We aimed to examine the effects of the ‘expert triage’ service model introduced by Cardiff and Vale Health Board’s out-of-hours service (Wales, UK) on 1st April 2013. The service typically receives about 8500 calls per month. Under the previous service model, non-clinical call handlers would obtain symptoms from patients or their representatives and by protocols for appropriate assessment, would offer the most appropriate treatment pathway. In response to service pressures resulting from high proportions of patients being classed as urgent and being offered face-to-face appointments, the ‘expert triage’ model was adopted. Under this new model, all callers to the out-of-hours service were triaged by a clinician, usually a GP, who would recommend the most appropriate treatment pathway. Call handlers remain the first point of contact; gathering case information and prioritising cases according to prioritisation guidelines. The triage clinician then calls back patients according to the prioritisation list. A number of strategies were adopted in its implementation. Triage providers attended training workshops which aimed to improve triage productivity, communication skills and appropriate use of triage outcomes of appointments and telephone consultations. The prioritisation support systems were revised to reflect in-hours practice, triage targets were implemented, and scheduled face-to-face appointments were lengthened from 10 to 12.5 minutes. Pay rates also improved under the model, which was thought to facilitate recruitment of GPs to the service. The aim of this study was to analyse patient and GP experiences of the ‘expert triage’ service model and effects on triage outcomes, particularly whether the changes were effective in overcoming the outcome challenges present under the previous model.
Overview
The ‘expert triage’ model was implemented on the 1st April 2013, aiming to improve triage quality and outcomes, and to improve training of experienced triage GPs. The proportion of calls concluded by telephone advice, face-to-face consultation or home visit, before and after the service change was the principal outcome. This was complemented by interviews with patients who had used the service before or after the changes, and with GPs involved in expert triage.
Design
Telephone interviews were conducted with patients and face-to-face interviews were conducted with GPs. Responses were analysed for themes and subthemes. Triage outcome data was extracted from a statistics database held within the out-of-hours service.
Participants
The patients under the ‘previous’ service model were recruited from the Adastra patient database, a clinical patient of case details from 1st January 2013 to 1st April 2013. This search excluded teenage children (where follow-up may raise confidentiality issues) or dental calls. After two rounds of invitations, 16 ‘previous’ service users had been recruited and provided responses, all of whom had used the service in either February or March 2013. Twenty ‘expert triage’ patients were also randomly selected from Adastra from lists of recent users during June-July 2013.
The triage GP sample consisted of 19 triage practitioners who were recruited from a list of 40 Cardiff & Vale triage providers based on their willingness to participate. They included one GP who had left the service since the adopted change, three who had left but re-joined the service under ‘expert triage’, two medical advisors, and thirteen triage practitioners who had worked for the service under both the ‘previous’ and ‘expert triage’ models.
Data collection
Triage outcome statistics were extracted before and after the service model change from a statistics database updated monthly and maintained within the out-of-hours service. Triage GP and patient experiences were explored through interviews, conducted with a question schedule, with both fixed response and open-ended questions, and with field notes recorded during each interview. The interview schedules were developed and revised with support from the head of unscheduled care; telephone interviews were voice recorded and played back during data analysis and face-to-face interviews were recorded in writing. Data were managed through recording the case details and interview time for telephone interviews and GP identity as ‘left’, ‘advisor’, ‘new’, or ‘both’ for face-to-face interviews. Both patient samples were interviewed by telephone in July 2013 lasting an average of 5 minutes, with those receiving triage under the ‘previous’ model using the service in February or March 2013 and those under the ‘expert triage’ model using the service a few days prior to interview. Of the triage GP sample, fifteen were interviewed face-to-face in their in-hours surgeries and the remaining four took part in telephone interviews, all lasting 30 to 45 minutes and taking place during July-August 2013. All telephone interviews were conducted from the triage centres.
Patients were asked questions about their understanding and use of the triage information, and their experience of the service. The GP sample were asked about the strategies and targets implemented by the model and about their suggestions to improve the service.
Data analysis
The triage outcome data are presented from before to after the service change in the form of a ‘run chart’ to depict change in treatment pathway outcomes across time and sustainability of such change (see Figure 1).[8]
The interview responses were summarised descriptively, content analysis was undertaken, and themes and subthemes were identified.
Triage outcomes
Changes in the proportion of service users receiving telephone advice, face-to-face consultation or home visits, before and after the service change are shown in Figure 1. The proportion of service users receiving primary care centre appointments decreased by approximately 11% following the service change and was maintained in the first fifteen months of the service. There was also a decrease in recommended attendances to Accident and Emergency centres.
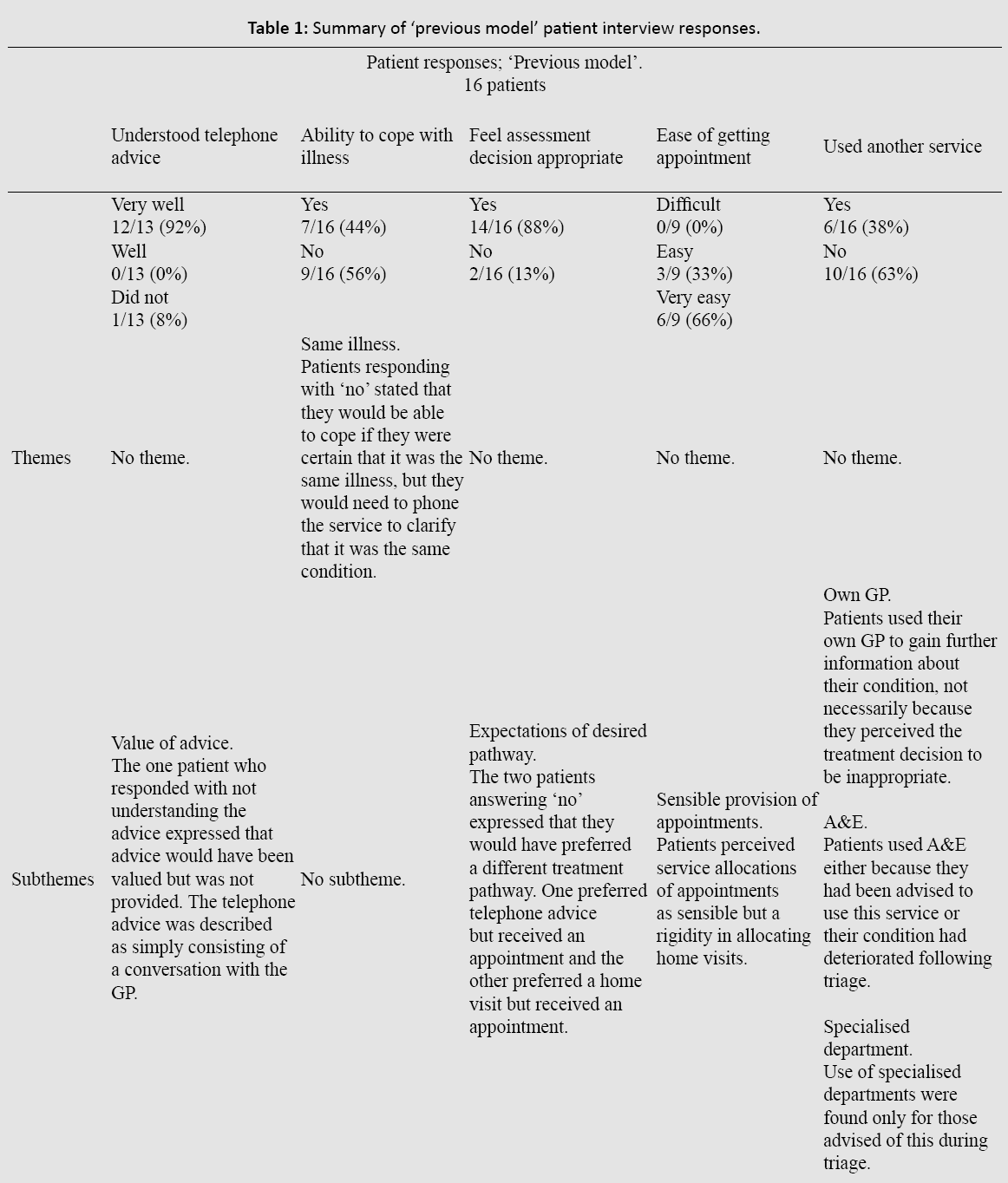
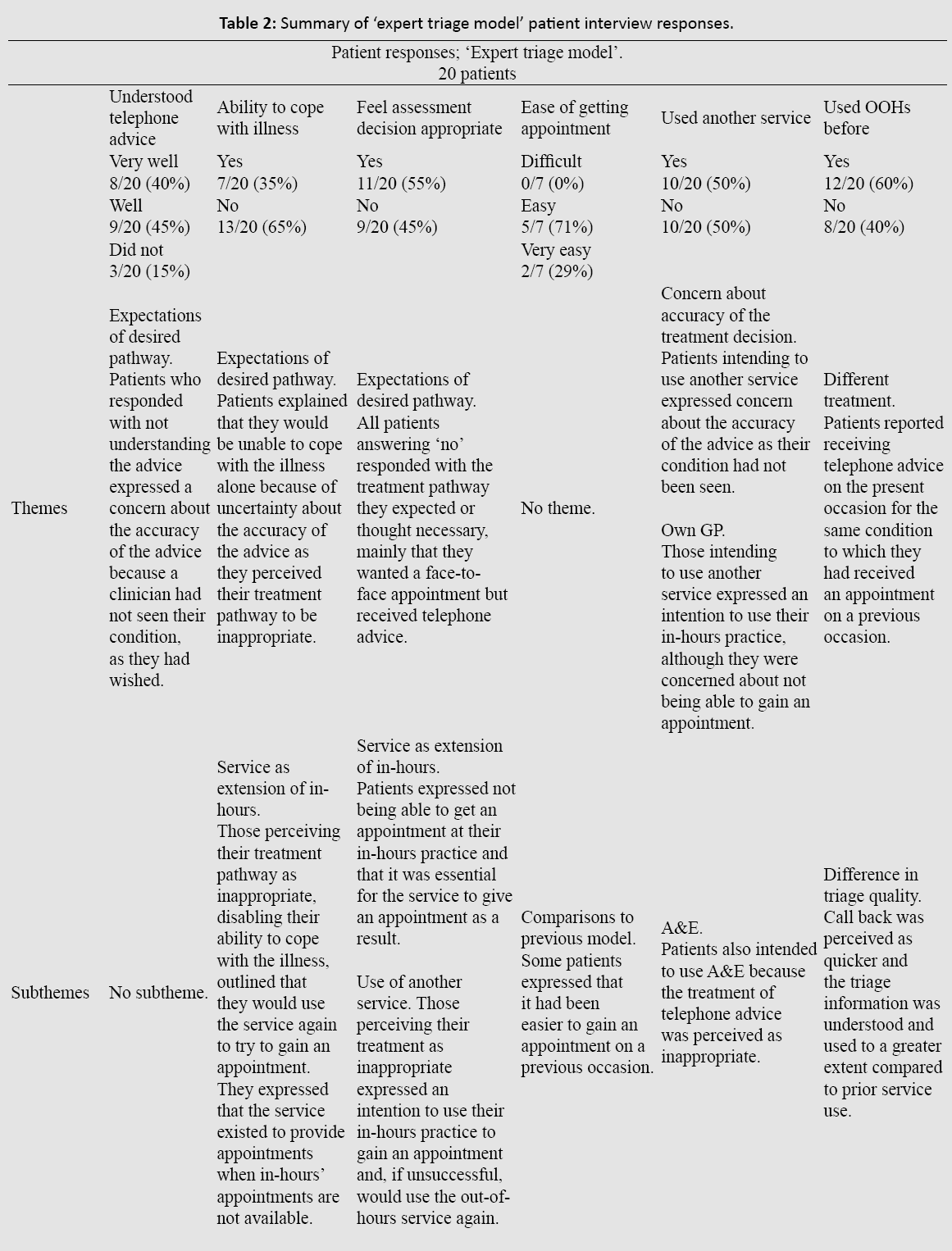
Patient experiences
Although many patients using the ‘expert triage’ service reported satisfactory outcomes in terms of their ability to understand (8/20) and cope with their illness (7/20) (“I did not need an appointment in the end because I understood the information over the phone”; “The information put me on the right path of care, (I have) better understanding of the illness and treatment”), there was some suggestion that ‘expert triage’ patients felt less able to understand the telephone advice given or to cope with their illness in some situations (fewer respondents reporting understanding the advice “very well”, able to cope with illness; (Table 2). ‘Expert triage’ patients gave some indication that it felt less easy to get a face-to-face appointment (“Very easy” 2/7; “Easy” 5/7) (“I received out-of-hours care years ago.
It was better before because they would definitely have given an appointment”), and that the assessment recommended was not appropriate (almost half 9/20 indicating “not appropriate”) (“Advice decision was not appropriate. I would have preferred an appointment”; “(I) would have preferred an appointment, especially as I raised concern about getting an appointment at my own GP”; “I am more anxious now than before as no one has seen the problem. I have not seen anyone to reassure me”). These patients also reported that they had used another service more often during the same episode (10/20; usually the patients’ own GP in-hours) (“I went to my GP surgery after to receive further information”). Among the users of the ‘expert triage service’ who also had experience of using the ‘previous’ model (12/20), comparisons between prior and present use of the out-of-hours services were variable – some perceiving better or poorer quality advice this time, or that telephone advice was more or less favourably received. These respondents perceived shorter waiting times to receive advice (“I received out-of-hours advice before. It was better this time. The information was better and I waited less time for the doctor to call back”; “I received advice before. This experience was better, (the) response was much quicker”), but no respondent reported perceiving longer appointments when seen face-to-face. Themes and subthemes of patient responses are provided in Table 1 and Table 2.
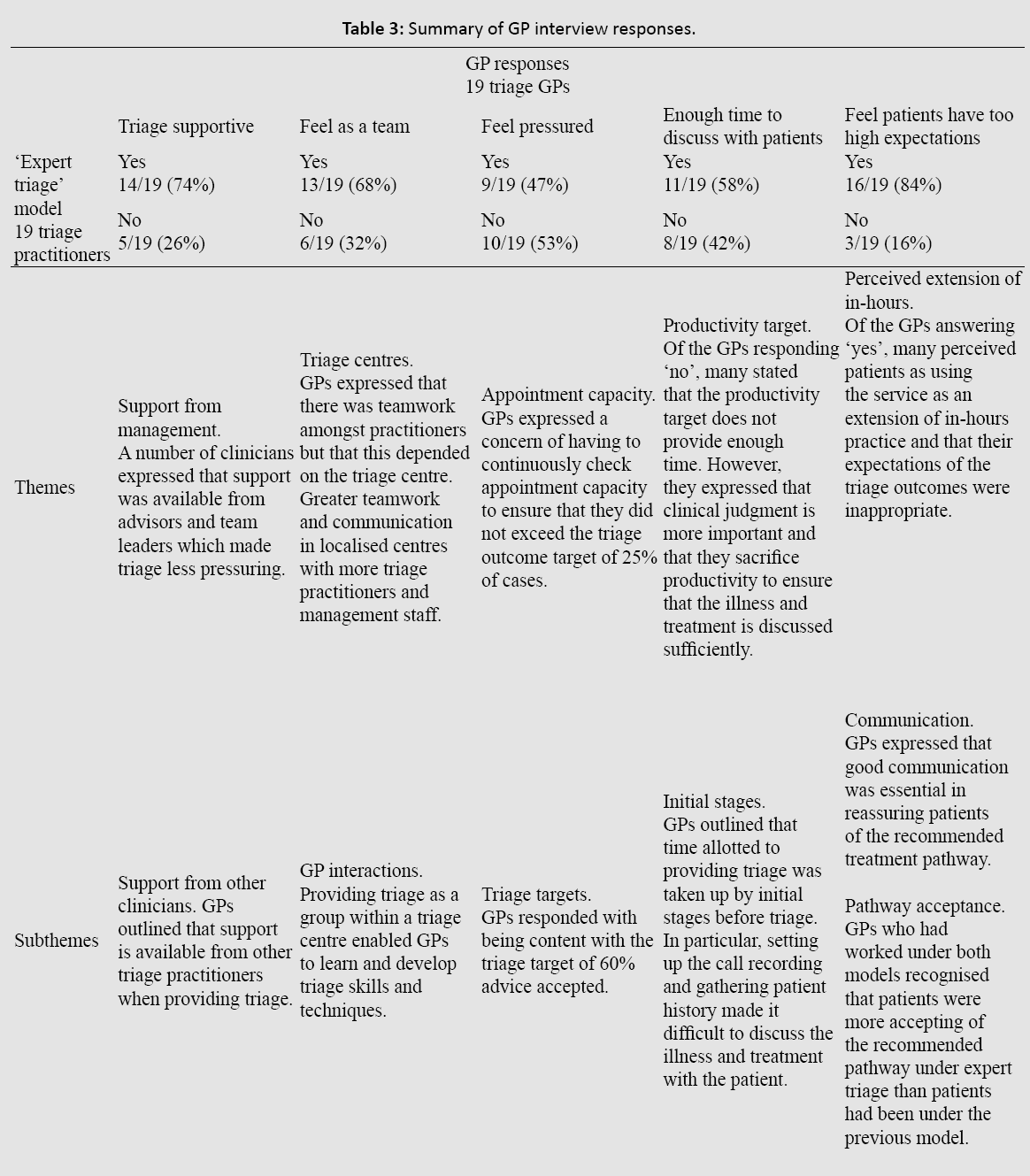
GP experiences
GPs now providing the service gave generally positive views about the new model of out-of-hours care. The service change was felt to have helped to address the challenges associated with the previous model, in particular triage delays, capacity and quality (“Triage has got better since the new system. More doctors triaging has made it easier”; “I’ve seen a change in patient expectations since the new model, I was seeing a lot of patients that did not need to be seen before”). The triage environment was perceived as supportive; a result of effective training (though which could be improved further) (“Having people in the same place is more supportive, I can talk to other doctors”; “There are other GPs around to talk to and ask their opinion. You gain tips from listening to other GPs”). A theme of responses was that GPs felt pressurised to achieve targets of telephone advice conclusions (9/19), and that they would value more time to discuss matters with patients (“When patients have high expectations it is difficult to ignore. More time is needed to persuade and reassure”). However, a subtheme of responses outlined that GPs were mainly content with the 60% telephone advice target, with a range from 40-60% in terms of what they felt was an appropriate target. Most GPs (16/19) felt that patients had (too) high expectations of the service (“Patients need to be educated of what the out-of-hours service is for; it is not an extension of in-hours”), although a subtheme of responses reflected negotiation and reassurance being possible, and that patients were generally accepting of the new model and advice given. Overall they identified potential further improvements that could be achieved through patient education, call handler and GP training, analysis and feedback on triage performance, implementing Clinical Professional Development and increasing consultation times for complex cases.
Summary
Triage outcomes changed from before to after the introduction of the ‘expert triage’ model of out-of-hours service delivery, with greater proportions of calls concluded with telephone advice and fewer patients being seen at out-of-hours centres and A&E centres. These changes were sustained for fifteen months. Patient interview responses indicated that the proportion of patients who used the triage advice given remained constant after introduction of ‘expert triage’ although there was some indication of less understanding of telephone advice, more disagreement with the triage recommendation, and greater intentions to use another service under expert triage. Clinicians reported perceived improvements in triage delays, capacity and quality, and that they did not feel overly pressurised by the triage outcome targets. Improvement suggestions included further public education about appropriate use of services, management of patient expectations, and further recruitment and training for triage practitioners and call handlers.
Strengths and Weaknesses
This study complemented activity-based triage outcomes with interviews to assess service user and provider experience of these service changes. Participants elaborated on responses and made suggestions about how the service could be improved based on their experiences. However, patient interviews lasted an average of 5 minutes which also restricted the length of elaboration. Although interviews with triage providers lasted for 30 to 45 minutes, it enabled a large amount of data to be gathered from each provider. Subject to recall bias possibilities, the responses from both triage users and providers are likely applicable to other services whose aim is to overcome challenges associated with pressures from patient expectations and demand for face-to-face appointments.
An important caution is that influences on A&E usage are not available, only the recommendation about whether to use A&E services. Furthermore, the safety of triage outcome pathways was not followed up; the change in triage outcomes may not have been optimal for patient safety. A weakness of the study is that patients from the ‘previous’ service model took part in interviews, on average, four months after they had used the service, making recall perhaps more variable in this group. Context of other literature Triage outcomes changed following the implementation of the ‘expert triage’ model with fewer patients being given primary care centre appointments and referrals to A&E centres. Patients had similar use of triage advice although greater disagreement with the triage outcome. Furthermore, patients and GPs who experienced both service models perceived improvements in triage delays and quality. Changes to out-of-hours services have been shown elsewhere to influence presentation rates in emergency centres.⁹ Perhaps in contrast to the recommendations for A&E usage in this study, however, Thompson et al. found that triage by appropriate clinicians increased the proportion of patients attending emergency care departments for non-trauma conditions, especially during overnight periods.[9] Elsewhere, evaluation of other out-of-hours organisational models has found telephone triage to be favourable for patient accessibility and satisfaction but less favourable from clinician satisfaction perspectives².
The present study supports those patient accounts identified, although in contrast, triage GP satisfaction was also high with only a few suggestions for improvement.
An issue identified with the present study was that safety of triage outcomes was not analysed. Although there have been a number of safety evaluations of out-of-hours triage revealing that telephone triage is generally a safe practice. Huibers et al. conducted a review of telephone triage and found triage to be safe for 97% of patients who contacted services. [10]Of the studies reporting adverse events just below half reported mortality, medical errors and hospitalisations¹º. In an evaluation of the Manchester Triage System which aimed to reduce the number of patients classed as urgent, triage identified less urgent patients safely and resulted in low hospitalisation following discharge for most patient groups. [11]
Among UK health service users, understanding that health resources are limited and that others may perhaps have greater needs is variable.[12] There was evidence of concern about appropriate use of health services, and patients reporting that they had consciously limited their own service use because they worried that they were “wasting clinician time”.[12] Discrepancy between patients’ expectations and GP recommendations is evident in previous literature. [12-14]
With mixed effects on patient satisfaction and enablement, Brown et al. found that patients who received advice other than that expected were still satisfied with the telephone triage, whereas Egbunike et al. found that patient expectations moderated the relationship between user concern and satisfaction with a greater intention to re-consult with the same service for the same illness episode. [13,14] In this study both patients and triage GPs were concerned about the expectations or perspective of the other, but patient agreement with the assessment recommendation was suboptimal. In line with this, Brown identified the importance of patient trust, finding effective communication of warmth, openness and understanding of the patient’s interests were the most effective strategies in upholding trust. [15] Findings from the present study, that patients were not fully accepting of the recommended treatment pathway under the ‘expert triage’ model, may suggest that patient trust and confidence in the triage process need to be further improved.
Implications for practice and research
The before and after comparisons in this study show that the ‘expert triage’ model has had an appreciable impact on this service, with fewer face-to-face consultations and more telephone advice concluding calls, less perceived delay in triage call back and in providing appointments, and encouragement of patients to use their in-hours practice. A concern from service providers that there would be a rise in complaints from patients, or GP in-hours and A&E providers about diverted demand, was not borne out. It also encouraged the return of nine doctors to the out-of-hours service (among a total of 40). Continued and wider adoption of the ‘expert triage’ model in out -of-hours services may lead to a decline in service pressures for the out-of-hours services, although impact on in-hours primary care and A&E services require evaluation. Findings from both service users and service providers were that patients have high, and sometimes inappropriate, expectations of the nature of the service and use of assessment pathways. This may provide a possible explanation as to why slightly fewer patients indicated understanding telephone advice under the new model; they did not agree with this treatment pathway and were therefore reluctant to utilize the information. Greater patient education about appropriate service use, for quality and safety purposes, is necessary, and findings in this study indicate that there would be patient and public support for such initiatives. In addition, this study evaluated the Cardiff & Vale out-of-hours service for a short time after the ‘expert triage’ model was implemented. Further research would benefit from longer term assessment of the impact of the service model on quality, safety, and patient and clinician experiences both in this location and if adopted further afield. Further evaluation should also use more detailed methods to assess patient experiences, including mixed methods approaches and with larger samples, to understand both the experiences in more depth and also the influences on help-seeking behaviour across the whole system of unscheduled care. Further research should also focus specifically on the quality and safety of telephone triage.
Adoption of the ‘expert triage’ model for this out-of-hours service has led to an increase in proportion of calls concluded by telephone advice instead of face-to-face consultations. As such the perceived associated improvements in triage and consultation delays, service quality, and positive experiences for participating clinicians, alongside largely maintained service user experiences, warrant continued implementation of this model of out-of-hours care. Caution and further evaluation of the effects on other primary care services is required, as are further improvements to address service users’ suggestions and to enhance public understanding and expectations.
We thank the staff at Cardiff & Vale Primary Care Division for assistance with patient and GP recruitment, and provision and interpretation of statistical data. We also thank the patients and triage GPs who provided responses.
Internal from Cardiff & Vale Primary Care Division for a studentship 10.
This was a service evaluation of a quality improvement project; therefore, no ethical approval was required.